Adrenergic Agonists and Adrenergic Blockers
Objectives
• Explain major responses to stimulation of adrenergic receptors.
• Differentiate between selective and nonselective adrenergic agonists.
• Contrast the uses of alpha blockers and beta blockers.
• Compare general side effects of adrenergic agonists and adrenergic blockers.
• Apply the nursing process for the patient taking beta-adrenergic blockers.
• Compare the indications of adrenergic agonists and adrenergic blockers.
Key Terms
adrenergic blockers, p. 262
adrenergic neuron blockers, p. 263
adrenergic receptor, p. 255
alpha blockers, p. 262
beta blockers, p. 263
catecholamines, p. 258
nonselective, p. 258
selective, p. 258
sympatholytics, p. 255
sympathomimetics, p. 255
This chapter discusses two groups of drugs that affect the sympathetic nervous system: adrenergic agonists (sympathomimetics) and adrenergic blockers (sympatholytics), along with their dosages and uses.
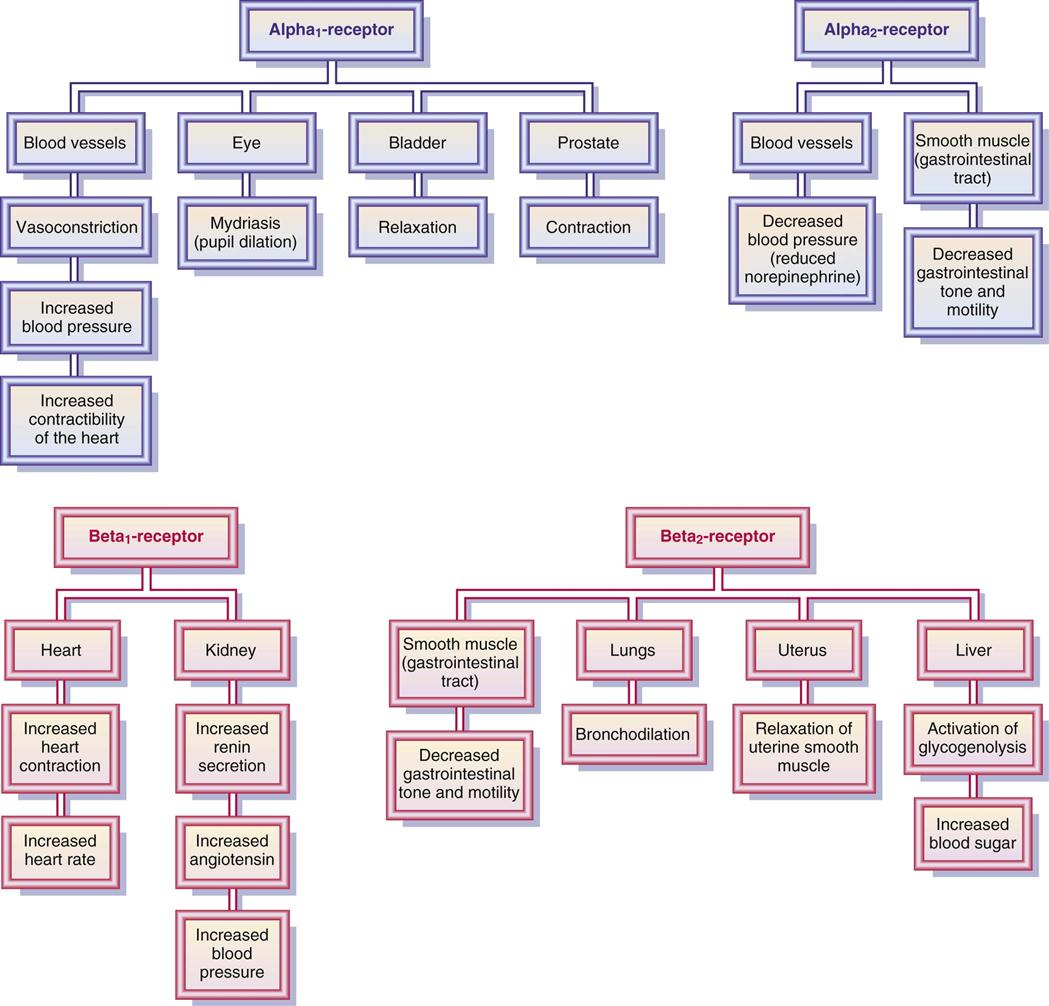
Adrenergic Agonists
Drugs that stimulate the sympathetic nervous system are called adrenergics, adrenergic agonists, or sympathomimetics, because they mimic the sympathetic neurotransmitters norepinephrine and epinephrine. They act on one or more adrenergic receptor sites located in the effector cells of muscles, such as the heart, bronchiole walls, gastrointestinal (GI) tract, urinary bladder, and ciliary muscle of the eye. There are many adrenergic receptors. The four main receptors are alpha1, alpha2, beta1, and beta2, which mediate the major responses described in Table 18-1 and illustrated in Figure 18-1.
TABLE 18-1
EFFECTS OF ADRENERGIC AGONISTS AT RECEPTORS
| RECEPTOR | PHYSIOLOGIC RESPONSES |
| Alpha1 | Increases force of heart contraction; vasoconstriction increases blood pressure; mydriasis (dilation of pupils) occurs; decreases secretion in salivary glands; increases urinary bladder relaxation and urinary sphincter contraction |
| Alpha2 | Inhibits release of norepinephrine; dilates blood vessels; produces hypotension; decreases gastrointestinal motility and tone |
| Beta1 | Increases heart rate and force of contraction; increases renin secretion, which increases blood pressure |
| Beta2 | Dilates bronchioles; promotes gastrointestinal and uterine relaxation; promotes increase in blood sugar through glycogenolysis in liver; increases blood flow in skeletal muscles |
The alpha-adrenergic receptors are located in blood vessels, eye, bladder, and prostate. When the alpha1 receptors in vascular tissues (vessels) of muscles are stimulated, the arterioles and venules constrict, increasing peripheral resistance and blood return to the heart. Circulation is improved, and blood pressure is increased. When there is too much stimulation, blood flow is decreased to the vital organs.
The alpha2 receptors are located in the postganglionic sympathetic nerve endings. When stimulated, they inhibit the release of norepinephrine, leading to a decrease in vasoconstriction. This results in vasodilation and a decrease in blood pressure.
The beta1 receptors are located in the kidney but primarily in the heart. Stimulation of the beta1 receptor increases myocardial contractility and heart rate.
The beta2 receptors are found mostly in the smooth muscles of the lung and gastrointestinal tract, the liver, and the uterine muscle. Stimulation of the beta2 receptor causes (1) relaxation of the smooth muscles of the lungs, resulting in bronchodilation; (2) a decrease in gastrointestinal tone and motility; (3) activation of glycogenolysis in the liver and increased blood glucose; and (4) relaxation of the uterine muscle, resulting in a decrease in uterine contraction (Figure 18-2; see also Table 18-1).
Another adrenergic receptor is dopaminergic and is located in the renal, mesenteric, coronary, and cerebral arteries. When this receptor is stimulated, the vessels dilate and blood flow increases. Only dopamine can activate this receptor.
Inactivation of Neurotransmitters
After the neurotransmitter (e.g., norepinephrine) has performed its function, the action must be stopped to prevent prolonging the effect. Transmitters are inactivated by (1) reuptake of the transmitter back into the neuron (nerve cell terminal), (2) enzymatic transformation or degradation, and (3) diffusion away from the receptor. The mechanism of norepinephrine reuptake plays a more important role in inactivation than the enzymatic action. Following the reuptake of the transmitter in the neuron, the transmitter may be degraded or reused. The two enzymes that inactivate norepinephrine are (1) monoamine oxidase (MAO), which is inside the neuron; and (2) catechol-O-methyltransferase (COMT), which is outside of the neuron.
Drugs can prolong the action of the neurotransmitter (e.g., norepinephrine) by either (1) inhibiting the norepinephrine reuptake, which prolongs the action of the transmitter or (2) inhibiting the degradation of norepinephrine by enzyme action.
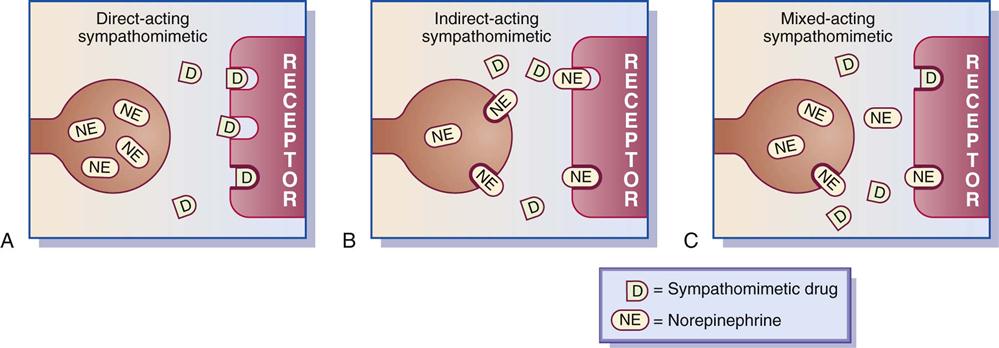
Classification of Sympathomimetics
The sympathomimetic drugs that stimulate adrenergic receptors are classified into three categories according to their effects on organ cells. Categories include (1) direct-acting sympathomimetics, which directly stimulate the adrenergic receptor (e.g., epinephrine or norepinephrine); (2) indirect-acting sympathomimetics, which stimulate the release of norepinephrine from the terminal nerve endings (e.g., amphetamine); and (3) mixed-acting sympathomimetics (both direct and indirect acting), which stimulate the adrenergic receptor sites and stimulate the release of norepinephrine from the terminal nerve endings (e.g., ephedrine) (Figure 18-3).![]()
Pseudoephedrine is an example of a mixed-acting sympathomimetic. This drug acts indirectly by stimulating the release of norepinephrine from the nerve terminals and acts directly on the alpha1 and beta1 receptors. Pseudoephedrine, like epinephrine, increases heart rate. It is not as potent a vasoconstrictor as epinephrine, and there is less risk of hemorrhagic stroke and hypertensive crisis. Pseudoephedrine is helpful to relieve nasal and sinus congestion without rebound congestion.
Catecholamines are the chemical structures of a substance (either endogenous or synthetic) that can produce a sympathomimetic response. Examples of endogenous catecholamines are epinephrine, norepinephrine, and dopamine. The synthetic catecholamines are isoproterenol and dobutamine. Noncatecholamines (e.g., phenylephrine, metaproterenol, albuterol) stimulate the adrenergic receptors. Most noncatecholamines have a longer duration of action than the endogenous or synthetic catecholamines.
Many of the adrenergic agonists stimulate more than one of the adrenergic receptor sites. An example is epinephrine (Adrenalin), which acts on alpha1-, alpha 2–, beta1-, and beta2-adrenergic receptor sites. The responses from these receptor sites include increase in blood pressure, pupil dilation, increase in heart rate (tachycardia), and bronchodilation. In anaphylactic shock, epinephrine is useful because it increases blood pressure, heart rate, and airflow through the lungs. Because epinephrine affects different adrenergic receptors, it is nonselective. Additional side effects result when more responses occur than are desired. Pseudoephedrine, ephedrine, and phenylpropanolamine are commonly used for illegal production of amphetamine and methamphetamine. These drugs are considered OTC drugs but may be obtained in limited amounts per month. Stores are required to keep these drugs behind the counter or in a locked cabinet and keep a log of purchases for at least 2 years. Prototype Drug Chart 18-1 lists the pharmacologic behavior of epinephrine.
Epinephrine
Pharmacokinetics
Epinephrine can be administered subcutaneously, intravenously, topically, or by inhalation, intracardiac, and instillation methods. It is not given orally, because it is rapidly metabolized in the GI tract and liver resulting in unstable serum levels. The percentage by which the drug is protein-bound and its half-life are unknown. Epinephrine is metabolized by the liver and excreted in the urine.
Pharmacodynamics
Epinephrine is frequently used in emergencies to treat anaphylaxis, which is a life-threatening allergic response. Epinephrine is a potent inotropic (strengthens myocardial contraction) drug that increases cardiac output, promotes vasoconstriction and systolic blood pressure elevation, increases heart rate, and produces bronchodilation. High doses can result in cardiac dysrhythmias necessitating electrocardiogram (ECG) monitoring. Epinephrine can also cause renal vasoconstriction, thereby decreasing renal perfusion and urinary output.
The onset of action and peak concentration times are rapid. The use of decongestants with epinephrine has an additive effect. When epinephrine is administered with digoxin, cardiac dysrhythmias may occur. Beta blockers can antagonize the action of epinephrine. Tricyclic antidepressants and monoamine oxidase inhibitors (MAOIs) allow epinephrine’s effects to be intensified and prolonged. Epinephrine is also discussed in Chapter 59 as one of the drugs used during emergencies.
Albuterol
Albuterol sulfate (Proventil), a beta2-adrenergic agonist, is selective for beta2-adrenergic receptors, so the response is relaxation of bronchial smooth muscle and bronchodilation. A patient with asthma may tolerate albuterol better than isoproterenol (which activates beta1 and beta2 receptors) because albuterol’s action is more selective (activates only the beta2 receptors). By using selective sympathomimetics, fewer undesired adverse effects will occur. However, high dosages of albuterol may affect beta1 receptors, causing an increase in heart rate. Prototype Drug Chart 18-2 lists the drug data related to albuterol.
Pharmacokinetics
Albuterol sulfate (Proventil, Ventolin) is well absorbed from the GI tract and is extensively metabolized by the liver. The half-life of the drug differs slightly according to the route of administration (oral route is 2.7 to 6 hours; inhalation route is 3.5 hours).
Pharmacodynamics
The primary use of albuterol is to prevent and treat bronchospasm. With inhalation, the onset of action of albuterol is faster than with oral administration, though the duration of action is the same for both oral and inhalation preparations.
Tremors, restlessness, and nervousness may occur when albuterol is taken. Tremors and nervousness are the most common side effects of oral or inhalation albuterol. If albuterol is taken with an MAOI, hypertensive crisis can result. Beta blockers may inhibit the action of albuterol. Albuterol and the beta2 drugs are also discussed in Chapter 41 and 44, respectively.
Central-Acting Alpha Agonists
Clonidine and Methyldopa
Clonidine (Catapres) is a selective alpha2-adrenergic agonist (sympathomimetic) used primarily to treat hypertension. Alpha2 drugs act by decreasing the release of norepinephrine from sympathetic nerves and decreasing peripheral adrenergic receptor activation. Alpha2 drugs also produce vasodilation by stimulating alpha2 receptors in the central nervous system (CNS), leading to a decrease in blood pressure (see Chapter 44).
Methyldopa (Aldomet) is an alpha-adrenergic agonist (sympathomimetic) that acts within the CNS. This drug is taken up into the brainstem neurons and converted to methylnorepinephrine, which is an alpha2-adrenergic agonist that leads to alpha2 activation. The decrease of sympathetic outflow from the CNS causes vasodilation and a reduction in blood pressure (see Chapter 44).
Side Effects and Adverse Reactions
Additional undesired side effects frequently result when the drug dosage is increased or the drug is nonselective. Side effects commonly associated with adrenergic agonists include hypertension, tachycardia, palpitations, restlessness, tremors, dysrhythmias, dizziness, urinary retention, nausea, vomiting, dyspnea, and pulmonary edema.
Names of adrenergic drugs, the receptors they activate, dosage information, and common uses are listed in Table 18-2.

 : UK
: UK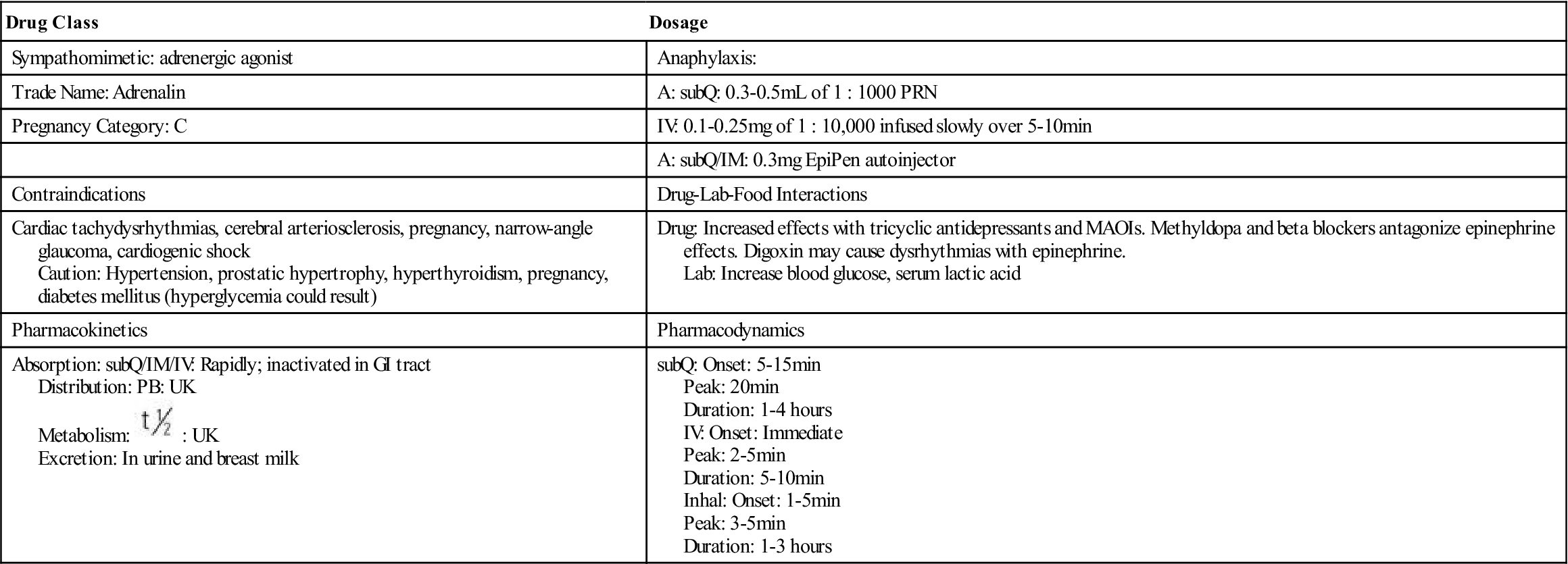
 , half-life; UK, unknown.
, half-life; UK, unknown. : PO: 2.7-6 h; Inhal: 3.5 h
: PO: 2.7-6 h; Inhal: 3.5 h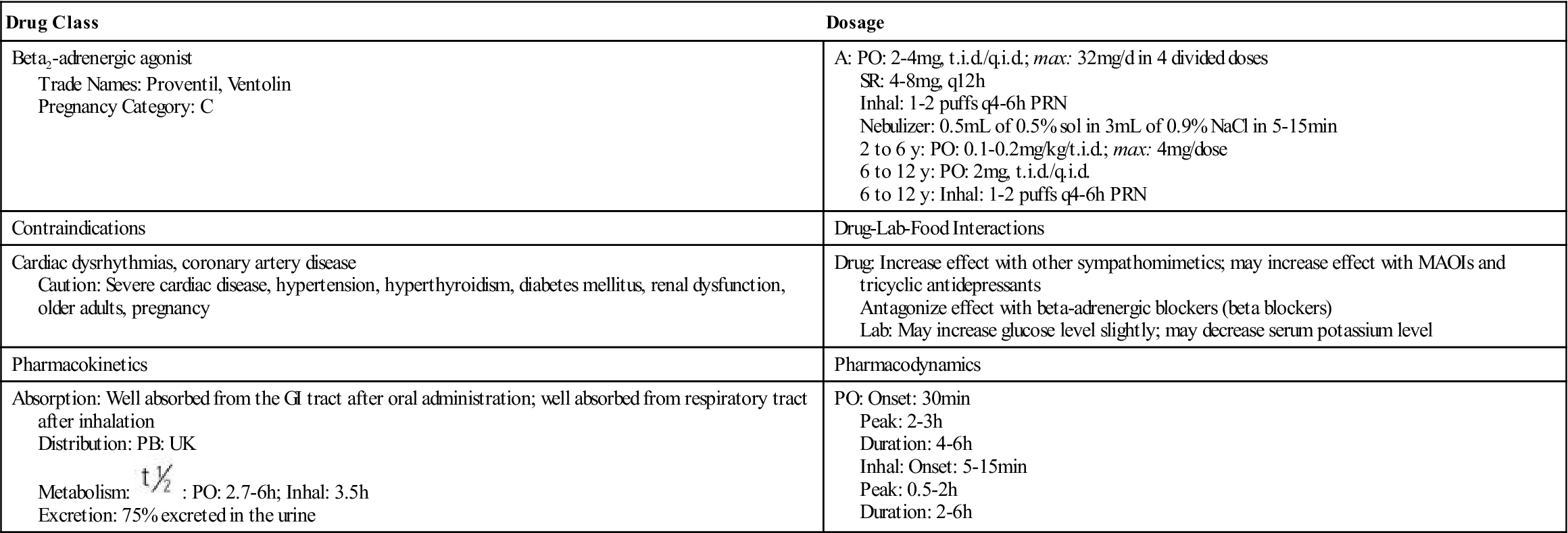
 , half-life; t.i.d., three times a day; UK, unknown; y, year.
, half-life; t.i.d., three times a day; UK, unknown; y, year.






