Assisting in Cardiology
Learning Objectives
1. Define, spell, and pronounce the terms listed in the vocabulary.
2. Apply critical thinking skills in performing the patient assessment and patient care.
3. Illustrate the anatomy and physiology of the heart and its significant structures.
4. Summarize risk factors for the development of heart disease.
6. Explain the signs and symptoms of myocardial infarction in women.
7. Compare and contrast the treatment protocols for hypertension.
8. Outline the causes and results of congestive heart failure.
9. Summarize the effects of inflammation and valvular disorders on cardiac function.
10. Describe the anatomy and physiology of the vascular system.
11. Differentiate among the various types of shock.
12. Summarize the characteristics of common vascular disorders.
13. Outline typical cardiovascular diagnostic procedures.
14. Describe patient education topics for cardiovascular patients.
Vocabulary
chordae tendineae (kor′-duh/ten′y-din-uh) The tendons that anchor the cusps of the heart valves to the papillary muscles of the myocardium, preventing valvular prolapse.
intermittent claudication Recurring cramping in the calves caused by poor circulation of blood to the muscles of the lower leg.
ischemia (is-ke′-mia) A decreased supply of oxygenated blood to an area or body part.
scleroderma (skluh-rah-der′-muh) An autoimmune disorder that affects the blood vessels and connective tissue, causing fibrous degeneration of the major organs.
vegetations Abnormal growth of tissue surrounding a valve consisting of fibrin, platelets, and bacteria.
Scenario
Adam Stern, CMA (AAMA), has been working for more than 3 years as a medical assistant in a variety of physicians’ offices. Adam recently was hired to work at City Hospital in the cardiology department. His job description includes working in the clinical area of the practice and assisting the attending physicians with patient education and follow-up. Because Adam has never worked for a cardiologist, he is concerned about his knowledge base and competency in cardiac patient care. Part of Adam’s responsibilities will be to help evaluate patient education materials about the warning signs of a heart attack, especially the differences between the symptoms seen in men and those seen in women. The practice also is in the process of updating its policy and procedures manual, and Adam has been asked to create scenarios for telephone screening of patients who call in with symptoms of chest pain.
While studying this chapter, think about the following questions:
Cardiac disease, in the past, was frequently seen in men but seldom in women. That has changed, and today the most common cause of illness and death, regardless of gender, is cardiovascular disease. Medical assistants in all specialties often care for patients with heart disorders. Seldom does the cardiologist discover the heart problem. Most patients who see this specialist already have been diagnosed with a suspected heart disorder and were referred to the cardiologist for verification of the initial diagnosis and specialized treatment.
Because of the overwhelming number of people with cardiovascular problems, all medical assistants must understand the cardiovascular system, be able to recognize early symptoms of potential disorders, perform basic screening tests when ordered by the physician, and assist the physician in the examination of the heart and blood vessels.
Anatomy and Physiology of the Heart
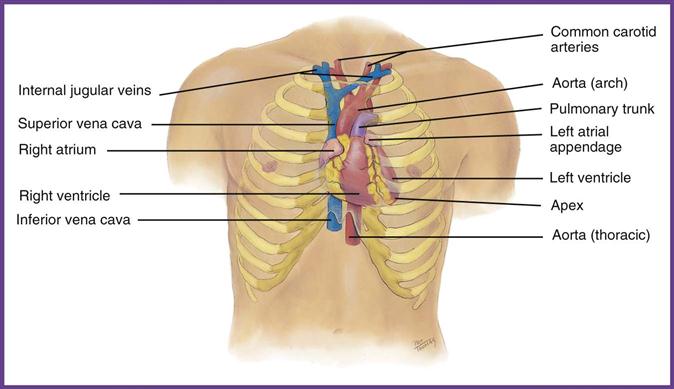
The heart is a hollow, muscular organ situated in the thoracic cavity in the mediastinal region, between the right and left pleural spaces. It weighs about 9 ounces and is about the size of a fist; approximately two thirds of it is located to the left of the sternum (Figure 47-1). The heart is a pump that provides the force needed to push blood through all the arteries of the body; the blood circulates a continuous supply of oxygen and nutrients to the cells and picks up the metabolic waste products from them. If deprived of these vital functions, the cells die. At the same time, the heart pushes deoxygenated blood through the pulmonary artery to the lungs for oxygen saturation and receives oxygenated blood back through the pulmonary veins into the left side of the heart. The average adult heart pumps about 5 L of blood every minute. If the heart loses its pumping action for even a few brief minutes, death or permanent damage can result.
Layers of the Heart
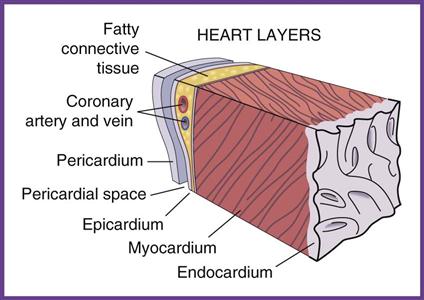
The heart is enclosed in a double-membrane sac called the pericardium. The outer layer of the pericardial sac, the parietal pericardium, is a tough membrane that connects the heart to the diaphragm and serves as a physical barrier to protect the heart against infection or inflammation from the lungs or pleural space. The inner layer, the visceral pericardium or epicardium, forms the first layer of the heart. Between the two membranes is a small space, the pericardial cavity, which contains about 30 mL of pericardial fluid; this fluid lubricates the internal surfaces of the pericardial membranes, enabling them to slide across each other during heart contractions. The middle layer of the heart, the myocardium, is the muscle layer that constitutes the largest percentage of the heart wall. Contractions of this muscle layer force the blood from the heart into the vessels. The inner layer of the heart, the endocardium, includes the heart valves that separate the chambers of the heart and provide a means of blocking the flow of blood from major blood vessels entering and exiting the heart (Figure 47-2).
Heart Chambers and Arteries
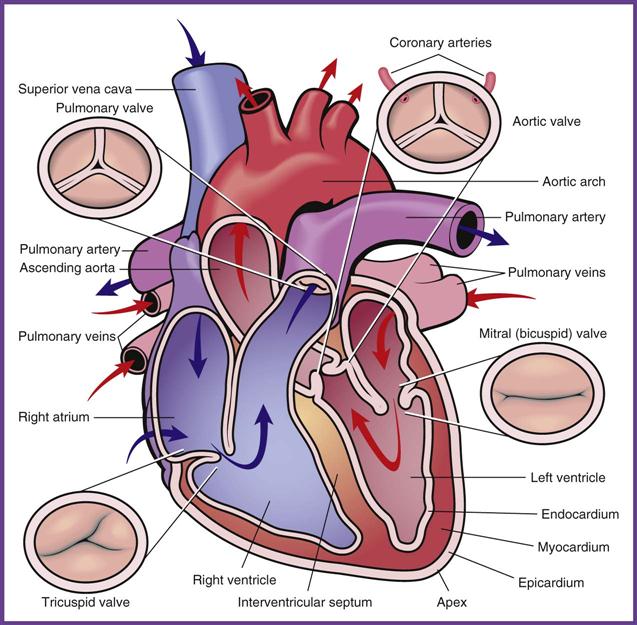
The heart is divided into four chambers (Figure 47-3). The atria, the top chambers, receive blood, and the ventricles, the bottom chambers, pump the blood out. The blood flow through the heart begins in the right atrium, which receives deoxygenated blood from the inferior and superior venae cavae. The atria contract, and blood passes through the tricuspid valve into the right ventricle; the ventricles contract, and blood passes from the right ventricle to the lungs via the pulmonary artery (the only artery in the body that contains deoxygenated blood). Oxygenation occurs in the alveoli of the lungs, and the now oxygenated blood returns to the left atria through the pulmonary veins (the only veins in the body that carry oxygen-rich blood). The atria contract, and blood passes through the mitral (bicuspid) valve into the left ventricle; the ventricles contract, and oxygen-rich blood is sent out to the body through the aorta (the largest artery in the body).
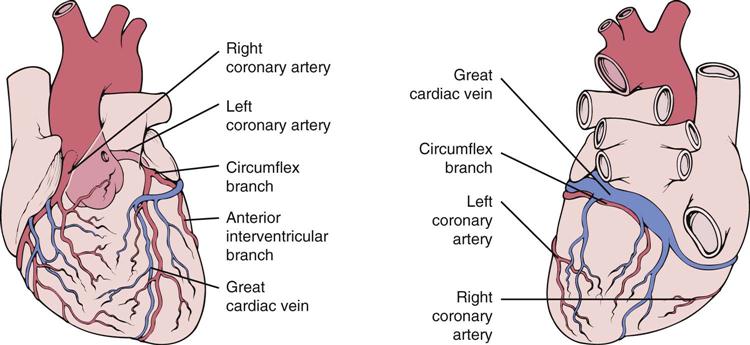
The myocardium requires a continuous supply of oxygen and nutrients, which are delivered through two coronary arteries that branch off the aorta above the aortic valve (Figure 47-4). The right coronary artery nourishes the anterior and posterior myocardium on the right side of the heart, and the left coronary artery does the same on the left side. The left coronary artery quickly divides and forms the left anterior descending artery and the left circumflex artery. Smaller branches of the coronary arteries feed the myocardium and the endocardium. Any interference in blood flow in any of the coronary vessels alters the action of the heart.
Heart Conduction
A sophisticated electrical conduction system operated by specialized cells located at various sites in the myocardium stimulates contractions. These muscle contractions move blood through the chambers of the heart and out through the aorta to the rest of the body. Each electrical impulse passes through the heart muscle in a twisting, spiral motion. These rhythmic waves stimulate the cardiac cells to beat, which causes the heart to contract.
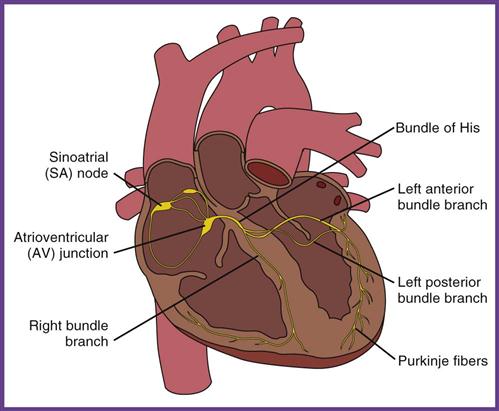
The cardiac impulse originates in specialized muscle tissue called the sinoatrial (SA) node. The SA node rhythmically initiates impulses 70 to 80 times a minute; because it creates the basic rhythm, it is the pacemaker of the heart. It is located in the posterior, superior wall of the right atrium, at the junction of the superior vena cava and the atrium and just above the tricuspid valve. When the SA node discharges its rhythm pattern into the myocardium, it passes across both atria, resulting in atrial contraction and forcing blood through the valves and into the ventricles. The wave then passes through a second area of specialized muscle tissue on the septal wall between the right atrium and right ventricle, called the atrioventricular (AV) node. The AV node holds the impulse for a fraction of a second to prevent inappropriately high atrial rates and to permit the blood to empty from the atria through the tricuspid and mitral valves. At this moment the chordae tendineae tightly close the valves between the atria and the ventricles. The AV node then releases the charge, sending it down through the bundle of His, which is located in the septum between the right and left ventricles. This bundle is divided into two main branches: the right bundle, on the right side of the septum, and the left bundle, on the left side. From the bundle branches, transmission of the cardiac wave continues through a mass of cardiac muscle fibers known as the Purkinje fibers. The Purkinje fibers totally encase both ventricles, and the cardiac wave causes the ventricles to contract (Figure 47-5).
Contraction of the atria and the ventricles is also called depolarization. After the chambers contract, a period of electric recovery occurs (repolarization), and the heart then returns to the resting phase (polarization), which starts the entire cycle again. The normal cardiac cycle consists of atrial contraction, ventricular contraction, recovery, and heart rest. This cycle maintains the average range of 60 to 100 beats per minute and a normal heart rhythm. It is this electrical force that is traced and evaluated when an electrocardiogram (ECG) is done. (Chapter 49 discusses ECGs in more detail.)
Diseases and Disorders of the Heart
Many diseases and disorders affect the heart and its blood vessels. Disorders that occur when the rhythm of the heart becomes irregular are addressed in Chapter 49. Cardiac disease has multiple risk factors; some of these cannot be changed, and others people can change or seek to have treated. The more risk factors a person has, the greater his or her risk of developing cardiovascular disease.
Coronary Artery Disease and Myocardial Infarction
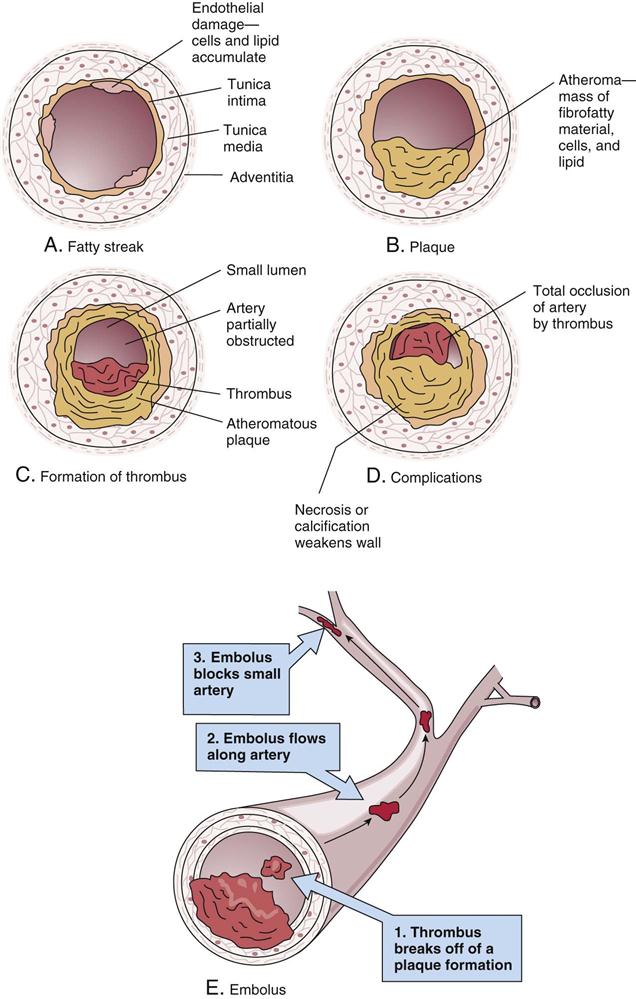
Coronary artery disease (CAD) causes more than 1 million deaths in the United States every year. In CAD, the formation of atherosclerotic plaques narrows the arteries supplying the myocardium. Atherosclerotic plaque buildup is primarily related to cholesterol blood levels (see Chapter 30, Table 30-2). Cholesterol blood testing is explained in Chapter 54. Medications that may be prescribed to treat hypercholesterolemia are described in Table 47-1. An atherosclerotic plaque originates at the site of a chronic injury to the endothelial lining of the artery caused by risk factors associated with heart disease (e.g., smoking or hypertension). Platelets attach to the site of the endothelial injury, and lipids continue to accumulate. Eventually an atheroma forms, which is made up of a tough collagen shell covering a fatty center that extends out into the lumen of the vessel, restricting blood flow past the plaque. Inflammation at the site attracts platelets to the surface of the atheroma, resulting in the formation of a clot (thrombus) that can completely occlude the lumen of the vessel, depriving the myocardium of an adequate nutritious blood supply (Figure 47-6). The cardinal symptom of myocardial ischemia is angina pectoris. Anginal chest pain is pain behind the sternum that is precipitated by exertion but that can be relieved either by rest or by sublingual nitroglycerin.
TABLE 47-1
Prescription Medications to Lower Blood Cholesterol Levels
| CLASSIFICATION | ACTION | SIDE EFFECTS AND CAUTIONS |
| Statins Altoprev (lovastatin) Crestor (rosuvastatin) Lescol (fluvastatin) Lipitor (atorvastatin) Mevacor (lovastatin) Pravachol (pravastatin) Zocor (simvastatin) | Lower LDL and triglycerides; slightly increase HDL | Constipation, nausea, diarrhea, stomach pain, cramps, muscle soreness, pain and weakness; possible interaction with grapefruit juice |
| Bile acid–binding resins Colestid (colestipol) Questran (cholestyramine sucrose) Welchol (colesevelam) | Lower LDL | Constipation, bloating, nausea, gas; may increase triglycerides |
| Cholesterol absorption inhibitors Zetia (ezetimibe) | Lower LDL; slightly decrease triglycerides; slightly increase HDL | Fatigue, gas, constipation, abdominal pain, cramps, muscle soreness; possible interaction with grapefruit juice |
| Fibrates Lofibra (fenofibrate) Lopid (gemfibrozil) TriCor (fenofibrate) | Decrease triglycerides; increase HDL | Nausea, stomach pain, gallstones |
| Combination statin and niacin Advicor (niacin-lovastatin) | Decrease LDL and triglycerides; increase HDL | Facial and neck flushing, dizziness, heart palpitations, shortness of breath, sweating, chills; possible interaction with grapefruit juice |
HDL, High-density lipoprotein; LDL, low-density lipoprotein.
Patients may be asymptomatic until the disease becomes fully developed. The first symptom may be angina, followed by pressure or fullness in the chest, syncope, shortness of breath, edema, unexplained coughing spells, and fatigue. A patient reporting any of these symptoms should be seen by the physician immediately.
In recent years the rate of heart disease has declined in men but not in women. Traditional risk factors negatively affect both genders; however, women are at greater risk if they have metabolic syndrome (a combination of hypertension, elevated insulin levels, excess body fat around the waist, and high blood cholesterol levels); if they have increased levels of stress and/or depression; if they smoke (female smokers are at much greater risk than male smokers); and if they have reduced estrogen production before menopause. The difference in female risks and symptoms is associated with the method of plaque buildup in women; the plaque tends to develop as an evenly spread layer along the entire lumen of the blood vessels rather than as a localized plaque buildup, as is seen in men. Women with heart disease typically experience this diffuse atheroma buildup in smaller vessels, which causes more subtle symptoms than the crushing chest pain associated with classic myocardial infarctions (MIs).
The major concern in heart disease is the lack of blood to the myocardium, which occurs when a vessel becomes totally blocked. Ischemia over a prolonged period leads to necrosis (death) of a portion of the myocardium, resulting in an MI, or heart attack. Symptoms of an MI are similar to those of angina; however, an MI is identified by pain that lasts longer than 30 minutes and is not relieved by rest or nitroglycerin tablets. An MI is a life-threatening event; intervention must begin within the first hour, or death may occur.
Diagnostic and Therapeutic Procedures
An MI is diagnosed by ECG changes and elevated cardiac enzymes. The blood test most often ordered to confirm myocardial damage is the creatine kinase (CK) level. CK levels begin to increase approximately 6 hours after the start of a heart attack and reach their peak in about 18 hours; they return to normal in 24 to 36 hours. The more severe the cardiac damage, the longer it takes for CK levels to peak and then return to normal. Determination of the troponin levels is a more sensitive blood test that can detect minor myocardial damage not evident with CK levels. Troponins increase in the bloodstream within 4 to 6 hours after the initial myocardial damage and peak in 10 to 24 hours. In the case of minor myocardial damage, troponin levels remain elevated up to 10 to 14 days, allowing for later diagnosis of the event. Patients diagnosed with an MI typically are hospitalized immediately, started on oxygen, and continuously monitored by ECG. Additional diagnostic procedures, such as an echocardiogram and heart catheterization, are discussed later in this chapter.
Medical treatment includes the use of thrombolytic medications, such as alteplase (Activase) and reteplase (Retavase), to dissolve coronary artery blockage and prevent permanent myocardial damage. To be most effective, this treatment must be started within 3 hours of the episode; however, it is still helpful if administered within 12 hours of initial symptoms. This timetable makes it extremely important that patients be diagnosed and treated as soon as possible. Thrombolytic medications are administered intravenously (IV) along with heparin to prevent clots that are being dissolved from reforming. Aspirin also is used to prevent the formation of blood clots in affected blood vessels. Additional pharmaceutical treatment includes the use of nitroglycerin to dilate the coronary arteries so that more blood can be delivered to the myocardium; beta blockers (atenolol [Tenormin], metoprolol [Lopressor], or propranolol [Inderal]) to slow the heart rate and lower blood pressure; anticoagulants (warfarin [Coumadin]) for 3 to 6 months to prevent thrombus formation; and anticholesterol agents to lower blood cholesterol levels and prevent subsequent formation of atherosclerotic plaques.
When the coronary arteries that supply blood to the myocardium are blocked, or occluded, either percutaneous transluminal coronary angioplasty (PTCA) or coronary artery bypass grafting (CABG) may be indicated. (These surgical procedures are discussed later in this chapter.)
After discharge from the hospital, patients with CAD that has resulted in an MI face multiple lifestyle changes to prevent another episode. Recommendations include no smoking; regular light exercise, such as walking 30 minutes a day, 5 days a week; a diet low in salt, fat, and cholesterol; maintaining a healthy weight; controlling hypertension; reducing stress; and limiting alcohol intake to one or two drinks a day. The medical assistant should be prepared to provide encouragement and to reinforce the importance of lifestyle changes to prevent future heart problems. If ordered by the physician, professional referrals to a cardiac rehabilitation program and dietitian can also be helpful.
Hypertensive Heart Disease
Chronic elevated blood pressure can result in left ventricular hypertrophy (enlargement), angina, MI, or heart failure. Hypertension also is a major cause of stroke and nephropathy (kidney disease). Some of the risk factors for hypertension include a family history of hypertension or stroke, hypercholesterolemia (high blood cholesterol), smoking, high sodium intake, diabetes, excessive alcohol intake, sedentary lifestyle, obesity, aging, prolonged stress, and race (African-Americans have a higher incidence than Caucasians). Hypertension has an insidious onset, and the patient shows few, if any, signs and symptoms until permanent damage has occurred. Initial symptoms may include general malaise and headache; epistaxis (nosebleed), vertigo, nausea, or syncope can occur with prolonged hypertension.
The two types of hypertension are primary hypertension and secondary hypertension. Secondary hypertension occurs because of a disease process in another body system, such as renal disease or an endocrine disorder. Before secondary hypertension can be properly treated, the underlying disease process must be resolved.
Primary, or essential, hypertension is idiopathic (of unknown cause) and is diagnosed if the patient’s blood pressure is persistently higher than 119 mm Hg systolic and/or 79 mm Hg diastolic at two or more office visits over several weeks or months. If the medical assistant first notes that a patient’s blood pressure is elevated, the pressure should be checked in both arms with the patient seated and after the patient has been standing for at least 2 minutes with a cuff that is the proper size for the patient’s arm. If the pressure readings are different, the physician uses the higher value for diagnostic purposes. The patient’s blood pressures should be checked again after at least 2 minutes. All of these readings must be documented in the patient’s record. Some patients have “white coat hypertension,” which appears only when they visit the physician. If the patient has a history of this problem, have him or her lie down on the examination table and rest for a few minutes before the blood pressure is taken; this may help in obtaining a more accurate reading (Table 47-2).
TABLE 47-2
Stages and Treatment of Hypertension
| BLOOD PRESSURE | TREATMENT |
| Prehypertension 120 to 139/80 to 89 mm Hg | Lifestyle modification (reduced sodium, low-fat diet; regular aerobic activity; moderate alcohol intake; smoking cessation; weight loss; stress reduction) Drug therapy for patients with diabetes mellitus or chronic kidney disease |
| Stage 1 hypertension 140 to 159/90 to 99 mm Hg | Consider coexisting conditions Thiazide-type diuretics (e.g., furosemide [Lasix] or hydrochlorothiazide plus triamterene [Dyazide]) for most patients |
| Stage 2 hypertension 160/100 mm Hg | Consider coexisting conditions Two-drug combination for most patients |
Recommendations from the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Accessed February 14, 2012. Available at www.nhlbi.nih.gov/health/health-topics/topics/hbp/.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree