Anticoagulants, Antiplatelets, and Thrombolytics
Objectives
• Compare the action for anticoagulants, antiplatelets, and thrombolytics.
• Apply the nursing process, including patient teaching, for anticoagulants and thrombolytics.
Key Terms
activated partial thromboplastin time, p. 651
acute myocardial infarction, p. 657
aggregation, p. 650
anticoagulants, p. 651
antiplatelets, p. 657
fibrinolysis, p. 659
international normalized ratio, p. 653
ischemia, p. 657
myocardial infarction, p. 651
necrosis, p. 657
partial thromboplastin time, p. 651
prothrombin time, p. 653
thromboembolism, p. 657
thrombolytics, p. 657
thrombosis, p. 650
Various drugs are used to maintain or restore circulation. The three major groups of these drugs are (1) anticoagulants, (2) antiplatelets (antithrombotics), and (3) thrombolytics. The anticoagulants prevent the formation of clots that inhibit circulation. The antiplatelets prevent platelet aggregation (clumping together of platelets to form a clot). The thrombolytics, popularly called clot busters, attack and dissolve blood clots that have already formed. Each of these three drug groups are discussed separately.
Pathophysiology: Thrombus Formation
Thrombosis is the formation of a clot in an arterial or venous vessel. The formation of an arterial thrombus could be caused by blood stasis (decreased circulation), platelet aggregation on the blood vessel wall, or blood coagulation. Arterial clots are usually made up of both white and red clots with the white clots (platelets) initiating the process, followed by fibrin formation and the trapping of red blood cells in the fibrin mesh. Blood clots found in the veins are from platelet aggregation with fibrin that attaches to red blood cells. Both types of thrombus can be dislodged from the vessel and become an embolus (blood clot moving through the bloodstream).
Platelets do not usually stick together unless there is a break in the endothelial lining of a blood vessel. When platelets adhere to the broken surface of an endothelial lining, they synthesize thromboxane A2, which is a product of prostaglandins and a potent stimulus for platelet aggregation (clumping of platelet cells). The platelet receptor protein that binds fibrinogen, known as glycoprotein IIb/IIIa, or GP IIb/IIIa, also promotes platelet aggregation. Thromboxane A2 and adenosine diphosphate (ADP) increase the activation of this receptor.
As the thrombus inhibits blood flow, fibrin, platelets, and red blood cells (erythrocytes) surround the clot, building the clot’s size and structure. As the clot occludes the blood vessel, tissue ischemia occurs.
The venous thrombus usually develops because of slow blood flow. The venous clot can occur rapidly. Small pieces of the venous clot can detach and travel to the pulmonary artery and then to the lung. Inadequate oxygenation and gas exchange in the lungs result.
Oral and parenteral anticoagulants (warfarin and heparin) act primarily to prevent venous thrombosis, whereas antiplatelet drugs act to prevent arterial thrombosis. However, both groups of drugs suppress thrombosis in general.
Anticoagulants
Anticoagulants are used to inhibit clot formation. Unlike thrombolytics, they do not dissolve clots that have already formed, but rather act prophylactically to prevent new clots from forming. Anticoagulants are used in patients with venous and arterial disorders that put them at high risk for clot formation. Venous problems include deep vein thrombosis (DVT) and pulmonary embolism, and arterial problems include coronary thrombosis, or myocardial infarction; presence of artificial heart valves; and cerebrovascular accidents (CVAs, or stroke).
Heparin
Anticoagulants are administered orally or parenterally (subcutaneously [subQ] and intravenously [IV]). Heparin, introduced in 1938, is a natural substance in the liver that prevents clot formation. It was first used in blood transfusions to prevent clotting. Heparin is indicated for rapid anticoagulant effect when a thrombosis occurs because of a deep vein thrombosis (DVT), pulmonary embolism (PE), or an evolving stroke. Heparin is also used in open-heart surgery to prevent blood from clotting and in the critically ill patient with disseminated intravascular coagulation (DIC). DIC occurs when fibrin clots form within the vascular system. These clots consume proteins and platelets, depleting clotting factors and causing excess bleeding. However, the primary use of heparin is to prevent venous thrombosis, which can lead to pulmonary embolism or stroke.
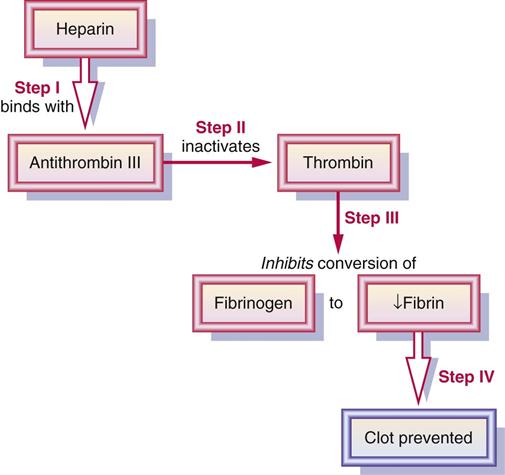
Heparin combines with antithrombin III, which accelerates the anticoagulant cascade of reactions that prevents thrombosis formation. By inhibiting the action of thrombin, conversion of fibrinogen to fibrin does not occur and the formation of a fibrin clot is prevented (Figure 45-1).
Heparin is poorly absorbed through the gastrointestinal (GI) mucosa, and much is destroyed by heparinase, a liver enzyme. Because heparin is poorly absorbed orally, it is given subQ for prophylaxis or IV to treat acute thrombosis. It can be administered as an IV bolus or in IV fluid for continuous infusion. Heparin prolongs clotting time. Partial thromboplastin time (PTT) and activated partial thromboplastin time (aPTT) are laboratory tests used to detect deficiencies of certain clotting factors, and these tests are used to monitor heparin therapy. Heparin can decrease the platelet count, causing thrombocytopenia. If hemorrhage occurs during heparin therapy, the anticoagulant antagonist protamine sulfate is given IV. Protamine sulfate can be an anticoagulant, but in the presence of heparin, it is an antagonist to reverse the action of heparin. Before discontinuing heparin, oral therapy with warfarin therapy is begun.
Low–Molecular-Weight Heparins
These derivatives of standard heparin were introduced to prevent venous thromboembolism. Studies have shown that by extracting only the low–molecular-weight fractions of standard heparin through depolymerization, the equivalent of anticoagulation can be achieved with a lower risk of bleeding. Low–molecular-weight heparins (LMWHs) produce more stable responses at recommended doses. As a result, frequent laboratory monitoring of aPTT is not required, because LMWH does not have the standard effect of heparin. Heparin prevents coagulation by combining with Antithrombin III to inactivate factor Xa and thrombin. Low–molecular-weight heparin inactivates the Xa factor, but it is less able to inactivate thrombin.
There are examples of LMWHs include enoxaparin sodium (Lovenox) and dalteparin sodium (Fragmin).
The anticoagulant fondaparinux (Arixtra) is a synthetically engineered antithrombotic designed to be effective as a once-daily subcutaneous injection. Categorized as a selective Factor Xa inhibitor, fondaparinux is closely related in structure to heparin and LMW heparins and is used for the same purposes.
These agents are most commonly prescribed to prevent DVT and acute pulmonary embolism after orthopedic or abdominal surgery. Hip- and knee-replacement anticoagulant therapy often includes enoxaparin, and abdominal surgery includes dalteparin. The drugs can be administered at home, because aPTT monitoring is not necessary, whereas heparin must be given in the hospital. LMWHs are administered subQ once or twice a day, depending on the drug or drug regimen, and are available in prefilled syringes with attached needles. The patient or family member is taught how to administer the subQ injection, which is usually given in the abdomen. The average treatment period lasts 7 to 10 days. The LMWH is usually started in the hospital within 24 hours after surgery (Table 45-1).
![]() TABLE 45-1
TABLE 45-1
ANTICOAGULANTS AND ANTICOAGULANT ANTAGONISTS
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| Anticoagulants | ||
| Heparins | ||
| heparin sodium | See Prototype Drug Chart 45-1. | |
| Low–Molecular-Weight Heparins (LMWHs) | ||
| dalteparin sodium (Fragmin) | Surgery: A: subQ: 2500 international units/d for 5-10 d starting 1-2 h before surgery DVT: A: subQ: 5000 units/d or q12h for 2-6 mo | For prevention of DVT before surgery and for those at risk of thromboembolism. Similar to enoxaparin. Pregnancy category: B; PB: <10%;  : 3-5 h : 3-5 h |
| enoxaparin sodium (Lovenox) | A: subQ: 40 mg daily for 5 to 10 d | For thromboembolism. Prevents and treats DVT and pulmonary embolism. Bleeding is an adverse reaction. Monitor CBC. Pregnancy category: B; PB: UK;  : 4.5 h : 4.5 h |
| Oral Anticoagulants | ||
| Coumarin | ||
| warfarin (Coumadin) | See Prototype Drug Chart 45-1. | |
| Selective Factor Xa Inhibitors | ||
| fondaparinux (Arixtra) | A: subQ: 2.5-10 mg/d for 5-9 d | Indirectly inhibits factor Xa, preventing blood clots. Closely related to heparin and LMWHs. Used to prevent DVT after hip fracture, hip replacement surgery, and knee replacement surgery and treat pulmonary emboli. May cause more bleeding than LMWHs. Long duration of action. Pregnancy category: B; PB: 94%;  : 17-21 h : 17-21 h |
| rivaroxaban (Xarelto) | A: PO: 10-20 mg once daily with evening meal; max: 30 mg/d | For prophylaxis of DVT and PE in patients undergoing knee or hip replacement surgery, stroke, and atrial fibrillation. Not easily reversed. Does not require routine coagulation monitoring. Pregnancy category: C; PB: 92%-95%;  : 5-9 h : 5-9 h |
| apixaban (Eliquis) | A: PO: 5 mg b.i.d. | To prevent stroke and thromboembolism associated with nonvalvular atrial fibrillation. Routine coagulation monitoring not required. Pregnancy category: B; PB: 87%;  : 5-12 h : 5-12 h |
| Direct-Acting Thrombin Inhibitors: Anticoagulants II (Intravenous) | ||
| argatroban (Argatroban) | A: IV: 2 mcg/kg/min; adjust dose to maintain aPTT 1.5-3 times baseline; max: 10 mcg/kg/min | Directly inhibits thrombin (thrombin inhibitor). Same effect as lepirudin. Decreases development of new thrombosis and treats heparin-induced thrombocytopenia (HIT). Pregnancy category: C; PB: 54%;  : 40-52 min : 40-52 min |
| bivalirudin (Angiomax) | A: IV bolus: 0.75 mg/kg; then IV infusion of 1.75 mg/kg/h during and within 4 h postprocedure; may require 0.2 mg/kg/h up to 20 h | Inhibits thrombin by binding to its receptor sites. Has been effective for use in preventing clot formation in patients with unstable angina who are undergoing cardiac angioplasty. Adverse effect is bleeding. Pregnancy category: B; PB: 0%;  : 25 min : 25 min |
| desirudin (Iprivask) | A: subQ: 15 mg/12 h for 9-12 d | Interferes with fibrin production, platelet aggregation, and factor XII activation, and inactivates thrombin. Given for DVT prophylaxis. Pregnancy category: C; PB: UK,  : 2-3 h : 2-3 h |
| lepirudin (Refludan) | A: IV bolus: 0.2-0.4 mg/kg over 15-20 sec; follow with 0.15 mg/kg/h for 2-10 d | Directly inhibits thrombin. Used for prophylaxis and treatment of thrombosis due to HIT. Titrated to aPTT ratio. Liver function should be normal. Adverse effect is bleeding. Pregnancy category: B; PB: UK;  : 1.3 h : 1.3 h |
| dabigatran (Pradaxa) | A: PO: 150 mg b.i.d.; max: 300 mg/d | For prevention of stroke and atrial fibrillation. Assess renal function before initiating drug and periodically throughout therapy. Pregnancy category: C; PB: 35%;  : 12-17 h : 12-17 h |
| Anticoagulant Antagonists | ||
| protamine sulfate | A: IV: Initially: 1 mg/100 units heparin; administer 10-50 mg in 10-15 min IV push; max: 100 mg in 2-h period | Binds and neutralizes heparin. Antidote to heparin overdose. Pregnancy category: C; PB: UK;  : 7.4 min : 7.4 min |
| phytonadione, Vitamin K1 (Mephyton) | A: PO/IM/IV: 1-10 mg, q12-24h PRN C: subQ/IM: 0.5-5 mg | Promotes liver synthesis of clotting factors. Antidote for warfarin overdose. Pregnancy category: C; PB: UK;  : UK : UK |
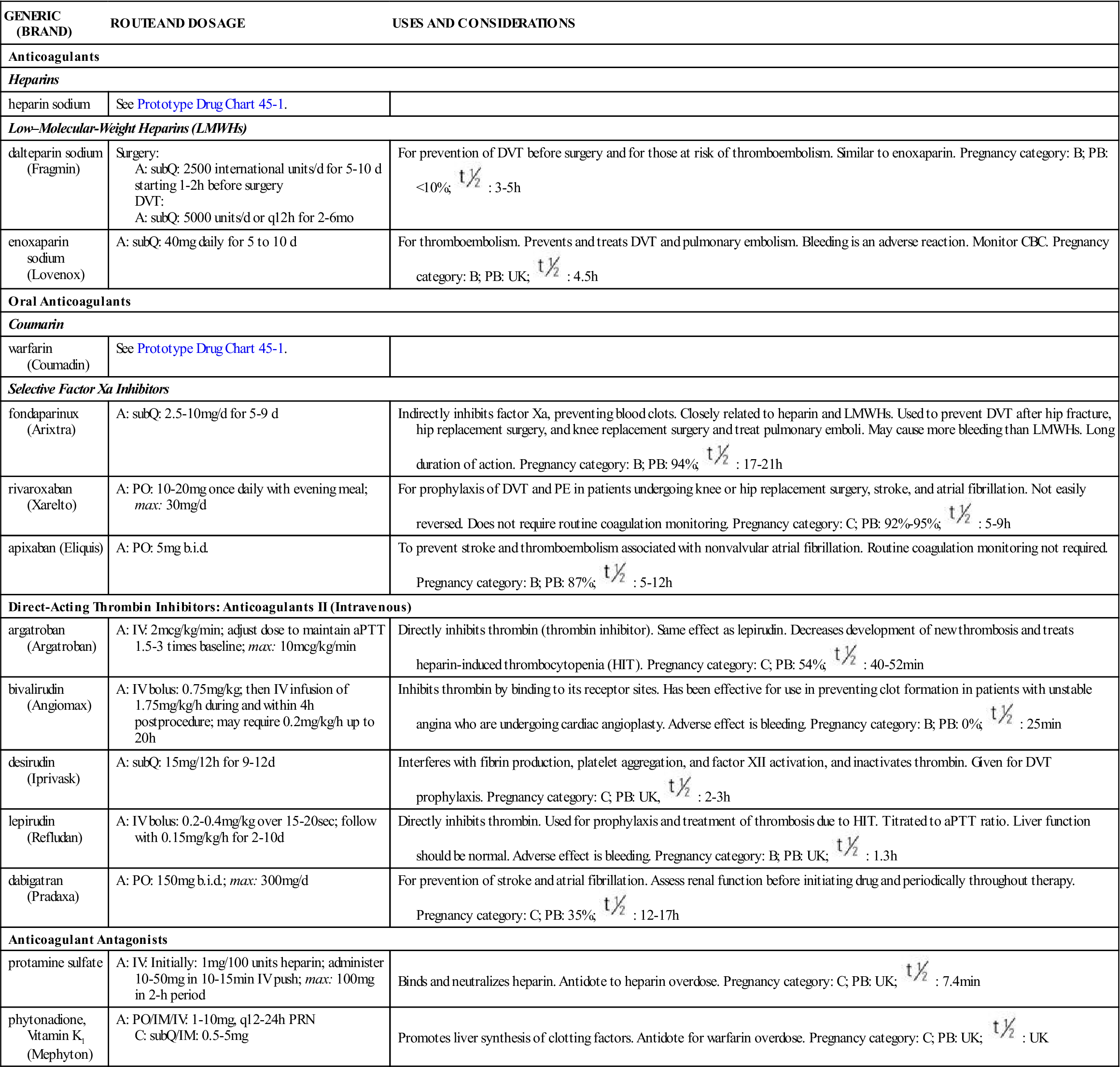
The half-life of LMWHs is two to four times longer than that of heparin. Patients should be instructed not to take antiplatelet drugs such as aspirin while taking LMWHs or heparin. Bleeding because of LMWH use is less likely to occur than when heparin is given. LMWH overdose is rare; if bleeding occurs, protamine sulfate is the anticoagulant antagonist used. The dosage is 1 mg of protamine sulfate for every 100 units of unfractionated heparin or LMWH given.
Contraindications
The LMWHs are contraindicated for patients with strokes, peptic ulcers, and blood anomalies. These drugs should not be given to patients having eye, brain, or spinal surgery.
Direct Thrombin Inhibitors: Parenteral Anticoagulants II
Parenteral anticoagulants directly inhibit thrombin from converting fibrinogen to fibrin. These drugs differ from heparin-like anticoagulants. Three of these drugs are given intravenously: argatroban (Acova), bivalirudin (Angiomax), and lepirudin (Refludan). Bivalirudin binds with and inhibits free-flowing thrombin. The fourth drug, desirudin (Iprivask), is administered subcutaneously. Dabigatran (Pradaxa) is an oral anticoagulant that does not require routine coagulation monitoring (see Table 45-1). These drugs are more expensive than the other anticoagulants.
Oral Anticoagulants
Warfarin (Coumadin) is an oral anticoagulant from the coumarin drug family. Dicumarol, a coumarin drug, and anisindione from the indanedione group, have been discontinued because of their many side effects. Warfarin is synthesized from dicumarol. Before warfarin was available for human use, it was used in rodenticides to kill rats by causing hemorrhage.
Oral anticoagulants inhibit hepatic synthesis of vitamin K, thus affecting the clotting factors II, VII, IX, and X. Warfarin is used mainly to prevent thromboembolic conditions such as thrombophlebitis, pulmonary embolism, and embolism formation caused by atrial fibrillation, which can lead to stroke (CVA). Oral anticoagulants prolong clotting time and are monitored by the prothrombin time (PT), a laboratory test that measures the time it takes blood to clot in the presence of certain clotting factors, which warfarin affects. This laboratory test is usually performed immediately before administering the next drug dose until the therapeutic level has been reached. Today, international normalized ratio (INR) is the laboratory test most frequently used to report PT results. It was introduced to account for variability in reported PTs from different laboratories. Reagents used in the PT test are compared with an international reference standard and reported as the INR; normal INR is 1.3 to 2. Patients on warfarin therapy are maintained at an INR of 2 to 3. The desired INR for patients who have a mechanical heart valve or recurrent systemic embolism is 2.5 to 3.5, but the desired level could be as high as 4.5.
Monitoring INR at regular intervals is required for the duration of drug therapy. Warfarin (Coumadin) has a long half-life and very long duration. Drug accumulation can occur and lead to external or internal bleeding, so the nurse must observe for petechiae, ecchymosis, tarry stools, and hematemesis and teach the patient to do the same at home.
The antidote for warfarin overdose is Vitamin K, but it takes 24 to 48 hours to be effective. Usually a low dose of oral Vitamin K may be recommended for patients with an INR of 5.5. If excessive Vitamin K is given, it may take warfarin 1 to 2 weeks before it can be effective again. For acute bleeding, fresh frozen plasma is indicated.
Parenteral and oral anticoagulants (heparin and warfarin) are presented in Prototype Drug Chart 45-1.
Pharmacokinetics
Heparin is poorly absorbed through the GI mucosa, and much is destroyed by heparinase, a liver enzyme. Heparin is given parenterally, either subcutaneously for prophylactic anticoagulant therapy or IV (bolus or continuous infusion) for an immediate response. Warfarin, an oral anticoagulant, is well absorbed through the GI mucosa; food will delay but not inhibit absorption.
The half-life of heparin is dose-related; high doses prolong the half-life. The half-life of warfarin is 1 to 7 days, in contrast to 0.5 to 2.5 hours for heparin. Because warfarin has a long half-life and is highly protein-bound, the drug can have cumulative effects. Bleeding can occur, especially if another highly protein-bound drug is administered together with warfarin. Kidney and liver disease prolong the half-life of both heparin and warfarin. Warfarin is metabolized to inactive metabolites that are excreted in urine and bile.
Pharmacodynamics
Heparin, administered for acute thromboembolic disorders, prevents thrombus formation and embolism. It has been effectively used to treat DIC, which causes multiple thrombi in small blood vessels. Warfarin is effective for long-term anticoagulant therapy. The PT level should be 1.5 to 2 times the reference value to be therapeutic, or INR should be 2.0 to 3.0. INR has effectively replaced the use of PT, because PT can vary from laboratory to laboratory and reagent to reagent. Higher INR levels (up to 3.5) are usually required for patients with prosthetic heart valves, cardiac valvular disease, and recurrent emboli. Heparin does not cross the placental barrier, unlike warfarin; warfarin use is not recommended during pregnancy.
Intravenous heparin has a rapid onset; its peak time of action is reached in minutes, and its duration of action is short. After an IV heparin dose, the patient’s clotting time will return to normal in 2 to 6 hours. SubQ heparin is more slowly absorbed through the blood vessels in fatty tissue. Warfarin (Coumadin) has a long onset of action, peak concentration, and duration of action, so drug accumulation may occur.
Table 45-2 gives the summary comparison between heparin and warfarin, including methods of administration, drug action, uses, contraindications, laboratory tests, side effects, adverse reactions, and antidotes.
TABLE 45-2
COMPARISON OF PARENTERAL AND ORAL ANTICOAGULANTS
| FACTORS TO CONSIDER | HEPARIN | WARFARIN (COUMADIN) |
| Methods of administration | Subcutaneously Intravenously | Primarily orally |
| Drug actions | Binds with antithrombin III, which inactivates thrombin and clotting factors, inhibiting fibrin formation | Inhibits hepatic synthesis of vitamin K, which decreases prothrombin and the clotting factors VII, IX, and X |
| Uses | Treatment of venous thrombosis, pulmonary embolism, thromboembolic complications (e.g., heart surgery, disseminated intravascular coagulation) | Treatment of deep vein thrombosis, pulmonary embolism, transient ischemic attack; prophylactic for cardiac valves |
| Contraindications/cautions | Hemophilia, peptic ulcer, severe (stage 3 or 4) hypertension, severe liver or renal disease, dissecting aneurysm | Hemophilia, peptic bleeding ulcer, blood dyscrasias, severe liver or kidney disease, acute myocardial infarction, alcoholism |
| Laboratory tests | PTT: 60-70 sec Anticoagulant therapeutic level: 1.5 to 2 × control in seconds | PT: 11-15 sec Anticoagulant therapeutic level: 1.25 to 2.5 × control in seconds |
| aPTT: 20-35 sec Anticoagulant: aPTT: 30-85 sec | INR: 1.3-2 Anticoagulant: INR 2-3 Prosthetic heart valves: INR up to 3.5 | |
| Side/adverse effects | Bleeding, hemorrhage, hematoma, severe hypotension | Bleeding, hemorrhage, GI bleeding, ecchymoses, hematuria |
| Antidote | Protamine sulfate: 1 mg per 100 units of heparin (see Table 45-1) | Vitamin K1 PO/subQ/IM/IV: 2.5-10 mg, C: subQ/IM: 5-10 mg Infant: 1 mg |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 , half-life; UK, unknown.
, half-life; UK, unknown. : heparin: 0.5-2.5 h; warfarin: 1-7 d
: heparin: 0.5-2.5 h; warfarin: 1-7 d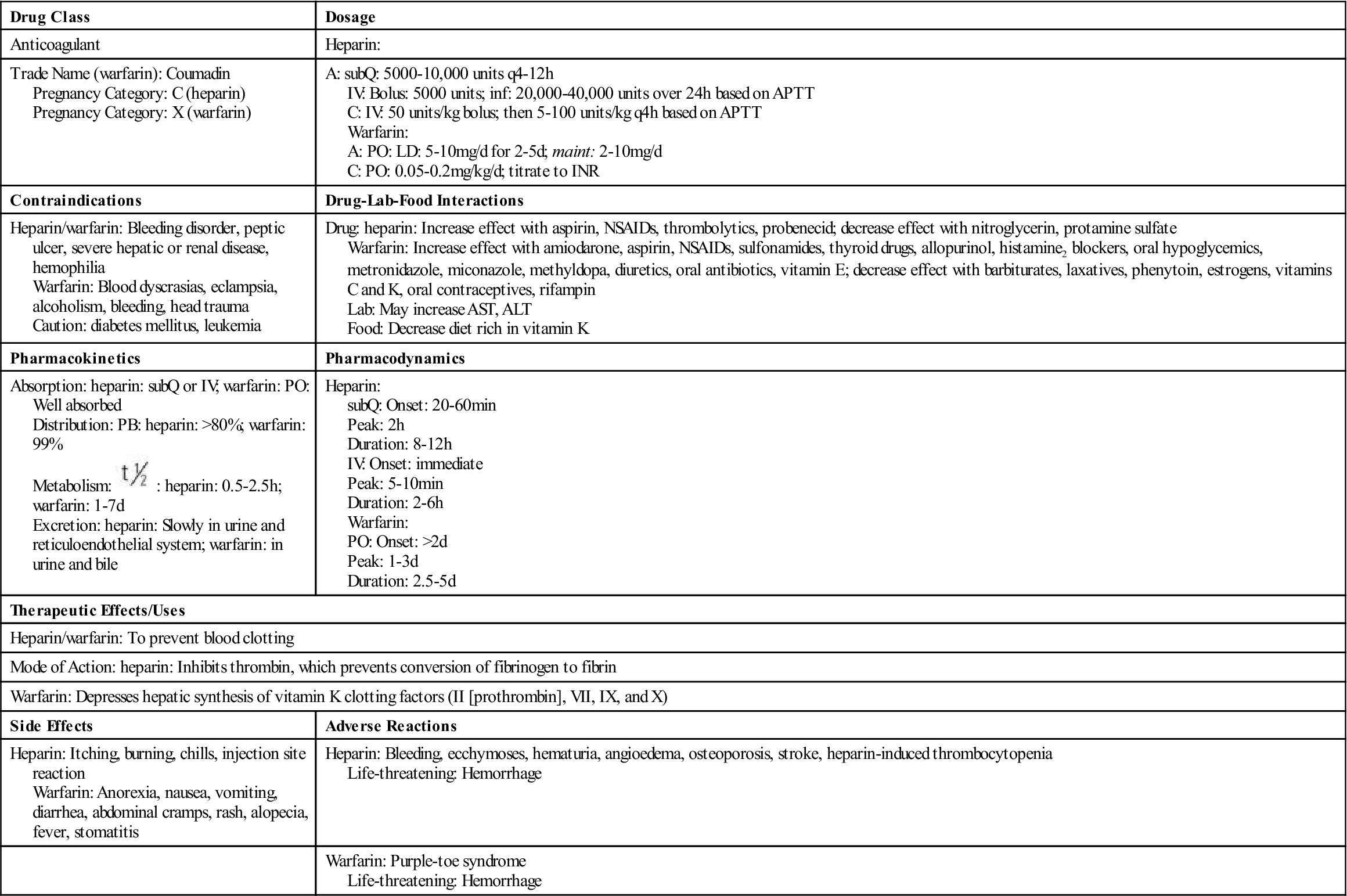
 , half-life, >, greater than.
, half-life, >, greater than.