Antihyperlipidemics and Peripheral Vasodilators
Objectives
• Describe the action of the two main drug groups: antihyperlipidemics and peripheral vasodilators.
• Compare the side effects and adverse reactions of antihyperlipidemics.
• Differentiate the side effects and adverse reactions of peripheral vasodilators.
Key Terms
antihyperlipidemics, p. 664
apolipoproteins, p. 665
chylomicrons, p. 665
high-density lipoprotein, p. 664
high-sensitivity C-reactive protein, p. 668
homocysteine, p. 666
hyperlipidemia, p. 664
lipoprotein, p. 664
low-density lipoprotein, p. 664
peripheral vasodilators, p. 664
very low-density lipoproteins, p. 664
Various drugs are used to maintain or decrease blood lipid concentrations and promote dilation of vessels. Drugs that lower blood lipids are called antihyperlipidemics, antilipidemics, antilipemics, and hypolipidemics. In this chapter, drugs used to lower lipoproteins are called antihyperlipidemics. Peripheral vasodilators are drugs that dilate vessels that have been narrowed by vasospasm.
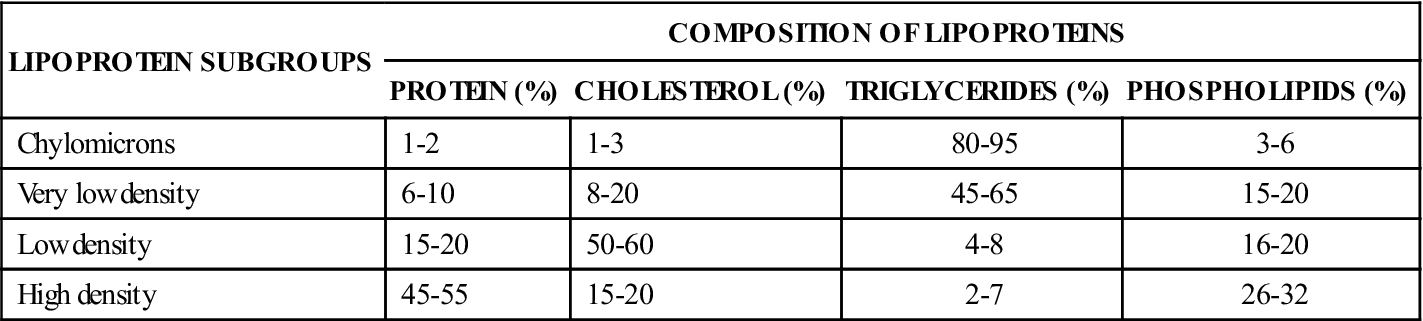
Lipoproteins
Lipids (cholesterol, triglycerides, and phospholipids) are bound in the inner shell of protein, which is a carrier that transports lipids in the bloodstream. When there is an excess of one or more lipids in the blood, the condition is known as hyperlipidemia or hyperlipoproteinemia. The four major categories of lipoprotein are high-density lipoprotein (HDL), low-density lipoprotein (LDL), very low-density lipoprotein (VLDL), and chylomicrons. HDL, also known as “friendly” or “good” lipoprotein, is the smallest, most dense lipoprotein, meaning that it contains more protein and less fat than the others. The function of HDL is to remove cholesterol from the bloodstream and deliver it to the liver for excretion in bile. LDL, the “bad” lipoprotein, contains 50% to 60% of cholesterol in the bloodstream. With an elevated LDL, there is greater risk for developing atherosclerotic plaques and heart disease. VLDL carries mostly triglycerides and less cholesterol. The chylomicrons are large particles that transport fatty acids and cholesterol to the liver. They are composed mostly of triglycerides. Table 46-1 presents the composition of the lipoproteins.
TABLE 46-1
| LIPOPROTEIN SUBGROUPS | COMPOSITION OF LIPOPROTEINS | |||
| PROTEIN (%) | CHOLESTEROL (%) | TRIGLYCERIDES (%) | PHOSPHOLIPIDS (%) | |
| Chylomicrons | 1-2 | 1-3 | 80-95 | 3-6 |
| Very low density | 6-10 | 8-20 | 45-65 | 15-20 |
| Low density | 15-20 | 50-60 | 4-8 | 16-20 |
| High density | 45-55 | 15-20 | 2-7 | 26-32 |
Serum cholesterol and triglyceride measurements are frequently part of a regular physical examination or readmission evaluation and are used as baseline test results. If the levels are high, a 12- to 14-hour fasting lipid profile may be ordered. When cholesterol, triglycerides, and LDL are elevated, the patient is at increased risk for coronary artery disease (CAD). Table 46-2 lists the various serum lipids and their reference values (normal serum levels) according to risk classification.
TABLE 46-2
| LIPIDS | DESIRABLE (mg/dL) | LEVEL OF RISK FOR CAD | ||
| LOW RISK (mg/dL) | MODERATE RISK (mg/dL) | HIGH RISK (mg/dL) | ||
| Cholesterol | 150-200 | 200 | 200-240 | >240 |
| Triglycerides | 40-150 | Values vary with age | Values vary with age | >190 |
| Lipoproteins | ||||
| LDL | <100 | 100-130 | 130-159 | >160 |
| HDL | >60 | 50-60 | 35-50 | <35 |
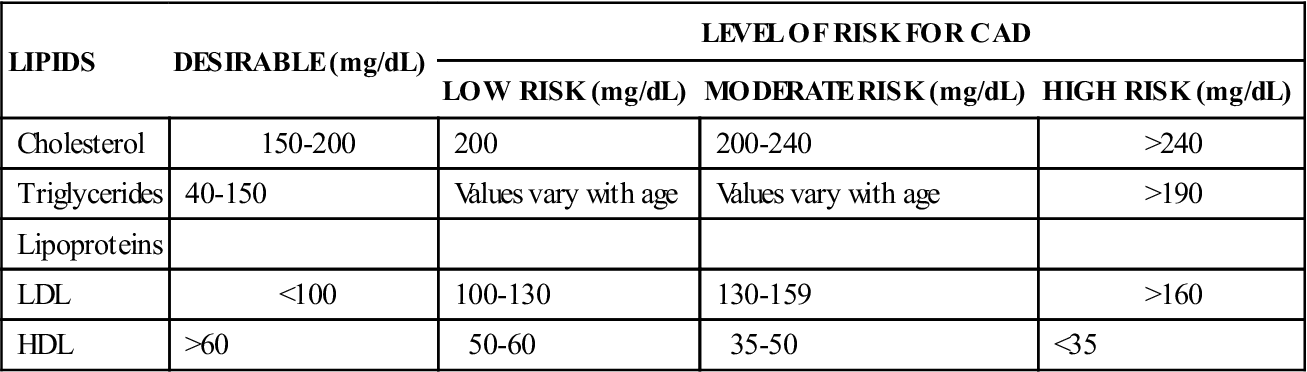
CAD, Coronary artery disease; HDL, high-density lipoproteins; LDL, low-density lipoproteins.
Apolipoproteins
Apolipoproteins are within the lipoprotein shell and contain apolipoprotein (apo) A-1, apoB, and apoE. The major component of apoA1 is HDL. The major component of apoB is LDL, which exists in two forms, apoB-100 and apoB-48. ApoB-100 has VLDL as well as LDL and is a better indicator of risk for coronary artery disease (CAD) than LDL alone.
Nonpharmacologic Methods for Cholesterol Reduction
Before drugs to lower LDL and raise HDL are prescribed, nondrug therapy should be initiated for decreasing cholesterol. Saturated fats and cholesterol in the diet should be reduced. Total fat intake should be 30% or less of caloric intake, and cholesterol intake should be 300 mg/d or less. The patient should be advised to read labels on containers and buy appropriate foods. Patients should choose lean meats, especially chicken and fish.
In many cases, diet alone will not lower blood lipid levels. Because 75% to 85% of serum cholesterol is endogenously (internally) derived, dietary modification alone will typically lower total cholesterol levels by only 10% to 30%. This and the fact that adherence to dietary restrictions is often short-lived explains why many patients do not respond to diet modification alone.
Exercise is an important aspect of the nonpharmacologic method to reduce cholesterol and increase HDL. For the older adult, exercise can be walking and bicycling. Smoking is another risk factor that should be eliminated. Smoking increases LDL cholesterol and decreases HDL.
If nonpharmacologic methods are ineffective for reducing cholesterol, LDL, and VLDL and hyperlipidemia remains, antihyperlipidemic drugs are prescribed to lower blood lipid levels. It must be emphasized to the patient that dietary changes need to be made and an exercise program followed even after drug therapy is initiated. The type of antihyperlipidemics ordered depends on the lipoprotein phenotype (Table 46-3).
TABLE 46-3
HYPERLIPIDEMIA: LIPOPROTEIN PHENOTYPE
| TYPE* | MAJOR LIPIDS |
| I | Increased chylomicrons and increased triglycerides. Uncommon. |
| IIA | Increased low-density lipoprotein (LDL) and increased cholesterol. Common. |
| IIB | Increased very low-density lipoprotein (VLDL), increased LDL, increased cholesterol and triglycerides. Very common. |
| III | Moderately increased cholesterol and triglycerides. Uncommon. |
| IV | Increased VLDL and markedly increased triglycerides. Very common. |
| V | Increased chylomicrons, VLDL, and triglycerides. Uncommon. |
*Types II and IV are commonly associated with coronary artery disease.
Antihyperlipidemics
Drugs that lower lipid levels include bile-acid sequestrants, fibrates (fibric acid), nicotinic acid, cholesterol absorption inhibitor, and hepatic 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors (statins). The statins have fewer adverse effects and are well tolerated.
One of the first antihyperlipidemics, cholestyramine (Questran), is a bile-acid sequestrant that reduces LDL cholesterol (LDL-C) levels by binding with bile acids in the intestine. It is effective against hyperlipidemia type II. This group may be used as an adjunct to the statins. The drug comes in a gritty powder, which is mixed thoroughly in water or juice. Colestipol (Colestid) is another resin antihyperlipidemic similar to cholestyramine. Both are effective in lowering cholesterol. Colesevelam HCl, another bile acid sequestrant similar to cholestyramine and colestipol, is an agent that has fewer side effects (less constipation, flatulence, and cramping). Colesevelam also has less effect on the absorption of fat-soluble vitamins than the older agents and is usually the first-choice bile-acid sequestrant drug.
Gemfibrozil (Lopid) is a fibric acid derivative that is more effective at reducing triglyceride and VLDL levels than reducing LDL. It is used primarily to reduce hyperlipidemia type IV, but it can also be used for type II hyperlipidemia. This drug is highly protein-bound and should not be taken with anticoagulants, because they compete for protein sites. The anticoagulant dose should be reduced during antihyperlipidemic therapy, and the international normalized ratio (INR) should be closely monitored. Fenofibrate has similar actions and some of the same side effects as gemfibrozil. If taken with warfarin, bleeding might occur. It is highly protein-bound.
Nicotinic acid, or niacin (vitamin B3), reduces VLDL and LDL. Nicotinic acid is actually very effective at lowering cholesterol levels, and its effect on the lipid profile is highly desirable. Because it has numerous side effects and large doses are required, as few as 20% of patients can initially tolerate niacin. However, with proper counseling, careful drug titration, and concomitant use of aspirin, this number can be increased to as high as 60% to 70%.
Ezetimibe (Zetia) is a cholesterol absorption inhibitor that acts on the cells in the small intestine to inhibit cholesterol absorption. It decreases cholesterol from dietary absorption, reducing serum cholesterol, LDL, triglycerides, and apoB levels. Ezetimibe causes only a small increase in HDL. It must be combined with a statin for optimum effect (ezetimibe and simvastatin [Zocor], marketed as Vytorin).
Statins
The statin drugs inhibit the enzyme HMG CoA reductase in cholesterol biosynthesis; thus the statins are called HMG CoA reductase inhibitors. By inhibiting cholesterol synthesis in the liver, this group of antihyperlipidemics decreases the concentration of cholesterol, decreases LDL, and slightly increases HDL cholesterol. Reduction of LDL cholesterol may be seen as early as 2 weeks after initiating therapy. The statin group has been useful in decreasing CAD and reducing mortality rates.
Numerous statins have been approved since they were first introduced. The present group of statins includes atorvastatin calcium (Lipitor), fluvastatin (Lescol), lovastatin (Mevacor), pravastatin sodium (Pravachol), simvastatin (Zocor), and rosuvastatin calcium (Crestor). Lovastatin was the first statin used to decrease cholesterol. It is effective in lowering LDL (hyperlipidemia type II) within several weeks. Gastrointestinal (GI) disturbances, headaches, muscle cramps, and fatigue are early complaints. With all statins, serum liver enzymes should be monitored, and an annual eye examination is needed, because cataract formation may result. The patient should report immediately any muscle aches or weakness, which can lead to rhabdomyolysis, a muscle disintegration that can become fatal.
The statins have actions in decreasing serum cholesterol, LDL, VLDL, and triglycerides, and they slightly elevate HDL. Atorvastatin, lovastatin, and simvastatin are more effective at lowering LDL than the other statins. Atorvastatin and simvastatin are at the top of the list of most prescribed drugs in the United States.
The statin drugs can be combined with other drugs to decrease blood pressure and blood clotting and to enhance the antihyperlipidemic effect. Examples are Advicor (lovastatin and niacin), Caduet (atorvastatin and amlodipine), Vytorin (simvastatin and ezetimibe), and Liptruzet (ezetimibe and atorvastatin). Table 46-4 lists these combination drugs and their dosages, uses, and considerations.
TABLE 46-4
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| Bile-Acid Sequestrants | ||
| cholestyramine (Questran, Prevalite) | A: PO: 4 g 1-2 times/d; mix powder in 120-240 mL of fluid; max: 24 g/d C >6 y: PO: 80 mg/kg/d t.i.d. | For type II hyperlipoproteinemia (LDL). Decrease in LDL apparent in 1 week. Mix powder well in 4-6 oz fluid. Has no effect on VLDL and HDL, but could increase triglyceride levels. GI upset and constipation can occur. Vitamin A, D, or K deficiency may occur because of decreased GI absorption. Pregnancy category: C; PB: UK;  : UK : UK |
| colesevelam (Welchol) | A: PO: 3 tabs (625 mg/tab) b.i.d. or 6 tabs/d with meals | Cholesterol-lowering effect achieved by binding with bile salts in intestines to form insoluble complex with fecal excretions, reducing circulating cholesterol, including LDL. Triglycerides may be slightly increased. Contraindicated with bowel obstruction. May be used in combination with a statin drug. Pregnancy category: B; PB: UK;  : UK : UK |
| colestipol HCl (Colestid) | A: PO: 5-20 g/d in divided doses; max: 30 g/d | To reduce cholesterol and LDL levels. Same as cholestyramine. Pregnancy category: C; PB: UK;  : UK : UK |
| Fibrates (Fibric Acid) | ||
| fenofibrate (TriCor) | A: PO: 48-145 mg/d; max: 148 mg/d | Treatment of type IV and V hyperlipidemia, and for hypertriglyceridemia. Specified diet should be part of drug therapy. Monitor serum creatinine levels. Pregnancy category: C; PB: 99%;  : 20 h : 20 h |
| gemfibrozil (Lopid) | A: PO: 600 mg b.i.d. 30 min before meals; max: 1,200 mg/d | For VLDL and elevated triglycerides; LDL may decrease, and HDL may increase. For types II (VLDL, LDL), III, IV, and V hyperlipidemia. Use in combination with lovastatin contraindicated because of increase in CPK. Pregnancy category: C; PB: 95%;  : 1.5 h : 1.5 h |
| Nicotinic Acid | ||
| niacin (nicotinic acid) (Niaspan) | A: PO: Initially: 250 mg/d; maint: 1.5-2 g/d with meals in 3 divided doses; max: 6 g/d | For VLDL and LDL: types II, III, IV, and V hyperlipidemia. Doses are 100 times higher than RDA to lower VLDL. Pregnancy category: C; PB: <20%;  : 45 min : 45 min |
| Cholesterol Absorption Inhibitors | ||
| ezetimibe (Zetia) | A/C >10 y: PO: 10 mg/d | Inhibits cholesterol absorption in small intestine. Reduces total cholesterol, LDL, and triglycerides. Increases HDL. Caution with liver dysfunction and elevated serum transaminase. Pregnancy category: C; PB: 90%;  : 22 h : 22 h |
| Statins (HMG-CoA Reductase Inhibitors) | ||
| atorvastatin calcium (Lipitor) | A: PO: 10-40 mg/d; max: 80 mg/d | Treatment of dyslipidemia and hypercholesterolemia. Monitor liver enzymes for elevation. Pregnancy category: X; PB 98%;  : 20-30 h : 20-30 h |
| fluvastatin sodium (Lescol) | A: PO: Initially: 20-40 mg h.s.; maint: 20-80 mg/d; max: 80 mg/d | Treatment of types IIA and IIB hyperlipidemia, total cholesterol, and elevated triglycerides. HDL slightly increased. Monitor liver function (liver enzymes). Pregnancy category: X; PB: 98%;  : 2.5 h : 2.5 h |
| lovastatin (Mevacor) | A: PO: 10-20 mg/d with evening meal; max: 80 mg/d | Controls cholesterol by inhibiting cholesterol synthesis. Decreases LDL, increases some HDL. Monitor liver enzymes. Pregnancy category: X; PB: 95%;  : 1-2 h : 1-2 h |
| pravastatin sodium (Pravachol) | A: PO: 10-80 mg/d; max: 80 mg/d | Decreases serum cholesterol, LDL, VLDL, and triglycerides. HDL slightly increased. Monitor liver enzymes. Pregnancy category: X; PB: 50%;  : 1.5-2.5 h : 1.5-2.5 h |
| rosuvastatin calcium (Crestor) | See Prototype Drug Chart 46-1. | |
| simvastatin (Zocor) | A: PO: 5-40 mg/d in evening; max: 40 mg/d | Similar to lovastatin. Monitor liver enzymes. Pregnancy category: X; PB: 95%;  : 2 h : 2 h |
| pitavastatin (Livalo) | A: PO: Initially 2 mg/d; maint: 1-4 mg/d; max: 4 mg/d | Moderate reduction of LDLs and only modest increase in HDLs. May cause rhabdomyolysis. Monitor liver enzymes and muscle pain. Pregnancy category: X; PB: 99%;  : 12 h : 12 h |
| Miscellaneous Antilipemics | ||
| icosapent ethyl (Vascepa) | A: PO: 2 g q12h; max: 4 g/d | For severe hypertriglyceridemia (triglyceride levels >500 mg/dL as an adjunct to diet. Monitor bleeding time for prolonged levels. Pregnancy category: C; PB: 99%;  : 89 h : 89 h |
| lomitapide (Juxtapid) | A: PO: 5 mg/d, may increase to 10 mg in 2 wks; max: 60 mg/d | For hypercholesterolemia. Most common adverse effects are GI disorders such as nausea, vomiting, abdominal pain, and diarrhea. Pregnancy category: X; PB: 99.8%;  : 39.7 h : 39.7 h |
| Omega 3 fatty acids (Lovaza) | A: PO: 4 g/d | For hypertriglyceridemia. Pregnancy category: C; PB: UK;  : UK : UK |
| Combination Anticholesterol Drugs | ||
| niacin and lovastatin (Advicor) | A: PO: 500 mg niacin/20 mg lovastatin Also available: 750 mg/20 mg; 1000 mg/20 mg; 1,000 mg/40 mg | Niacin raises HDL, triglycerides; lovastatin lowers LDL. Indicated for hypercholesterolemia and mixed dyslipidemia. |
| amlodipine and atorvastatin (Caduet) | A: PO: 2.5 mg amlodipine/20 mg atorvastatin/d; Also available: 2.5 mg/40 mg; 5 mg/10 mg to 5 mg/80 mg; 10 mg/10 mg to 10 mg/80 mg | Combination of calcium channel blocker and statin. Useful in treating hypertension and dyslipidemia. Helpful to patients who take these drugs separately. |
| ezetimibe/simvastatin (Vytorin) | A: PO: 10/10 mg to 10/80 mg | Combination of ezetimibe (Zetia) and simvastatin (Zocor). Ezetimibe decreases absorption of cholesterol in small intestine; simvastatin interferes with production of cholesterol in liver. |
| Ezetimibe and atorvastatin (Liptruzet) | A: PO: 10 mg daily | For hyperlipidemia. May cause increased ALT and AST. Pregnancy category: X; PB: 90%-98%;  : 14 h : 14 h |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


