Chapter 12 Anemias
Basic concepts
2 What are reticulocytes? What is a normal reticulocyte count?
Example: Assuming a severe anemia with a hematocrit of 10% and a reticulocyte count of 2.5%, we have
4 Regarding hemolytic anemia, what is the difference between intravascular and extravascular hemolysis?
5 Why is there a greater degree of hemoglobinemia and hemoglobinuria in intravascular hemolysis than in extravascular hemolysis?
In intravascular hemolysis, lysed RBCs spill their hemoglobin directly into the bloodstream (hemoglobinemia), which may then be filtered out into the urine (hemoglobinuria). In extravascular hemolysis, the hemoglobin in phagocytosed RBCs is metabolized intracellularly to bilirubin, reducing the amount of hemoglobin that ends up in the blood or urine (Table 12-1).
Table 12-1 Characteristics of Hemolysis
| Hematologic Feature | Intravascular Hemolysis | Extravascular Hemolysis |
|---|---|---|
| Hemoglobinemia | Yes | None or slight |
| Hemoglobinuria | Yes | None or slight |
| Plasma haptoglobin | Large decrease | Normal or slight decrease |
| Anemia | Yes | Yes |
| Jaundice | Yes | Yes |
| Hepatosplenomegaly | No | Often |
| Example disorders | Microangiopathic hemolytic anemia, disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, paroxysmal nocturnal hemoglobinuria | Immune-mediated (ABO mismatch), hypersplenism |
3 What are the three main types of hemoglobin found within normal adult red blood cells? How does this expression pattern differ in sickle cell anemia?
7 Why are parents of children with sickle cell disease taught how to palpate the spleen whenever their children develop a febrile illness?
11 This boy has one brother who does not have the disease. Neither of his parents are affected. How would you describe the genetics of this disease?
19 Patients with sickle cell disease can develop complications in many other organ systems as well. What two bone “diseases” are these patients predisposed to and why? To which other conditions are patients with sickle cell disease prone?
Other conditions affecting sickle cell patients include the following:
20 Some patients with sickle cell disease are treated with the chemotherapeutic drug hydroxyurea. What would be your rationale for starting this patient on this treatment?
21 What are sickle cell trait and Hemoglobin C (HbC)?
Summary Box: Sickle Cell Disease
 Sickle cell disease is inherited in an autosomal recessive manner.
Sickle cell disease is inherited in an autosomal recessive manner.
 Carriers of sickle cell trait are usually asymptomatic and are protected from falciparum malaria. Africans are more often affected.
Carriers of sickle cell trait are usually asymptomatic and are protected from falciparum malaria. Africans are more often affected.
 Examination may show scleral icterus, mild jaundice, and hepatosplenomegaly in patients younger than 5 years.
Examination may show scleral icterus, mild jaundice, and hepatosplenomegaly in patients younger than 5 years.
 Blood tests show normocytic anemia, reticulocytosis, and elevated indirect bilirubin.
Blood tests show normocytic anemia, reticulocytosis, and elevated indirect bilirubin.
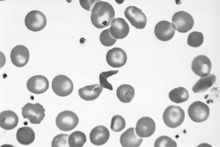
 Blood smear shows sickled cells, Howell-Jolly bodies, and reticulocytosis.
Blood smear shows sickled cells, Howell-Jolly bodies, and reticulocytosis.
 Hemoglobin electrophoresis shows hemoglobin S (HbS).
Hemoglobin electrophoresis shows hemoglobin S (HbS).
 Treatment includes hydroxyurea, pneumococcal and Haemophilus influenzae vaccines, and analgesia and hydration for treatment of acute crises.
Treatment includes hydroxyurea, pneumococcal and Haemophilus influenzae vaccines, and analgesia and hydration for treatment of acute crises.
 Sickle cell crises are precipitated by infection, dehydration, and hypoxemia.
Sickle cell crises are precipitated by infection, dehydration, and hypoxemia.
 Complications include the following:
Complications include the following:
6 Why do you see scleral icterus and organomegaly?
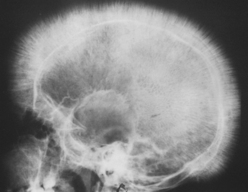
You may be given a radiograph of a skull that demonstrates a “crew cut” appearance (see Fig. 12-2). This is a sign of bone marrow expansion and is associated with thalassemia and sickle cell disease.
7 Why might this boy be more susceptible to fractures?
Ineffective erythropoiesis in the bone marrow results in markedly hyperplastic bone marrow and bone marrow expansion (Fig. 12-2). This bone marrow expansion erodes away the cancellous and cortical bone, resulting in significant structural weakness.