Antituberculars, Antifungals, Peptides, and Metronidazole
Objectives
• Compare first-line and second-line antitubercular drugs, and give examples of each.
• Differentiate between the five groups of antifungal drugs.
• Explain the uses of polyenes.
• Differentiate the adverse reactions of antitubercular, antifungal, and peptide drugs.
• Apply the nursing process for patients taking antitubercular, antifungal, and peptide drugs.
• Describe the side effects/adverse effects for metronidazole.
Key Terms
acquired immunodeficiency syndrome, p. 437
antifungal drugs, p. 441
antimycotic drugs, p. 441
antitubercular drugs, p. 437
first-line drugs, p. 438
hepatotoxicity, p. 438
human immunodeficiency virus, p. 437
neurotoxicity, p. 445
opportunistic infections, p. 441
paresthesias, p. 445
peptides, p. 445
prophylaxis, p. 446
second-line drugs, p. 438
![]() http://evolve.elsevier.com/KeeHayes/pharmacology/
http://evolve.elsevier.com/KeeHayes/pharmacology/
This chapter covers antitubercular drugs, antifungal drugs, peptide drugs, and metronidazole. Although these drug categories differ from each other, they each contain drugs that inhibit or kill organisms that cause disease.
Tuberculosis
Tuberculosis (TB) is caused by the acid-fast bacillus Mycobacterium tuberculosis. This pathogen is frequently called the tubercle bacillus. Tuberculosis is one of the world’s major health problems, killing more persons than any other infectious disease, including acquired immunodeficiency syndrome (AIDS) (immune disorder characterized by opportunistic diseases). More than 1.5 billion people in the world have TB, and many are unaware of their infection. Each year more than 8 million new cases of TB are diagnosed. Until the 1980s, the incidence of TB had decreased in the United States. The later increase in TB can be attributed, in part, to the increase in people with AIDS in whom active TB has developed because of compromised immune systems. In addition, the increased incidence is partly a result of increasingly crowded living conditions in urban areas. Patients more susceptible to TB are those with alcohol addiction, AIDS, and debilitative conditions.
Pathophysiology
TB is transmitted from one person to another by droplets dispersed in the air through coughing and sneezing. The organisms are inhaled into the alveoli (air sacs) of the lung. If the body’s immune system is strong and intact, phagocytes stop the multiplication of the tubercle bacilli. When the immune system is compromised, however, tubercle bacilli can spread from the lungs to other organs of the body via the blood and lymphatic system. Dissemination of TB bacilli can be found in the liver, kidneys, spleen, and other organs. Symptoms of TB include anorexia, cough and sputum production, increased fever, night sweats, weight loss, and positive acid-fast bacilli in the sputum.
Antitubercular Drugs
Before 1944, many people died from TB because of the absence of drug therapy. Streptomycin, a parenteral antibiotic, was the first drug used to treat TB. Isoniazid (INH), discovered in 1952, was the first oral drug preparation effective against the tubercle bacillus. Isoniazid is a bactericidal drug that inhibits tubercle cell wall synthesis and blocks pyridoxine (vitamin B6), which is used for intracellular enzyme production. When isoniazid is prescribed, pyridoxine may also be prescribed to avoid deficiency and possible occurrence of peripheral neuropathy. Group names for drugs used to treat TB include antimycobacterial agents and antitubercular drugs (agents that treat tuberculosis).
Prophylactic antitubercular therapy is suggested for individuals who have been in close contact with persons with TB. Prophylaxis is also recommended for those who test positive for human immunodeficiency virus (HIV) (virus causing an infection characterized by profound immunosuppression) and also have a positive TB skin test or are in close contact with someone who has TB. Patients who have converted from a negative to a positive TB skin test should be considered candidates for prophylactic isoniazid therapy. Young children who have been in contact with persons with active TB are at high risk and should receive prophylactic antitubercular therapy. When a person is diagnosed with TB, family members are usually given prophylactic doses of isoniazid for 6 months to 1 year. For HIV-positive patients with positive TB skin tests, a 2-month prophylactic treatment with rifampin and pyrazinamide may be recommended.
Prophylactic therapy is contraindicated for persons with liver disease. Isoniazid is the primary antitubercular drug used and may cause isoniazid-induced liver damage. Other antitubercular drugs may also cause liver damage if given in high doses over an extended period.
Single-drug therapy with isoniazid proved ineffective in treating TB, because resistance to the drug developed in a short time. It was discovered that when a combination of antitubercular drugs was used, bacterial resistance did not occur, and the duration of treatment was reduced from 2 years to 6 to 9 months. Different combinations of drugs can be used: (1) isoniazid and rifampin; (2) isoniazid, rifampin, and ethambutol; or (3) isoniazid, rifampin, and pyrazinamide. Rifampin and ethambutol were discovered in the early 1960s; neither drug is effective against the tubercle bacillus when given alone. In fact, if rifampin is taken alone, bacterial resistance occurs quickly. Prototype Drug Chart 32-1 lists the drug data for isoniazid.
Multidrug therapy against TB is more effective. The treatment regimen is divided into two phases: the first, or initial, phase lasts 2 months, and the second phase covers the next 4 to 7 months. The total treatment plan is for 6 to 9 months and depends on the response to the antitubercular therapy. Table 32-1 gives examples of various drug regimens to treat TB.
TABLE 32-1
POSSIBLE DRUG REGIMENS FOR TUBERCULOSIS
| PHASE | EXAMPLE I | EXAMPLE II | EXAMPLE III | EXAMPLE IV |
| First phase (2 mo)* | isoniazid, rifampin | isoniazid, rifampin, pyrazinamide | isoniazid, rifampin, streptomycin | isoniazid, rifampin, pyrazinamide, kanamycin or ciprofloxacin |
| Second phase (4-7 mo) | isoniazid, rifampin | isoniazid, rifampin, ethambutol | isoniazid, rifampin, capreomycin or cycloserine | isoniazid, rifampin, ethambutol, streptomycin or kanamycin or ciprofloxacin or clarithromycin or capreomycin |
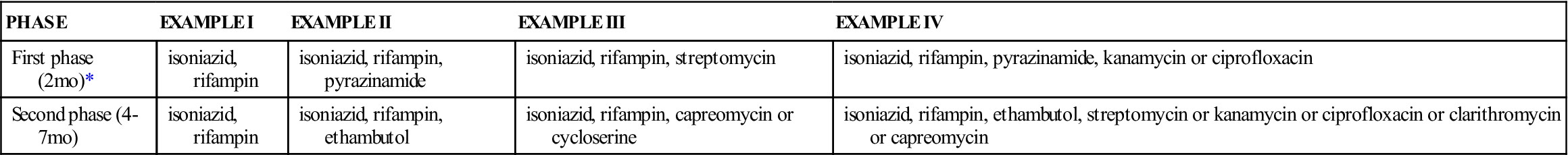
*If there is bacterial resistance to isoniazid, the first phase of the drug regimen may be rifampin, ethambutol, and pyrazinamide. Adjust drug regimen according to drug susceptibility. The health care provider determines which antitubercular drug and how many combinations to use. Symptoms for drug toxicity should be closely monitored. Examples III and IV may be used in various combinations for multidrug resistance.
If multidrug resistance to the tubercle bacilli persists, other antibacterial drugs such as the aminoglycosides (streptomycin, kanamycin, amikacin) or the fluoroquinolones (ciprofloxacin, ofloxacin) may be given as part of multidrug therapy. Susceptibility testing to determine drug resistance should be performed before drug therapy. At times, susceptibility testing of the sputum and antitubercular drugs is performed, but only if the patient has not responded to the drug therapy regimen.
Mycobacterium tuberculosis strains that are resistant to streptomycin can be sensitive to kanamycin. An aminoglycoside should not be taken if renal dysfunction is present. When antibacterial agents are used continuously or at high doses, the serum drug level should be closely monitored to avoid drug toxicity.
Pharmacokinetics
Isoniazid is well absorbed from the gastrointestinal (GI) tract. It can also be administered intramuscularly (IM). It has a very low protein-binding rate (10%), and its half-life is 1 to 4 hours. Isoniazid is metabolized by the liver, and 75% of the drug is excreted in the urine.
Pharmacodynamics
Isoniazid inhibits cell-wall synthesis of the tubercle bacillus. It is usually prescribed with other antitubercular agents. The onset of action and peak concentration time for oral and IM routes of isoniazid are the same. Peripheral neuropathy is an adverse reaction to isoniazid, so pyridoxine (vitamin B6) is usually taken with isoniazid to decrease the probability of neuropathy. Alcohol ingestion with the drug can increase the incidence of peripheral neuropathy. If phenytoin is taken with isoniazid, the effect of phenytoin may be decreased. Antacids decrease isoniazid absorption.
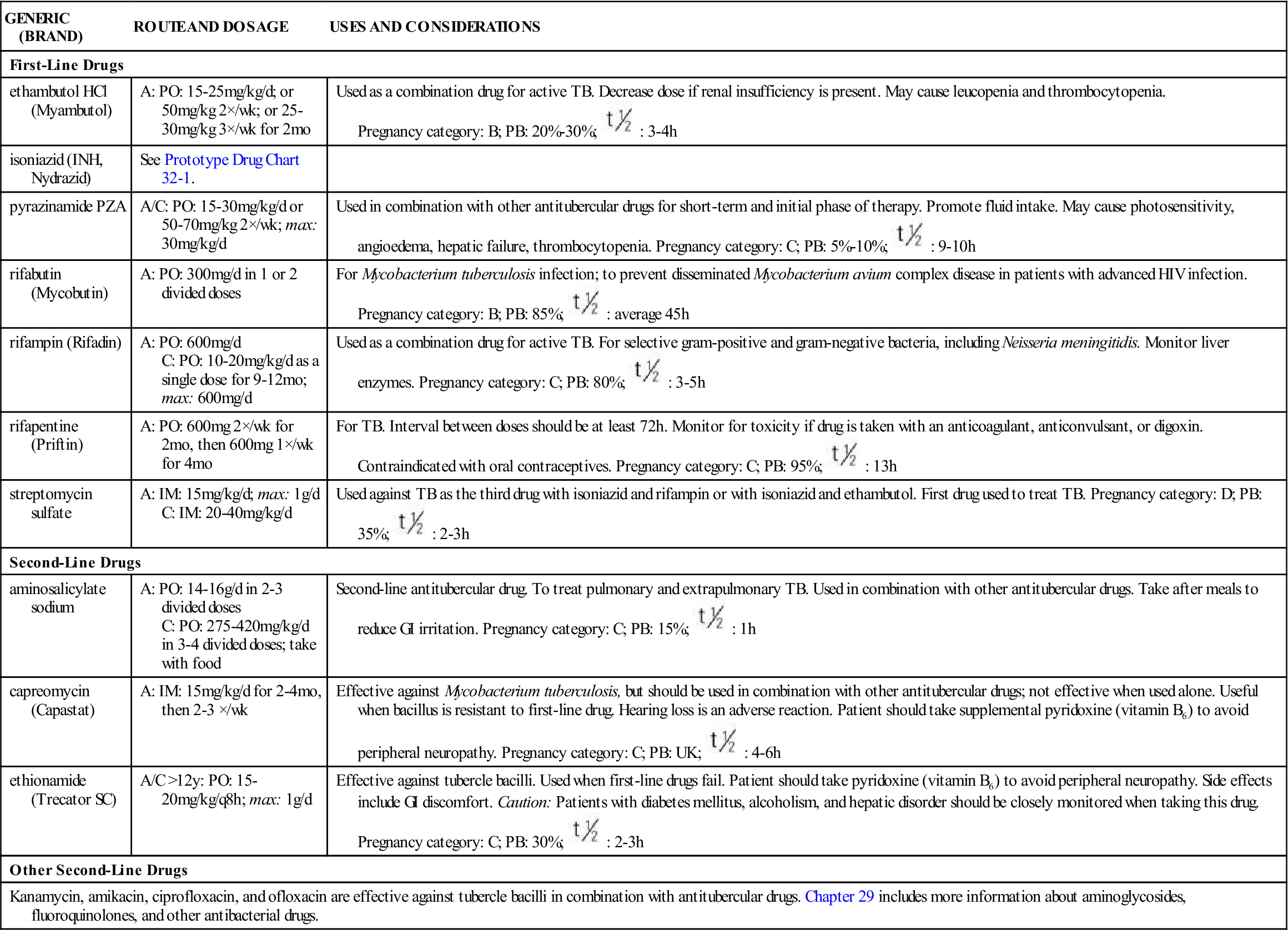
Antitubercular drugs are divided into two categories: first-line and second-line. First-line drugs (drugs chosen first) (i.e., isoniazid, rifampin, rifabutin, rifapentine, pyrazinamide, ethambutol, streptomycin) are considered more effective and less toxic than second-line drugs in treating TB. Rifapentine, an analog of rifampin, is the newest first-line drug for treating TB. The patient takes it only twice a week, unlike rifampin, which is given daily. To avoid resistance, rifapentine should be combined with another antitubercular drug. Second-line drugs (second-choice drugs) (i.e., para-aminosalicylic acid, kanamycin, cycloserine, ethionamide, capreomycin, pyrazinamide, others) are not as effective as first-line drugs; some can be more toxic. Second-line drugs may be used in combination with first-line drugs, especially to treat disseminated TB. First-line and some second-line drugs are described in Table 32-2.
TABLE 32-2
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| First-Line Drugs | ||
| ethambutol HCl (Myambutol) | A: PO: 15-25 mg/kg/d; or 50 mg/kg 2×/wk; or 25-30 mg/kg 3×/wk for 2 mo | Used as a combination drug for active TB. Decrease dose if renal insufficiency is present. May cause leucopenia and thrombocytopenia. Pregnancy category: B; PB: 20%-30%;  : 3-4 h : 3-4 h |
| isoniazid (INH, Nydrazid) | See Prototype Drug Chart 32-1. | |
| pyrazinamide PZA | A/C: PO: 15-30 mg/kg/d or 50-70 mg/kg 2×/wk; max: 30 mg/kg/d | Used in combination with other antitubercular drugs for short-term and initial phase of therapy. Promote fluid intake. May cause photosensitivity, angioedema, hepatic failure, thrombocytopenia. Pregnancy category: C; PB: 5%-10%;  : 9-10 h : 9-10 h |
| rifabutin (Mycobutin) | A: PO: 300 mg/d in 1 or 2 divided doses | For Mycobacterium tuberculosis infection; to prevent disseminated Mycobacterium avium complex disease in patients with advanced HIV infection. Pregnancy category: B; PB: 85%;  : average 45 h : average 45 h |
| rifampin (Rifadin) | A: PO: 600 mg/d C: PO: 10-20 mg/kg/d as a single dose for 9-12 mo; max: 600 mg/d | Used as a combination drug for active TB. For selective gram-positive and gram-negative bacteria, including Neisseria meningitidis. Monitor liver enzymes. Pregnancy category: C; PB: 80%;  : 3-5 h : 3-5 h |
| rifapentine (Priftin) | A: PO: 600 mg 2×/wk for 2 mo, then 600 mg 1×/wk for 4 mo | For TB. Interval between doses should be at least 72 h. Monitor for toxicity if drug is taken with an anticoagulant, anticonvulsant, or digoxin. Contraindicated with oral contraceptives. Pregnancy category: C; PB: 95%;  : 13 h : 13 h |
| streptomycin sulfate | A: IM: 15 mg/kg/d; max: 1 g/d C: IM: 20-40 mg/kg/d | Used against TB as the third drug with isoniazid and rifampin or with isoniazid and ethambutol. First drug used to treat TB. Pregnancy category: D; PB: 35%;  : 2-3 h : 2-3 h |
| Second-Line Drugs | ||
| aminosalicylate sodium | A: PO: 14-16 g/d in 2-3 divided doses C: PO: 275-420 mg/kg/d in 3-4 divided doses; take with food | Second-line antitubercular drug. To treat pulmonary and extrapulmonary TB. Used in combination with other antitubercular drugs. Take after meals to reduce GI irritation. Pregnancy category: C; PB: 15%;  : 1 h : 1 h |
| capreomycin (Capastat) | A: IM: 15 mg/kg/d for 2-4 mo, then 2-3 ×/wk | Effective against Mycobacterium tuberculosis, but should be used in combination with other antitubercular drugs; not effective when used alone. Useful when bacillus is resistant to first-line drug. Hearing loss is an adverse reaction. Patient should take supplemental pyridoxine (vitamin B6) to avoid peripheral neuropathy. Pregnancy category: C; PB: UK;  : 4-6 h : 4-6 h |
| ethionamide (Trecator SC) | A/C >12 y: PO: 15-20 mg/kg/q8h; max: 1 g/d | Effective against tubercle bacilli. Used when first-line drugs fail. Patient should take pyridoxine (vitamin B6) to avoid peripheral neuropathy. Side effects include GI discomfort. Caution: Patients with diabetes mellitus, alcoholism, and hepatic disorder should be closely monitored when taking this drug. Pregnancy category: C; PB: 30%;  : 2-3 h : 2-3 h |
| Other Second-Line Drugs | ||
| Kanamycin, amikacin, ciprofloxacin, and ofloxacin are effective against tubercle bacilli in combination with antitubercular drugs. Chapter 29 includes more information about aminoglycosides, fluoroquinolones, and other antibacterial drugs. | ||
Side Effects and Adverse Reactions
Side effects and adverse reactions differ according to the drug prescribed. For isoniazid, peripheral neuropathy can be a problem, especially for those who are malnourished, have diabetes mellitus, or are alcoholics. This condition can be prevented if pyridoxine (vitamin B6) is administered. Hepatotoxicity (liver toxicity) is an adverse reaction to isoniazid, rifampin, and streptomycin. Patients with liver disorders should not take these drugs unless liver enzymes are closely monitored, because liver enzymes may become elevated. The patient taking isoniazid, rifampin, and streptomycin may develop headaches, blood dyscrasias, paresthesias, GI distress, and ocular toxicity. Isoniazid may cause hyperglycemia, hyperkalemia, hypophosphatemia, and hypocalcemia. Rifampin turns body fluids orange, and soft contact lenses may be permanently discolored. The patient taking ethambutol may develop dizziness, confusion, hallucinations, and joint pain. Streptomycin may lead to many adverse effects, such as ototoxicity, optic nerve toxicity, encephalopathy, angioedema, CNS and respiratory depression, nephrotoxicity, and hepatotoxicity.
 : 1-4 h
: 1-4 h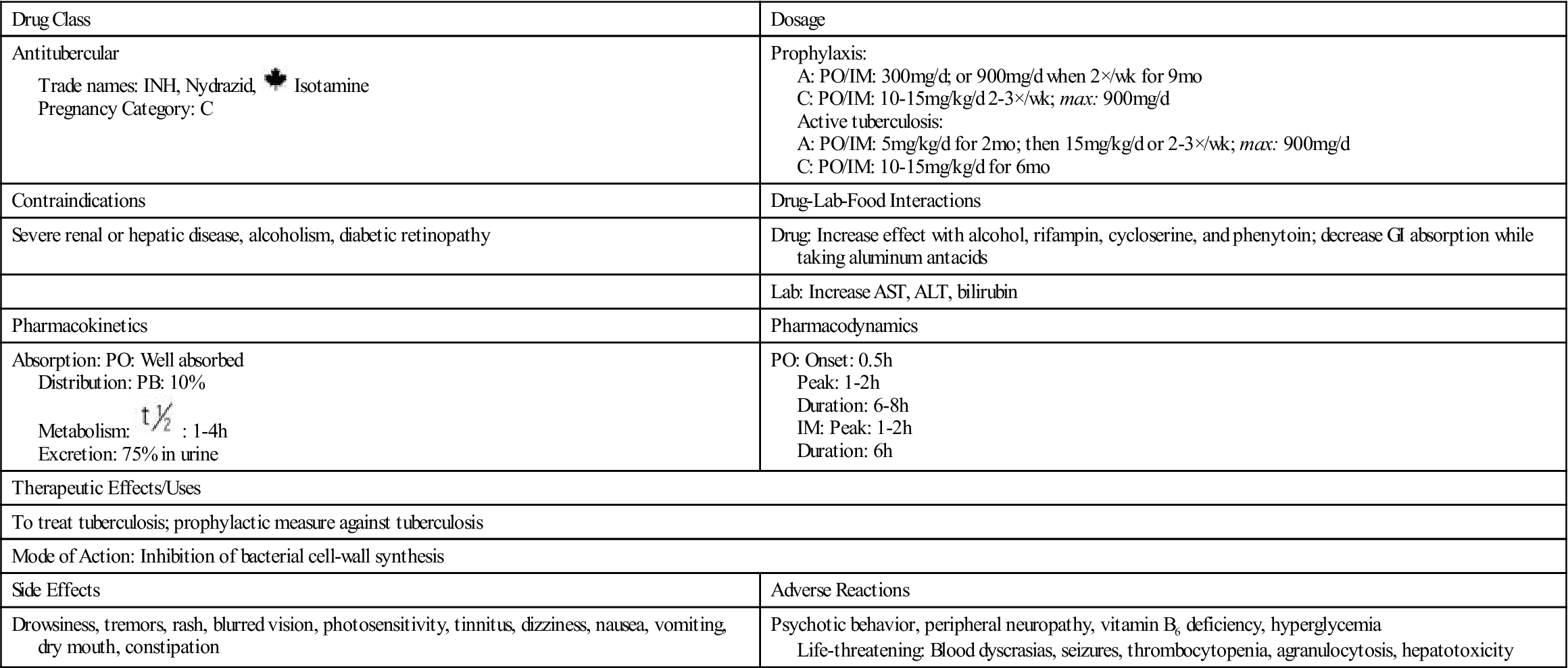
 , half-life; wk, week;
, half-life; wk, week;  , half-life; TB, tuberculosis; UK, unknown; wk, week; y, year; >, greater than.
, half-life; TB, tuberculosis; UK, unknown; wk, week; y, year; >, greater than.







