Anatomy and Physiology of the Respiratory System
QUICK LOOK AT THE CHAPTER AHEAD
The respiratory system provides several important functions:
Gas exchange
Humidification and filtration of air
Regulation of acid-base balance
Speech production
Taste and smell perception
The respiratory system is composed of the upper and lower respiratory tracts.
The lower respiratory tract consists of the trachea, bronchi, bronchioles, alveolar ducts, and alveoli.
The gas is exchanged in the respiratory system through pulmonary and alveolar ventilation, and it is influenced by gas pressures, air flow, perfusion, diffusion, compliance, and control of ventilation.
 CASE STUDY
CASE STUDYCode Blue! Room 622! Code Blue! Room 622!
Hearing those words over the intercom always perks up a nurse’s ears and attention. Everyone moves quickly to assure the best outcome for the patient. But much of what goes on during a code involves understanding the anatomy and physiology of the respiratory system. Let’s return to the code and watch the interventions of the staff.
Mrs. T is a 68-year-old woman who had a colectomy 2 days ago. The surgery was uncomplicated, but since her oxygen saturation levels were low postoperatively, she was receiving oxygen via nasal cannula at 4 liters (L) per minute. Her vital signs 1 hour ago were: blood pressure (BP)— 168/88 mmHg, pulse—92 beats per minute, respiration—24 breaths per minute, and her temperature was 100.8°F orally. Her prior medical history includes hypertension, obesity, and smoking one pack of cigarettes per day for 50 years. Mrs. T had just ambulated in the hall with the nursing assistant and felt short of breath, so she was returned to bed. The nursing assistant came to find the nurse to report Mrs. T’s symptoms. The nurse entered the room and found the patient unresponsive and not breathing. She called for help and began cardiopulmonary resuscitation (CPR). As the nurse positioned the patient’s head and listened for breathing, she watched the chest and did not observe any movement. She tried to deliver a breath but had difficulty ventilating the patient. She repositioned the head and was then able to deliver a breath and observe the chest rise and fall. As she checked for a carotid pulse, the anesthesiologist arrived and determined that Mrs. T needed to be intubated. The nurse felt for a carotid pulse and noted a faint pulse. Using the laryngoscope, the anesthesiologist visualized the vocal cords and inserted the endotracheal tube. After inflating the cuff on the tube, lungs were ventilated by manual inflation. Listening with the stethoscope, the anesthesiologist noted that there were no breath sounds on the left side of the chest.
Important Questions to Ask
Why did changing the position of the head allow the nurse to ventilate the patient?
If rescue breathing involves exhalation, why does it help to oxygenate the patient?
Why are the vocal cords visualized prior to intubation?
After intubation, why were breath sounds not heard on the left side of the chest?
The primary function of the respiratory system is gas exchange. In aerobic organisms, such as humans, oxygen is required for the production of energy. This efficient system provides the body with oxygen and removes carbon dioxide, the waste product of metabolism. The lungs provide an extensive area for the exchange of gases between air and circulating blood. The respiratory system also performs several secondary functions, including regulation of acid-base balance, humidification and filtration of air, speech production, and taste and smell perception.
 THE ANATOMY OF THE RESPIRATORY SYSTEM
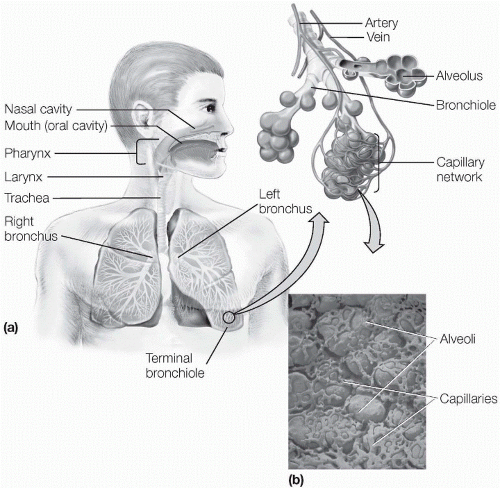
THE ANATOMY OF THE RESPIRATORY SYSTEMThe respiratory tract is divided into the upper and lower respiratory tracts (see Figure 1-1). The upper respiratory system includes the nasal cavities, the pharynx, and the larynx. The lower respiratory tract includes the trachea, bronchi, bronchioles, lungs, and alveoli. The lungs are encased in the thoracic cage and utilize multiple muscles, including the diaphragm and the intercostal muscles, to facilitate ventilation.
The Upper Respiratory Tract
The Nasal Cavities
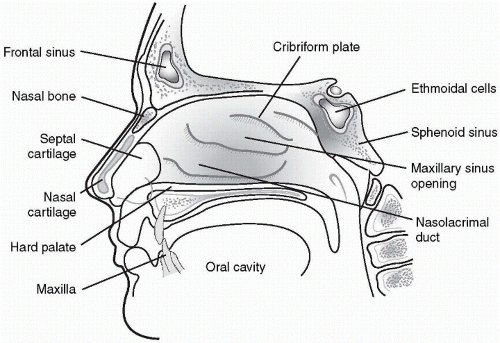
The nasal cavities or passages are the two sides of the nose divided by the nasal septum (see Figure 1-2). The upper third of the nose, the bridge, is bony while the lower third of the nose is cartilaginous. The nostrils (or nares), the two external openings to the nasal cavities, are lined with skin and hair follicles (vibrissae). The vibrissae are the first line of defense for filtering foreign objects and preventing them from being inhaled into the respiratory tract. The interior portion of the nasal passages and nasopharynx, which is the posterior aspect of the nasal cavities that connects with the pharynx, are lined with a mucous membrane that is well-supplied with blood. The mucous membrane serves to warm, filter, and humidify air. It is composed of columnar epithelial cells and goblet cells and produces mucus, which forms the mucociliary blanket. This blanket
protects the respiratory system by entrapping foreign particles and pathogens. Cilia are tiny hairlike projections that move the mucociliary blanket and its entrapped particles toward the oropharynx where they can either be expelled by coughing or sneezing or swallowed. Anatomically, the nasal passages make a 90° angle down into the oropharynx, allowing additional filtering of particles from inspired air.
protects the respiratory system by entrapping foreign particles and pathogens. Cilia are tiny hairlike projections that move the mucociliary blanket and its entrapped particles toward the oropharynx where they can either be expelled by coughing or sneezing or swallowed. Anatomically, the nasal passages make a 90° angle down into the oropharynx, allowing additional filtering of particles from inspired air.
The cribiform plate is inside the nasal passages, below the ethmoid bone. It is covered with mucous membrane and contributes to the sense of smell. This region is supplied by the first cranial nerve—the olfactory nerve—which passes through holes in the cribiform plate. Turbinates
are bony projections covered with mucous membrane along the sides of the nasal vestibule. The turbinates are highly vascular and serve to cleanse, warm, and humidify inspired air. They also increase the turbulence of inspired air, enhancing capture of particles in the mucociliary blanket.
are bony projections covered with mucous membrane along the sides of the nasal vestibule. The turbinates are highly vascular and serve to cleanse, warm, and humidify inspired air. They also increase the turbulence of inspired air, enhancing capture of particles in the mucociliary blanket.
 The mucous membranes serve to warm, filter, and humidify air. It is composed of columnar epithelial cells and goblet cells and produces mucus, which forms the mucociliary blanket. This blanket protects the respiratory system by entrapping foreign particles and pathogens.
The mucous membranes serve to warm, filter, and humidify air. It is composed of columnar epithelial cells and goblet cells and produces mucus, which forms the mucociliary blanket. This blanket protects the respiratory system by entrapping foreign particles and pathogens.The paranasal sinuses are hollow spaces in the facial bones surrounding the nasal passages. The sinuses are named for the bones in which they are located: sphenoid, ethmoid, and maxillary. The paranasal sinuses drain into the nasal cavities, as do the nasolacrimal ducts that drain tears from the surface of the eyes.
The Pharynx
The pharynx is located on the posterior aspect of the oral and nasal cavities and extends down to the larynx (see Figure 1-3). This tunnel-shaped
passageway is shared by the respiratory and digestive systems. It is divided into three parts:
passageway is shared by the respiratory and digestive systems. It is divided into three parts:
The nasopharynx, located above the margin of the soft palate
The oropharynx, located behind the tongue
The openings for the eustachian tubes are located on either side of the oropharynx. The lingual, palatine, and pharyngeal tonsils are nubs of lymphatic tissue in the pharynx. The mouth serves as an alternative airway
when either the nasal passages are obstructed or when high volumes of air are needed, such as during exercise. The mouth is less efficient at humidifying, filtering, and warming air than the nose. The pharynx is the only opening from the nasal passages and the mouth to the lungs, so that any obstruction of the pharynx immediately impairs ventilation.
when either the nasal passages are obstructed or when high volumes of air are needed, such as during exercise. The mouth is less efficient at humidifying, filtering, and warming air than the nose. The pharynx is the only opening from the nasal passages and the mouth to the lungs, so that any obstruction of the pharynx immediately impairs ventilation.
The epiglottis is a thin, leaf-shaped structure of elastic cartilage that helps to protect the larynx during swallowing (see Figure 1-4). The epiglottis covers the larynx during swallowing to prevent food and fluids from entering the lungs. The closed vocal cords are the final lines of defense for the lungs. At the point where the epiglottis covers the larynx, the pharynx divides into the larynx and the esophagus.
 The pharynx is the only opening from the nasal passages and the mouth to the lungs, so that any obstruction of the pharynx immediately impairs ventilation.
The pharynx is the only opening from the nasal passages and the mouth to the lungs, so that any obstruction of the pharynx immediately impairs ventilation.The Larynx
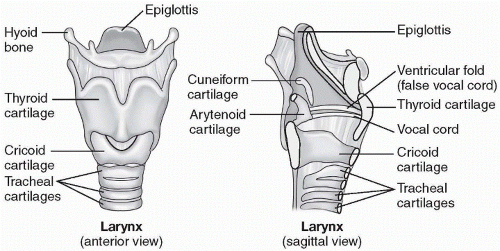
The larynx, commonly called the voice box, connects the pharynx with the trachea (see Figure 1-5). The larynx has two purposes:
Production of sound and speech
Protection of lungs from entrance by substances other than air
The larynx lies in the midline of the neck and contains two folds of mucous membrane known as the vocal cords. Vibration of the tightened vocal cords allows phonation to occur. The arytenoid cartilage is used in vocal cord movement. The epiglottis is attached at the top of the larynx. The esophagus is just posterior to the larynx. Should anything other than air enter the larynx, the cough reflex and laryngeal spasms would reflexively try to expel it. The epiglottis is essential in creating the cough reflex. Nine cartilage rings form the larynx; the largest of which, the thyroid cartilage, is sometimes called the Adam’s apple. The cricoid cartilage, that lies below the thyroid cartilage, contains the vocal cords. The cricothyroid membrane connects the cricoid and thyroid cartilage and may be incised for emergency access to the airway.
 The cricothyroid membrane connects the cricoid and thyroid cartilage and may be incised for emergency access to the airway.
The cricothyroid membrane connects the cricoid and thyroid cartilage and may be incised for emergency access to the airway.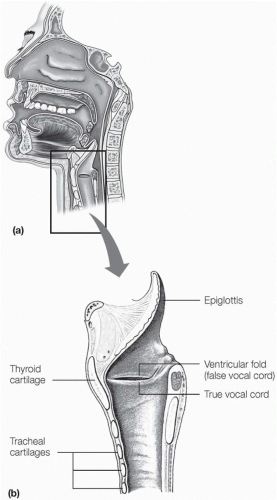 Figure 1-4 The vocal cords. (a) Uppermost portion of respiratory system showing location of the vocal cords. (b) Longitudinal section of the larynx showing the location of the vocal cords. Note the presence of the false vocal cord, so named because it does not function in phonation. |
The Lower Respiratory Tract
The lower respiratory tract consists of the trachea, the two mainstem bronchi, lobar, segmental and subsegmental bronchi, bronchioles, alveolar ducts, and alveoli. The tracheobronchial tree can be viewed as a system of branching tubes, each smaller, carrying air to the site of gas exchange: the alveolar membrane. There are about 23 levels of branching from the trachea down to the alveoli. Smooth muscle is wound about all the structures of the lower respiratory tract and constricts airways in disorders such as asthma.
 Smooth muscle is wound about all the structures of the lower respiratory tract and constricts airways in disorders such as asthma.
Smooth muscle is wound about all the structures of the lower respiratory tract and constricts airways in disorders such as asthma.The Trachea
The trachea or windpipe is a flexible tube that connects the larynx with the major bronchi of the lungs. It begins at the lower border of the cricoid cartilage and extends down to the level of the posterior fifth or sixth thoracic vertebrae or the anterior sternal angle, where it branches into the left and right mainstem bronchi. The site of this bifurcation is referred to as the carina. The strongest cough reflex is at the carina. Tracheobronchial suctioning may stimulate vigorous coughing if the carina is stimulated. The walls of the trachea contain about 20 horseshoe-shaped cartilages that stiffen the trachea, preventing collapse or expansion of the trachea
when intrathoracic pressures change. The cartilages are open posteriorly to allow stretching of the esophagus when a bolus of food passes. The walls of the trachea are composed of mucus-secreting, ciliated cells (the mucociliary blanket) that carry particles away from the lungs and up to the pharynx. These ciliated cells are destroyed by smoking, resulting in the loss of this valuable function.
when intrathoracic pressures change. The cartilages are open posteriorly to allow stretching of the esophagus when a bolus of food passes. The walls of the trachea are composed of mucus-secreting, ciliated cells (the mucociliary blanket) that carry particles away from the lungs and up to the pharynx. These ciliated cells are destroyed by smoking, resulting in the loss of this valuable function.
The Bronchi and Bronchioles
The right and left mainstem bronchi begin at the carina. These bronchi are similar in structure to the trachea, with cartilage surrounding the airway and maintaining the shape. Smooth muscle, controlled by the parasympathetic nervous system, wraps around the bronchi. The right mainstem bronchus is more like a linear extension of the trachea and is shorter and anatomically more vertically downward than the left. Therefore, aspirated foreign bodies and even accidental intubations are more likely to occur in the right mainstem bronchus.
The bronchioles spread in an inverted treelike formation throughout each lung. The segmental and subsegmental bronchi further branch into smaller and smaller bronchioles until they reach the terminal bronchioles. These bronchioles are only about 1 mm in diameter. They do not have cartilage rings and therefore depend on the elastic recoil of the lungs to maintain patency. They do not have cilia or participate in gas exchange.
 The right mainstem bronchus is more like a linear extension of the trachea and is shorter and anatomically more vertically downward than the left. Therefore, aspirated foreign bodies and even accidental intubations are more likely to occur in the right mainstem bronchus.
The right mainstem bronchus is more like a linear extension of the trachea and is shorter and anatomically more vertically downward than the left. Therefore, aspirated foreign bodies and even accidental intubations are more likely to occur in the right mainstem bronchus.The Alveoli
The alveoli are cup-shaped structures that are grouped like clusters of grapes at the end of the terminal bronchioles (see Figure 1-6). There are
150 to 300 million alveolar sacs in an adult’s lungs. Thin walls separate the alveoli from each other, and within the walls is an extensive network of capillaries that is so dense that it has been referred to as a sheet of blood. It is within these walls that the actual gas exchange takes place. Oxygen in the alveoli diffuses across the alveolar membrane into the blood, and carbon dioxide in the blood diffuses back into the alveoli (see Figure 1-7). Surfactant, a phospholipid protein, is secreted by cells called type II pneumocytes within the alveoli. Surfactant reduces the surface tension in the alveoli, allowing more surface area for gas exchange and preventing collapse of the alveolar sac. Lack of surfactant may cause respiratory failure in premature infants and has also been implicated in adult respiratory distress syndrome (ARDS). As there are no mucus-secreting glands in the alveoli, the majority of particle removal is done by alveolar macrophages and the lymphatic channels of the lungs.
150 to 300 million alveolar sacs in an adult’s lungs. Thin walls separate the alveoli from each other, and within the walls is an extensive network of capillaries that is so dense that it has been referred to as a sheet of blood. It is within these walls that the actual gas exchange takes place. Oxygen in the alveoli diffuses across the alveolar membrane into the blood, and carbon dioxide in the blood diffuses back into the alveoli (see Figure 1-7). Surfactant, a phospholipid protein, is secreted by cells called type II pneumocytes within the alveoli. Surfactant reduces the surface tension in the alveoli, allowing more surface area for gas exchange and preventing collapse of the alveolar sac. Lack of surfactant may cause respiratory failure in premature infants and has also been implicated in adult respiratory distress syndrome (ARDS). As there are no mucus-secreting glands in the alveoli, the majority of particle removal is done by alveolar macrophages and the lymphatic channels of the lungs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access