Basic Emergency Care
Objectives
• Define the key terms and key abbreviations in this chapter.
• Describe the rules of emergency care.
• Identify the signs of cardiac arrest and the emergency care required.
• Describe emergency care for poisoning.
• Describe emergency care for hemorrhage, fainting, and shock.
• Describe emergency care for stroke.
• Explain how to care for a person during a seizure.
• Describe emergency care for concussions.
• Describe emergency care for burns.
• Perform the procedures described in this chapter.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Key Abbreviations
| AED | Automated external defibrillator |
| AHA | American Heart Association |
| BLS | Basic Life Support |
| CPR | Cardiopulmonary resuscitation |
| ECC | Emergency Cardiovascular Care |
| EMS | Emergency Medical Services |
| MET | Medical Emergency Team |
| RRT | Rapid Response Team |
| SCA | Sudden cardiac arrest |
| VF; V-fib | Ventricular fibrillation |
Emergencies can occur anywhere. Sometimes you can save a life if you know what to do. First aid and Basic Life Support (BLS) courses prepare you to give emergency care.
The BLS procedures in this chapter are given as basic information. They do not replace certification training. You need a BLS course for health care providers.
BLS guidelines are updated as new information becomes available. You are responsible for following current guidelines. Emergency Cardiovascular Care (ECC) updates can be found on-line at ECCguidelines.heart.org.
Emergency Care
First aid is the emergency care given to an ill or injured person before medical help arrives. The goals of first aid are to:
In an emergency, the Emergency Medical Services (EMS) system is activated. Emergency personnel (paramedics, emergency medical technicians) rush to the scene. They treat, stabilize, and transport persons with life-threatening problems. They have guidelines for care and communicate with doctors in hospital emergency rooms. The doctors can direct their care. Their ambulances have emergency drugs, equipment, and supplies. To activate the EMS system, do 1 of the following.
Each emergency is different. The rules in Box 54-1 apply to any emergency. Hospitals and other agencies have procedures for emergencies. Rapid Response Teams (RRTs) or Medical Emergency Teams (METs) are called when a person shows warning signs of a life-threatening condition. An RRT (MET) may include a doctor, a nurse, and a respiratory therapist. The RRT’s (MET’s) goal is to prevent death.
See Focus on Communication: Emergency Care.
See Focus on Long-Term Care and Home Care: Emergency Care.
See Promoting Safety and Comfort: Emergency Care.
BLS for Adults
When the heart and breathing stop, the person is clinically dead. Blood is not circulated through the body. Heart, brain, and other organ damage occurs within minutes. The American Heart Association’s (AHA’s) BLS procedures support circulation and breathing.
Sudden Cardiac Arrest
Sudden cardiac arrest (SCA) or cardiac arrest is when the heart stops suddenly and without warning. Within moments, breathing stops as well. Permanent brain and other organ damage occurs unless circulation and breathing are restored. There are 3 major signs of SCA.
The person’s skin is cool, pale, and gray. The person is not coughing or moving.
SCA is a sudden, unexpected, and dramatic event. It can occur anywhere and at any time—while driving, shoveling snow, playing golf or tennis, watching TV, eating, or sleeping. Common causes include heart disease, heart attack, enlarged heart, heart valve problems, dysrhythmias (arrhythmias), and congenital heart defects (Chapter 45). Electrical shock, chest trauma, and illegal drug use are other causes. These causes lead to an abnormal heart rhythm called ventricular fibrillation (p. 835). The heart cannot pump blood. A normal rhythm must be restored. Otherwise the person will die.
Chains of Survival.
The AHA’s BLS courses teach Chains of Survival. The Chains of Survival identify the different pathways of care for in-hospital and out-of-hospital cardiac arrests (Box 54-2). Care is provided as soon as possible. Any delay reduces the person’s chance of surviving.
See Focus on Communication: Chains of Survival.
Respiratory Arrest
Respiratory arrest is when breathing stops but heart action continues for several minutes. If breathing is not restored, cardiac arrest occurs. Respiratory arrest can occur from:
• Problems affecting nerves, muscles, or areas of the brain that control breathing—amyotrophic lateral sclerosis (ALS), spinal cord injuries, stroke (Chapter 44); drug or alcohol over-dose; drug side-effects
• Damage to the lungs—injury to the chest
• Lung disorders and problems—pneumonia, chronic obstructive pulmonary disease (Chapter 45), pulmonary embolism (Chapter 35)
• Blocked airflow—choking (Chapter 13 and p. 844), drowning, suffocation
Rescue Breathing.
Rescue breaths are given when there is a pulse but no breathing or only agonal gasping. To give rescue breaths:
• Give 1 breath every 5 to 6 seconds for adults.
• Give 1 breath every 3 to 5 seconds for infants and children.
• Give each breath over 1 second. The chest should rise when breaths are given.
• Check the pulse every 2 minutes. If there is no pulse, begin CPR. If the pulse is 60 or less in an infant or child, begin CPR (p. 839).
Adult CPR
When the heart and breathing stop, blood and oxygen are not supplied to the body. Brain and other organ damage occurs within minutes.
CPR must be started at once when a person has SCA. CPR supports circulation and breathing. It provides blood and oxygen to the heart, brain, and other organs until advanced emergency care is given. CPR involves:
CPR procedures require speed, skill, and efficiency.
See Promoting Safety and Comfort: Adult CPR, p. 832.
Chest Compressions.
The heart, brain, and other organs must receive blood. Otherwise, permanent damage results. In cardiac arrest, the heart has stopped beating. Blood must be pumped through the body another way. Chest compressions force blood through the circulatory system.
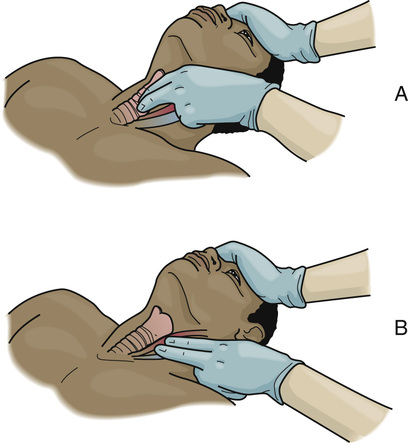
Before starting chest compressions, check for a pulse. Use the carotid artery on the side near you. To find the carotid pulse, place 2 or 3 fingertips on the trachea (windpipe). Then slide your fingers down off the trachea to the groove of the neck (Fig. 54-1). Check for a pulse for no more than 10 seconds. While checking for a pulse, look for signs of circulation. See if the person has started breathing or is coughing or moving.
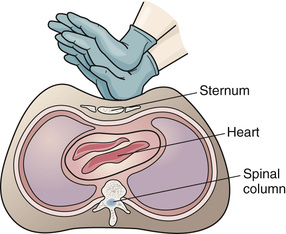
The heart lies between the sternum (breastbone) and the spinal column. When pressure is applied to the sternum, the sternum is depressed (moved down). This compresses the heart between the sternum and spinal column (Fig. 54-2). For effective chest compressions, the person must be supine on a hard, flat surface—floor or back-board. You are positioned at the person’s side.
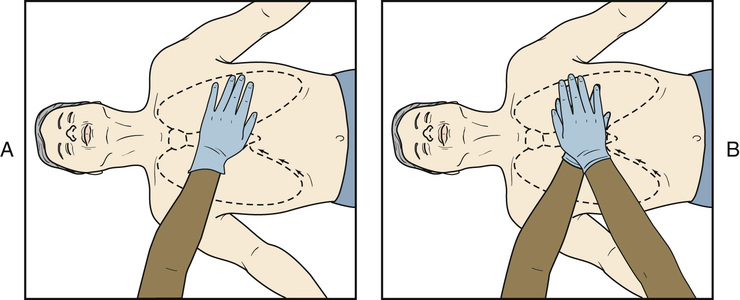
Hand position is important for effective chest compressions (Fig. 54-3). You use the heels of your hands—1 on top of the other—for chest compressions. For proper placement:
To give chest compressions, your arms are straight. Your shoulders are directly over your hands. And your fingers are interlocked (Fig. 54-4). Exert firm downward pressure to depress the average adult sternum at least 2 inches. According to AHA guidelines, avoid pressing down more than 2.4 inches. Then release pressure without removing your hands from the chest. Avoid leaning on the chest between compressions. Releasing pressure allows the chest to recoil—to return to its normal position. Recoil lets the heart fill with blood.
The AHA recommends that you:
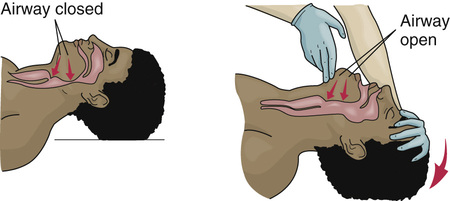
Airway.
The respiratory passages (airway) must be open to restore breathing. The airway is often obstructed (blocked) during SCA. The person’s tongue falls toward the back of the throat and blocks the airway. The head tilt–chin lift method opens the airway (Fig. 54-5).
• Place the palm of 1 hand on the forehead.
• Tilt the head back by pushing down on the forehead with your palm.
• Lift the jaw. This brings the chin forward.
• Do not close the person’s mouth. The mouth should be slightly open.
Breathing.
Air is not inhaled when breathing stops. The person must get oxygen. If not, permanent heart, brain, and other organ damage occurs. The person is given breaths. That is, a rescuer inflates the person’s lungs.
Each breath should take 1 second. You should see the chest rise with each breath. Two breaths are given after every 30 chest compressions.
See Focus on Children and Older Persons: Breathing.
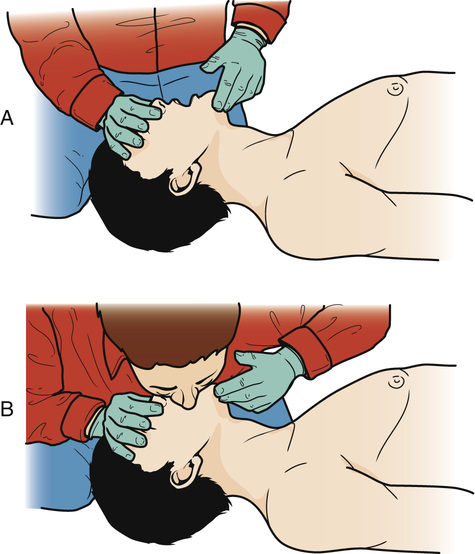
Mouth-to-Mouth Breathing.
Mouth-to-mouth breathing (Fig. 54-6) is one way to give breaths. You place your mouth over the person’s mouth. Contact with the person’s blood, body fluids, secretions, or excretions is likely. To give mouth-to-mouth breathing:
1. Keep the airway open with the head tilt–chin lift method.
3. Take a breath. A regular breath is needed, not a deep breath.
4. Place your mouth tightly over the person’s mouth. Seal the mouth with your lips.
5. Blow air into the person’s mouth. You should see the chest rise as the lungs fill with air.
6. Repeat the head tilt–chin lift method if the chest did not rise.
7. Remove your mouth from the person’s mouth. Then take in a quick breath.
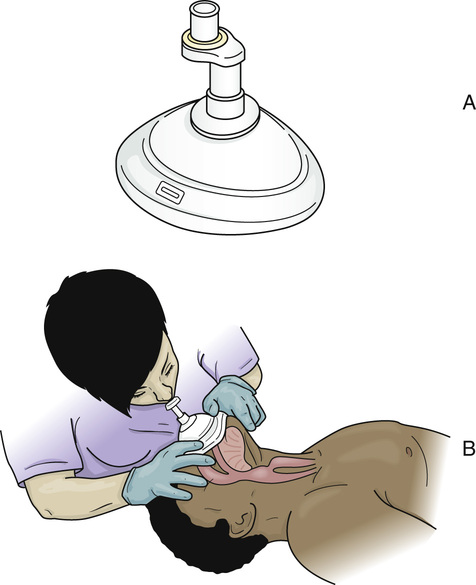
Barrier Device Breathing.
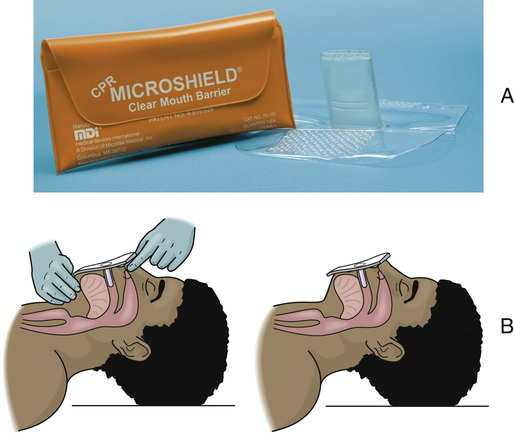
A barrier device is used for giving breaths whenever possible. The device prevents contact with the person’s mouth and blood, body fluids, secretions, or excretions. A face shield may be used (Fig. 54-7). A face shield is replaced with a face mask as soon as possible (Fig. 54-8, A). The mask is placed over the person’s mouth and nose (Fig. 54-8, B). When using a barrier device, seal the device against the person’s face. The seal must be tight. Then open the airway with the head tilt–chin lift method.
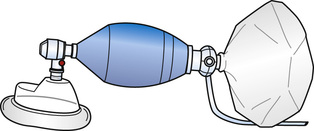
A bag valve mask (Fig. 54-9) is another device used to give rescue breaths. The device consists of a hand-held bag attached to a mask. The mask is held securely to the person’s face. The bag is squeezed to give breaths. The bag can be connected to an oxygen source.
Mouth-to-Nose Breathing.
Mouth-to-nose breathing is used when:
• You cannot breathe through the person’s mouth.
• Your mouth is too small to make a tight seal for mouth-to-mouth breathing.
• The mouth or jaw is severely injured.
The mouth is closed for mouth-to-nose breathing. The head tilt–chin lift method opens the airway. Pressure is placed on the chin to close the mouth. To give a breath, place your mouth over the person’s nose and blow air into the nose (Fig. 54-10). After giving a breath, remove your mouth from the person’s nose.

Mouth-to-Stoma Breathing.
Some people breathe through stomas (openings) in their necks (Fig. 54-11). To give mouth-to-stoma breathing:
1. Keep the person’s mouth closed.
2. Do not tilt the person’s head back.
3. Seal your mouth around the stoma.
If the person’s chest does not rise, you may need to pinch the nostrils shut.

Before giving mouth-to-mouth or mouth-to-nose breathing, always check to see if the person has a stoma. Other rescue breathing methods are not effective if the person has a stoma.
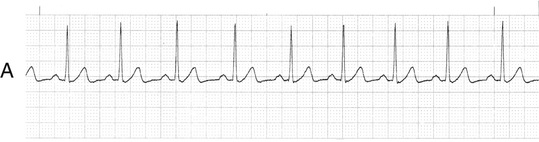
Defibrillation.
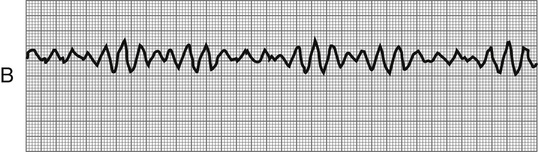
Ventricular fibrillation (VF, V-fib) is an abnormal heart rhythm (Fig. 54-13, p. 836). It causes sudden cardiac arrest. Rather than beating in a regular rhythm, the heart shakes and quivers like a bowl of Jell-O. The heart does not pump blood. The heart, brain, and other organs do not receive blood and oxygen.
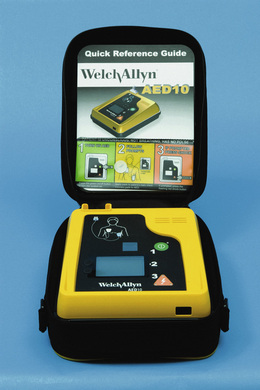
A defibrillator is used to deliver a shock to the heart. The shock stops the VF (V-fib). This allows the return of a regular heart rhythm. Defibrillation as soon as possible after the onset of VF (V-fib) increases the person’s chance of survival.
For adults, the AHA recommends that rescuers:
• Use an AED as soon as possible.
• Give 1 shock. Then resume CPR at once. Begin with chest compressions.
• Check for a heart rhythm again after about 2 minutes of CPR (when prompted by the AED).
AEDs are found in health care agencies (Fig. 54-14, p. 836). They are on airplanes and in airports, health clubs, malls, and other public places. Some people have them in their homes.
You will learn more about using an AED in the AHA’s BLS for Healthcare Providers course.
See Focus on Children and Older Persons: Defibrillation, p. 836.
 Performing Adult CPR.
Performing Adult CPR.
CPR is done only for cardiac arrest. You must determine if cardiac arrest or fainting (p. 845) has occurred. CPR is done if the person does not respond, is not breathing or only gasping (has no normal breathing ), and has no pulse.
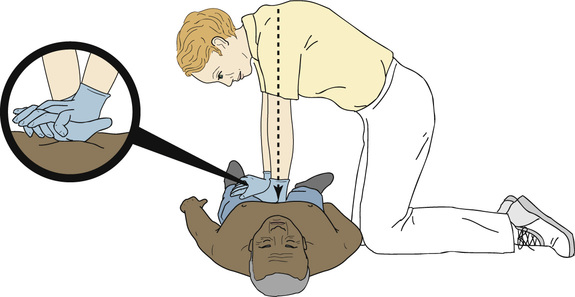
CPR is done alone or with another person. When done alone, chest compressions and breaths are given by 1 rescuer. With 2 rescuers, 1 person gives chest compressions and the other gives breaths (Fig. 54-15). Rescuers switch tasks about every 2 minutes to avoid fatigue and inadequate compressions. The second rescuer uses the AED if one is available.

See Focus on Communication: Performing Adult CPR.
See Promoting Safety and Comfort: Performing Adult CPR.
See procedure: Adult CPR—1 Rescuer.
See procedure: Adult CPR With AED—2 Rescuers.
Basic Life Support guidelines are updated as new information becomes available. You are responsible for following current guidelines. Updates can be found on-line at ECCguidelines.heart.org.