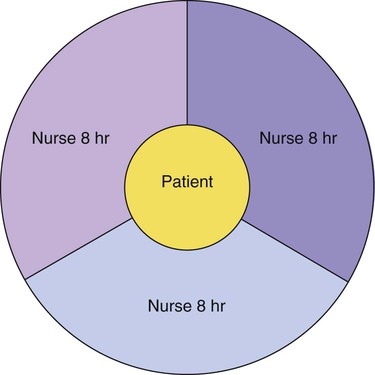
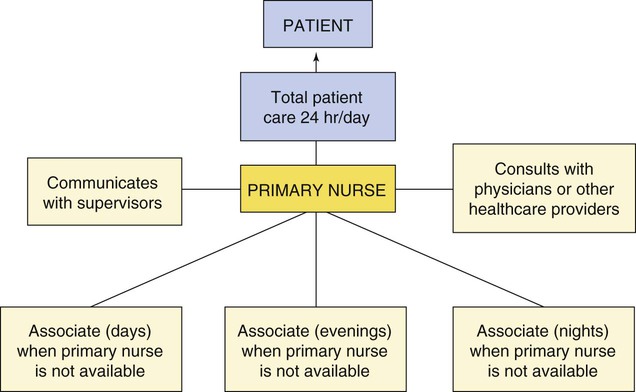
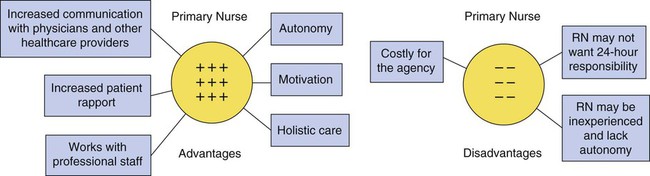
• Differentiate the characteristics of nursing care delivery models used in health care. • Determine the role of the nurse manager and the staff nurse in each model. • Describe the implementation of a disease-management program. • Summarize the differentiated nursing practice model and related methods to determine competencies of nurses who deliver care. • Consider the impact of “transforming care at the bedside” (TCAB) on the delivery of care in a specific nursing unit. During an 8- or 12-hour shift, the patient receives consistent care from one nurse. The nurse, patient, and family usually trust one another and can work together toward specific goals. Usually, the care is patient-centered, comprehensive, continuous, and holistic. But the nurse may choose to deliver this care with a task orientation that negates the holistic perspective (Tiedeman & Lookinland, 2004). Because the nurse is with the patient during most of the shift, even subtle changes in the patient’s status are easily noticed (Figure 13-1). In today’s costly healthcare economy, total patient care provided by a registered nurse (RN) is very expensive. Is it realistic to use the highly skilled and extremely knowledgeable professional nurse to provide all the care required in a unit that may have 20 to 30 patients? Who oversees the care coordination in a 24-hour period (Tiedeman & Lookinland, 2004)? In times of nursing shortages, there may not be enough resources or nurses to use this model. In the case method, the staff RN provides holistic care to a group of patients during a defined work time. The physical, emotional, and technical aspects of care are the responsibility of the assigned RN. This model is especially useful in the care of complex patients who need active symptom management provided by an RN, such as the care of the patient in a hospice setting or an intensive care unit. This care delivery model requires the nurse who is assigned to total patient care to complete the complex functions of care, such as assessment and teaching the patient and family, as well as the less complex functional aspects of care, such as personal hygiene. Some nurses find satisfaction with this model of care because no aspect of nursing care is delegated to another, thus eliminating the need for supervision of others (Tiedeman & Lookinland, 2004). The functional model of nursing is a method of providing patient care by which each licensed and unlicensed staff member performs specific tasks for a large group of patients. These tasks are in part determined by the scope of practice defined for each type of caregiver. For example, the RN must be responsible for all assessments, although the LPN/LVN and UAPs may collect data that can be used in the assessment. Regarding treatments, an RN may administer all intravenous (IV) medications and do admissions, one LPN/LVN may provide treatments, another LPN/LVN may give all oral medications, one assistant may do all hygiene tasks, and another assistant may take all vital signs (Figure 13-2). This division of aspects of care is similar to the assembly line system used by manufacturing industries. Just as an auto worker becomes an expert in attaching fenders to a new vehicle, the staff nurse becomes expert in the tasks expected in functional nursing. A charge nurse coordinates care and assignments and may ultimately be the only person familiar with all the needs of any individual patient. Although financial savings may be the impetus for organizations to choose the functional system of delivering care, the disadvantages may outweigh the savings (Figure 13-3). A major disadvantage is the fragmentation of care. The physical and technical aspects of care may be met, but the psychological and spiritual needs may be overlooked. Patients become confused with so many different care providers per shift. These different staff members may be so busy with their assigned tasks that they may not have time to communicate with each other about the patient’s progress. Because no one care provider sees patient care from beginning to end, the patient’s response to care is difficult to assess. Critical changes in patient status may go unnoticed. Fragmented care and ineffective communication can lead to patient and family dissatisfaction and frustration. Exercise 13-2 provides an opportunity to imagine how a patient would react to the functional method and also to imagine how the nurse may feel. In team nursing, a team leader is responsible for coordinating a group of licensed and unlicensed personnel to provide patient care to a small group of patients. The team leader should be a highly skilled leader, manager, and practitioner, who assigns each member specific responsibilities according to role, licensure, education, ability, and the complexity of the care required. The members of the team report directly to the team leader, who then reports to the charge nurse or unit manager (Figure 13-4). There are several teams per unit, and patient assignments are made by each team leader. The team method of patient care delivery has one major disadvantage, which arises if the team leader has poor leadership skills. The team leader must have excellent communication skills, delegation and conflict management abilities, strong clinical skills, and effective decision-making abilities to provide a working “team” environment for the members. The team leader must be sensitive to the needs of the patient and, at the same time, attentive to the needs of the staff providing the direct care (Moore, 2004). When the team leader is not prepared for this role, the team method becomes a miniature version of the functional method and the potential for fragmentation of care is high. The nurse manager, charge nurse, and team leaders must have management skills to effectively implement the team nursing method of patient care delivery. In addition, the nurse manager must determine which RNs are skilled and interested in becoming a charge nurse or team leader. Because the basic education of baccalaureate-prepared RNs emphasizes critical-thinking and leadership concepts, they are likely candidates for such roles. The nurse manager should also provide an adequate staff mix and orient team members to the team nursing system by providing continuing education about leadership, management techniques, delegation, and team interaction (see Chapters 1, 3, 4, 18, and 26). By addressing these factors, the manager is aiding the teams to function optimally. Primary nursing, an adaptation of the case method, was developed by Marie Manthey as a method for organizing patient care delivery in which one RN functions autonomously as the patient’s primary nurse throughout the hospital stay (Manthey, Ciske, Robertson, & Harris, 1970). Primary nursing brought the nurse back to direct patient care. The primary nurse is accountable for the patients’ care 24 hours a day from admission through discharge. Conceptually, primary nursing care provides the patient and the family with coordinated, comprehensive, continuous care (Tiedeman & Lookinland, 2004). Care is organized, using the nursing process. The primary nurse collaborates, communicates, and coordinates all aspects of patient care with other nurses as well as other disciplines (Tiedeman & Lookinland, 2004). Advocacy and assertiveness are desirable leadership attributes for this care delivery model. The primary nurse, preferably at least baccalaureate-prepared, is held accountable for meeting outcome criteria and communicating with all other healthcare providers about the patient (Figure 13-5). For example, a patient is admitted to a medical unit with pulmonary edema. His primary nurse admits him and then provides a written plan of care. When his primary nurse is not working, an associate nurse implements the plan. The associate nurse is an RN who has been delegated to provide care to the patient according to the primary nurse’s specification. If the patient develops additional complications, the associate nurse notifies the primary nurse, who has 24-hour accountability and responsibility. The associate nurse provides input to the patient’s plan of care, and the primary nurse makes the appropriate alterations. Tiedeman and Lookinland (2004) cited numerous works that speak to the quality of care and patient satisfaction with primary care. Some studies cited in their work speak to increased quality of care and patient satisfaction, whereas others find no difference in these parameters when compared with team nursing. RNs practicing primary nursing must possess a broad knowledge base and have highly developed nursing skills. In this system of care delivery, professionalism is promoted. Nurses experience job satisfaction because they can use their education to provide holistic and autonomous care for the patient. This high level of accountability for patient outcomes encourages RNs to further their knowledge and refine skills to provide optimal patient care. If the primary nurse is not motivated or feels unqualified to provide holistic care, job satisfaction may decrease. A professional advantage to the primary nursing method is a decrease in the number of unlicensed personnel. The ideal primary nursing system requires an all-RN staff. The RN can provide total care to the patient, from bed baths to patient education, even both at the same time! Unlicensed personnel are not qualified to provide this level of inclusive care (Figure 13-6).
Care Delivery Strategies
Case Method (Total Patient Care)
Model Analysis
Staff RN’s Role
Functional Nursing
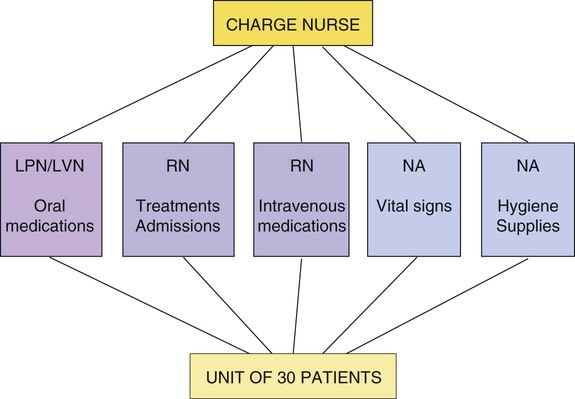
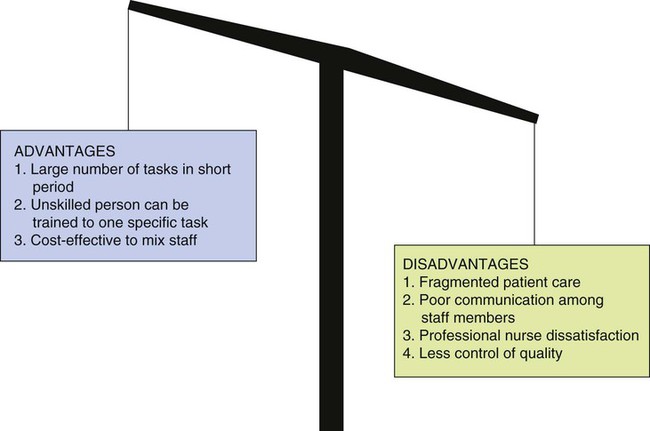
Model Analysis
Team Nursing
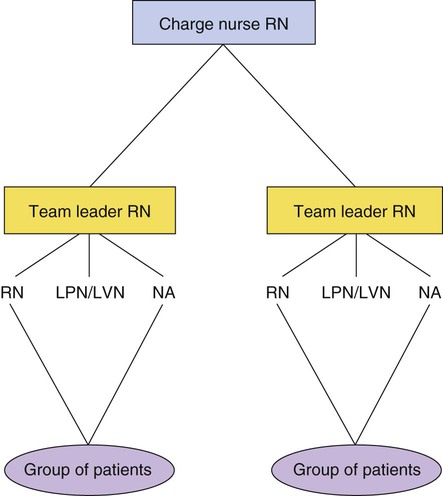
Model Analysis
Nurse Manager’s Role
Primary Nursing
Model Analysis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access