Bowel Elimination
Objectives
• Define the key terms and key abbreviations in this chapter.
• Describe normal defecation and the observations to report.
• Identify the factors affecting bowel elimination.
• Explain how to promote comfort and safety during defecation.
• Describe the common bowel elimination problems.
• Explain why enemas are given.
• Describe the common enema solutions.
• Describe the rules for giving enemas.
• Describe how to care for a person with an ostomy.
• Perform the procedures described in this chapter.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Key Abbreviations
| BM | Bowel movement |
| CMS | Centers for Medicare & Medicaid Services |
| GI | Gastro-intestinal |
| ID | Identification |
| IV | Intravenous |
| mL | Milliliter |
| oz | Ounce |
| SSE | Soapsuds enema |
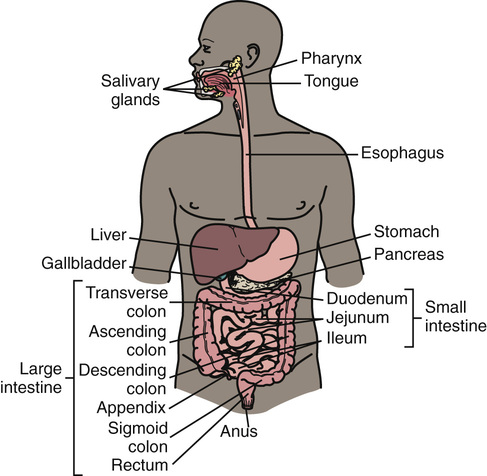
Bowel elimination is a basic physical need. Wastes are excreted from the gastro-intestinal (GI) system (Chapter 10). Many factors affect bowel elimination—privacy, habits, age, diet, exercise and activity, fluids, drugs, disability. Problems easily occur. Normal bowel elimination is important. You assist patients and residents to meet elimination needs.
See Body Structure and Function Review: The Gastro-Intestinal Tract.
See Delegation Guidelines: Bowel Elimination.
See Promoting Safety and Comfort: Bowel Elimination.
Normal Bowel Elimination
Some people have a bowel movement (BM) every day. Others do so every 2 to 3 days. Some people have 2 or 3 BMs a day. Many people have a BM after breakfast. Others do so in the evening.
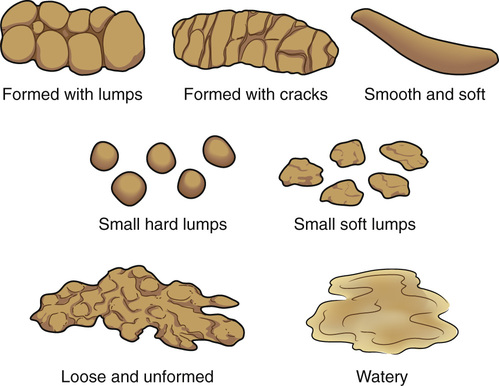
Stools are normally brown. Bleeding in the stomach and small intestine causes black or tarry stools. Bleeding in the lower colon and rectum causes red-colored stools. So do beets, tomato juice or soup, red Jell-O, and foods with red food coloring. Green vegetables can cause green stools. Diseases and infection can cause clay-colored or white, pale, orange-colored, or green-colored stools and stools with mucus. Figure 26-2, p. 424 shows a color chart for stools.

Stools are normally soft, formed, moist, and shaped like the rectum. They have a normal odor caused by bacteria in the intestines. Certain foods and drugs also cause odors.
See Focus on Children and Older Persons: Normal Bowel Elimination, p. 424.
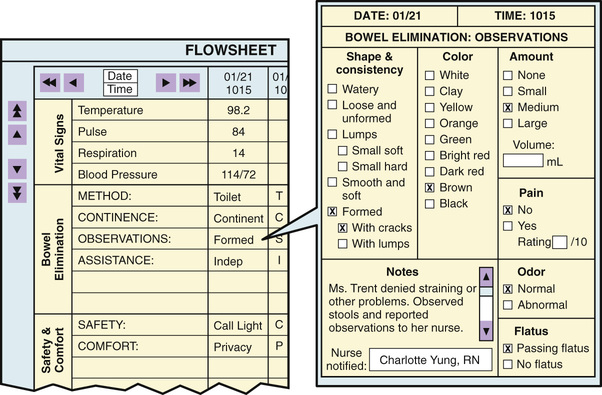
Observations
Your observations are used for the nursing process. Ask the nurse to observe abnormal stools. Report and record the following.
See Focus on Communication: Observations.
Factors Affecting BMs
These factors affect BM frequency, consistency, color, and odor. They are part of the nursing process to meet the person’s elimination needs. Normal, regular elimination is the goal.
• Diet—high-fiber foods. High-fiber foods leave a residue for needed bulk to prevent constipation (p. 426). Fruits, vegetables, and whole-grain cereals and breads are high in fiber. Many people do not eat enough fruits and vegetables. Some cannot chew these foods. They may not have teeth. Or dentures fit poorly. Some people think that they cannot digest fruits and vegetables. So they refuse to eat them. Sometimes bran is added to cereal, prunes, or prune juice.
• Drugs. Drugs can prevent constipation or control diarrhea. Other drugs have diarrhea or constipation as side effects. Pain-relief drugs often cause constipation. Antibiotics (used to fight or prevent infections) often cause diarrhea. Diarrhea occurs when the antibiotics kill normal flora in the colon. Normal flora is needed to form feces. (See “Normal Flora” in Chapter 16.)
• Disability. Some people cannot control BMs. They have a BM whenever feces enter the rectum. A bowel training program is needed (p. 430).
See Focus on Children and Older Persons: Factors Affecting BMs.
Safety and Comfort
The care plan has measures for meeting elimination needs. It may involve diet, fluids, and exercise. The measures in Box 26-1 promote safety and comfort.
See Focus on Communication: Safety and Comfort.
See Teamwork and Time Management: Safety and Comfort.
Common Problems
Common problems include constipation, fecal impaction, diarrhea, fecal incontinence, and flatulence.
Constipation
Constipation is the passage of a hard, dry stool. The person strains to have a BM. Stools are large or marble-sized. Large stools cause pain as they pass through the anus. Constipation occurs when feces move slowly through the bowel. This allows more time for water absorption. Common causes of constipation include:
Diet changes, fluids, and activity prevent or relieve constipation. The doctor may order 1 or more of the following.
 Fecal Impaction
Fecal Impaction
A fecal impaction is the prolonged retention and buildup of feces in the rectum. Feces are hard or putty-like. Fecal impaction results if constipation is not relieved. The person cannot have a BM. More water is absorbed from the already hard feces. Liquid feces pass around the hardened fecal mass in the rectum and seep from the anus.
The person tries many times to have a BM. Abdominal discomfort, abdominal distention (swelling), nausea, cramping, and rectal pain are common. Older persons may have poor appetite or confusion. Some persons have a fever. Report such signs and symptoms to the nurse.
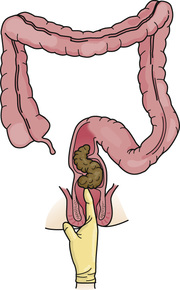
The nurse does a digital (finger) exam to check for an impaction. A lubricated, gloved finger is inserted into the rectum to feel for a hard mass in the lower rectum (Fig. 26-5). Sometimes it is out of reach higher in the colon. The digital exam often causes the urge to have a BM. The doctor may order drugs, suppositories, or enemas to remove the impaction.
Sometimes digital removal of an impaction is done. A lubricated, gloved finger is hooked around a piece of feces. Then the finger and feces are removed. The stool is dropped into the bedpan. The process is repeated as needed. The procedure can be uncomfortable and embarrassing.
Checking for and removing impactions are very dangerous. The vagus nerve can be stimulated. Stimulation of the vagus nerve slows the heart rate. The heart rate can slow to unsafe levels in some persons.
See Focus on Long-Term Care and Home Care: Fecal Impaction.
See Delegation Guidelines: Fecal Impaction.
See Promoting Safety and Comfort: Fecal Impaction.
See procedure: Checking For and Removing a Fecal Impaction, p. 428.
Diarrhea
Diarrhea is the frequent passage of liquid stools. Feces move through the intestines rapidly. This reduces the time for fluid absorption. The need for a BM is urgent. Some people cannot get to a bathroom in time. Abdominal cramping, nausea, and vomiting may occur.
Causes of diarrhea include infections, some drugs, irritating foods, and microbes in food and water. Diet and drugs are ordered to reduce peristalsis. You need to:
• Assist with elimination needs promptly.
• Dispose of stools promptly. This prevents odors and the spread of microbes.
Fluid lost through diarrhea must be replaced to prevent dehydration. Dehydration is the excessive loss of water from tissues. The person has pale or flushed skin, dry skin, and a coated tongue. Urine is dark and scant in amount (oliguria). Thirst, weakness, dizziness, and confusion also occur. Falling blood pressure and increased pulse and respirations are serious signs. Death can occur. The nursing process is used to meet fluid needs. The doctor may order IV (intravenous) fluids in severe cases (Chapter 28).
Microbes can cause diarrhea. Preventing the spread of infection is important. Always follow Standard Precautions and the Bloodborne Pathogen Standard when in contact with stools.
See Focus on Children and Older Persons: Diarrhea.
See Promoting Safety and Comfort: Diarrhea.