Barbara Lauritsen Christensen
Care of the patient with a gallbladder, liver, biliary tract, or exocrine pancreatic disorder
Objectives
3. Discuss specific complications and teaching content for the patient with cirrhosis of the liver.
4. Define jaundice and describe signs and symptoms that may occur with jaundice.
5. State the six types of viral hepatitis, including their modes of transmission.
6. List the subjective and objective data for the patient with viral hepatitis.
8. Discuss the two methods of surgical treatment for cholecystitis and cholelithiasis.
Key terms
asterixis ( s-t
s-t r-
r- K-s
K-s s, p. 240)
s, p. 240)
esophageal varices ( -s
-s f-
f- -J
-J –
– l V
l V R-
R- -s
-s z, p. 238)
z, p. 238)
flatulence (FL T-
T- -l
-l ns, p. 249)
ns, p. 249)
hepatic encephalopathy (h -P
-P T-
T- k
k  n-s
n-s f-
f- -L
-L P-
P- -th
-th , p. 240)
, p. 240)
hepatitis (h -p
-p -T
-T -t
-t s, p. 234)
s, p. 234)
paracentesis (p r-
r- -s
-s n-T
n-T -s
-s s, p. 237)
s, p. 237)
parenchyma (p -r
-r ng-K
ng-K -m
-m , p. 236)
, p. 236)
spider telangiectases (SP -d
-d r t
r t l-
l- n-j
n-j –
– K-t
K-t -s
-s z, p. 236)
z, p. 236)
steatorrhea (st –
– -t
-t -R
-R –
– , p. 249)
, p. 249)
This chapter discusses disorders of the accessory organs of digestion—namely the liver, the gallbladder, and the exocrine pancreas. These organs assist in digestion in various ways. See Chapter 5 for a review of the anatomy and physiology of the liver, the biliary tract, the gallbladder, and the pancreas.
Laboratory and diagnostic examinations in the assessment of the hepatobiliary and pancreatic systems
Serum bilirubin test
Rationale
Total serum bilirubin determination measures both direct, or conjugated (water-soluble), and indirect, or unconjugated (water-insoluble), bilirubin. Total serum bilirubin level is the sum of the direct and indirect bilirubin levels. Testing for bilirubin in the blood provides valuable information for diagnosis and evaluation of liver disease, biliary obstruction, and hemolytic anemia. Jaundice, the discoloration of body tissues caused by abnormally high blood levels of bilirubin, is visible when the total serum bilirubin exceeds 2.5 mg/dL.
Nursing interventions
Keep the patient on nothing by mouth (NPO) status until after the blood specimen is drawn.
Liver enzyme tests
The normal values are as follows:
Rationale
The liver is a storehouse of many enzymes. Injury or diseases affecting the liver cause release of these intracellular enzymes into the bloodstream, and their levels become elevated. Some of these enzymes are also produced in other organs, and injury or disease affecting these organs will raise the serum level. Therefore, although elevation of these serum enzymes is found in pathologic liver conditions, the test is not specific for liver diseases alone.
Nursing interventions
Assess the venipuncture site for bleeding.
Serum protein test
The normal values are as follows:
Rationale
One way to assess the liver’s functional status is to measure the products it synthesizes. One of these products is protein, especially albumin. When disease affects the liver cell, the hepatocyte loses its ability to synthesize albumin and the serum albumin level is markedly decreased. Low serum albumin levels may also result from excessive loss of albumin into urine (as in nephrotic syndrome) or into third-space volumes (as in ascites), liver disease, increased capillary permeability, or protein-caloric malnutrition.
Nursing interventions
Assess the venipuncture site for bleeding.
Oral cholecystography
Rationale
The oral cholecystogram (OCG) provides roentgenographic visualization of the gallbladder after the oral ingestion of a radiopaque, iodinated dye. Adequate visualization requires concentration of the dye within the gallbladder. An OCG (also called a gallbladder [or GB] series) is less accurate than a gallbladder ultrasound and is less commonly used for visualizing the biliary tree. OCG will not visualize the biliary tree in the jaundiced patient. Adequate dye concentration depends on the following factors:
Nursing interventions
Before administering the dye, make certain the patient is not allergic to iodine to prevent adverse or allergic reaction. This rarely occurs because the dye is not administered intravenously. If the patient is not allergic to iodine, administer six tablets orally (e.g., iopanoic acid (Telepaque), iodalphionic acid (Priodax), or iprodate (Oragrafin), one every 5 minutes, beginning after the evening meal. The patient is on NPO status from midnight. The patient may be given a high-fat meal or beverage to stimulate emptying of the gallbladder after the test has begun. No other food or fluids are allowed until after the examination.
Intravenous cholangiography
Rationale
In intravenous cholangiography, intravenously administered radiographic dye is concentrated by the liver and secreted into the bile duct. The intravenous cholangiogram (IVC) allows visualization of the hepatic and common bile ducts and also the gallbladder if the cystic duct is patent. IVC is used to demonstrate stones, strictures, or tumors of the hepatic duct, common bile duct, and gallbladder. IVC is a less commonly used method of visualizing the biliary tree and will not do so in a jaundiced patient.
Operative cholangiography
In operative cholangiography the common bile duct is directly injected with radiopaque dye. Stones appear as radiolucent shadows, and tumors cause partial or total obstruction of the flow of dye into the duodenum. Visualization of the biliary duct structures provides the surgeon with a “road map” of a difficult anatomical area. This reduces the possibility of inadvertently injuring the common duct.
If common duct stones are suspected, a cholecystectomy as well as a common duct exploration (CDE) must be performed. When intraoperative cholangiography is used routinely, CDE is performed only on those with positive cholangiograms.
T-tube cholangiography
Rationale
T-tube cholangiography (postoperative cholangiography) is performed to diagnose retained ductal stones postoperatively in the patient who has had a cholecystectomy and a common bile duct (CBD) exploration to demonstrate good flow of contrast into the duodenum. The test is performed through a T-shaped rubber tube that the surgeon places in the bile duct during the operation. The end of the T-tube exits through the abdominal wall, where dye is injected and radiographic films taken.
Nursing interventions
Protect the patient from sepsis by connecting the T-tube (if left in place) to a sterile closed-drainage system. If the T-tube is removed, cover the T-tube tract site with a sterile dressing to prevent bacteria from entering the ductal system.
Before administering the dye, ensure that the patient is not allergic to iodine. Preparation of the patient also includes NPO status after midnight and until the examination is completed. Administer a cleansing enema on the morning of the examination, if ordered.
Ultrasonography of the liver, the gallbladder, and the biliary system
Rationale
Ultrasonography (ultrasound, echogram) is an imaging technique that visualizes deep structures of the body by recording the reflections (echoes) of ultrasonic waves directed into the tissues. This diagnostic test is not effective in examining all tissue because ultrasound waves do not pass through structures that contain air, such as the lungs, the colon, or the stomach. Although fasting is preferred, it is not necessary for ultrasonography. Because ultrasound requires no contrast material and has no associated radiation, it is especially useful for patients who are allergic to contrast media or are pregnant. Ultrasound is used with increasing frequency to corroborate data already obtained by “questionable positive” cholangiograms, liver scans, and OCGs.
Nursing interventions
The patient is on NPO status from midnight. If the patient had recent barium contrast studies, request an order for cathartics. Ultrasound cannot penetrate barium, and the study will not be adequate.
Gallbladder scanning
Rationale
The biliary tract can be evaluated safely, accurately, and noninvasively with the use of intravenous (IV) injection of technetium (99Tc; technetium99m), and positioning the patient under a camera to record distribution of tracer in the liver, the biliary tree, the gallbladder, and the proximal small bowel. The primary use of this study is in the diagnosis of acute cholecystitis. This procedure is superior to oral cholecystography, ultrasonography, and computed tomography (CT) scanning of the abdomen for the detection of acute cholecystitis. Hepatobiliary iminodiacetic acid (HIDA) scanning is also useful for identifying diffuse hepatic disease (such as cirrhosis or neoplasm).
Nursing interventions
Reassure the patient that exposure to radioactivity is minimal because only a trace dose of the radioisotope is used. The patient is on NPO status from midnight until the examination is complete.
Needle liver biopsy
Rationale
Needle liver biopsy is a safe, simple, and valuable method of diagnosing pathologic liver conditions. A specially designed needle is inserted through the skin, between the sixth and seventh or eighth and ninth intercostal spaces, and into the liver. The patient lies supine with the right arm over the head. The patient is instructed to exhale fully and not breathe while the needle is inserted. This procedure is often done using ultrasound or CT guidance. A piece of hepatic tissue is removed for microscopic examination. The tissue sample is placed into a labeled specimen bottle containing formalin and sent to the pathology department. Percutaneous liver biopsy is used in the diagnosis of various liver disorders, such as cirrhosis, hepatitis, drug-related reactions, granuloma, and tumor.
Nursing interventions
Explain the procedure to the patient and obtain the patient’s signature on a consent form. Ensure that measurements of platelets, clotting or bleeding time, prothrombin time, and International Normalized Ratio (INR) have been ordered; report any abnormal values to the physician. After the procedure observe the patient for symptoms of bleeding. Monitor vital signs every 15 minutes (two times), then every 30 minutes (four times), and then every hour (four times).
Some pain is common. When leakage involves a large quantity of blood or bile, the peritoneal reaction is great and the resulting pain severe. Assess the patient for pneumothorax (collapsed lung) caused by improper placement of the biopsy needle into the adjacent chest cavity or for bile peritonitis. Immediately report to the physician signs and symptoms of pneumothorax such as shortness of breath, change in respiratory and cardiac rate, or decreased breath sounds on the affected side. Keep the patient lying on the right side for at least 2 hours to splint the puncture site. In this position, the liver capsule is compressed against the chest wall, decreasing the risk of hemorrhage or bile leak.
Radioisotope liver scanning
Rationale
This radionuclide procedure is used to outline and detect structural changes of the liver. A radionuclide is given intravenously. Later, a gamma-ray detecting device (Geiger counter) is passed over the patient’s abdomen. This records the distribution of the radioactive particles in the liver. The spleen can also be visualized by the detector when technetium 99m sulfur is used.
Nursing interventions
The patient is on NPO status from midnight. Assure patients that they will not be exposed to a large amount of radioactivity, since only trace doses of isotopes are used.
Serum ammonia test
Normal value is 10 to 80 mcg/dL.
Rationale
Ammonia is a by-product of protein metabolism. Most of the ammonia is made by bacteria acting on proteins in the intestine. By way of the portal vein, ammonia goes to the liver, where it is normally converted into urea and then excreted by the kidneys. When the patient has severe liver dysfunction or altered blood flow to the liver, ammonia cannot be catabolized, the serum ammonia level rises, and the blood urea nitrogen level decreases. The serum ammonia level is primarily used as an aid in diagnosing hepatic encephalopathy and hepatic coma. Elevated serum ammonia levels suggest liver dysfunction as the cause of these signs and symptoms.
Nursing interventions
On the laboratory requisition, list any antibiotics the patient is currently taking. Certain broad-spectrum antibiotics such as neomycin can cause a decreased ammonia level, thus giving inaccurate test results.
Hepatitis virus studies
A normal laboratory test result will be negative for hepatitis-associated antigen.
Rationale
Hepatitis is an inflammation of the liver caused by viruses, bacteria, and noninfectious causes of liver inflammation. Six viruses, designated A through G, can cause this disease. Hepatitis A and B viruses have been recognized for years, but hepatitis C, D, E, and G viruses were identified more recently (so-called hepatitis F virus was eventually found to be a mutation of hepatitis C virus [HCV]). Hepatitis A, B, and C viruses are the most common viruses that cause hepatitis. Hepatitis D virus is carried by the hepatitis B virus (HBV). Both hepatitis D and E viruses are seen less frequently in the United States than the hepatitis A, B, or C viruses (Pagana & Pagana, 2008). The individual hepatitis viruses can be detected by different antigen and antibody levels, and different incubation periods must be considered.
Nursing interventions
Use standard precautions and handle the serum specimen as if it were capable of transmitting viral hepatitis. Don gloves when handling any blood or body fluids, and wash hands carefully after handling equipment.
Serum amylase test
Normal value is 60 to 120 Somogyi units/dL, or 30 to 220 units/L (SI units).
Rationale
The serum amylase test is an easily and rapidly performed test for pancreatitis. Damage to pancreatic cells (as in pancreatitis) or obstruction to the pancreatic ductal flow (as in pancreatic carcinoma) causes an outpouring of this enzyme into the intrapancreatic lymph system and the free peritoneum. Blood vessels draining the free peritoneum and absorbing the lymph pick up this excess amylase. An abnormal rise in the serum level of amylase occurs within 2 hours of the onset of pancreatic disease. Because amylase is rapidly cleared by the kidney, serum levels may return to normal within 36 hours. Persistent pancreatitis, duct obstruction, or pancreatic duct leak (e.g., pseudocysts) cause persistent elevated serum levels.
Nursing interventions
Note on the laboratory requisition whether the patient is receiving intravenous dextrose or any medications, since these can cause a false-negative result.
Urine amylase test
The normal value for this study is up to 5000 Somogyi units/24 hr, or 6.5 to 48.1 units/hr.
Rationale
Levels of amylase in the urine remain elevated for 7 to 10 days after the onset of disease. Urine amylase is particularly useful in detecting pancreatitis late in the disease course. This fact is important for diagnosing pancreatitis in patients who have had symptoms for 3 days or longer.
Nursing interventions
Record the exact time at the beginning and end of the collection period. A 2-hour spot urine or 6-hour, 12-hour, or 24-hour collection can be performed, depending on the physician’s order. The collection begins after the patient empties the bladder and discards that specimen. All subsequent urine is collected, including the voiding at the end of the collection period. Keep the specimen on ice or refrigerated until it is sent to the laboratory.
Serum lipase test
The normal value is 10 to 140 units/L.
Rationale
Like serum amylase, serum lipase is elevated in acute pancreatitis and is a helpful complementary test because other disorders (e.g., mumps, cerebral trauma, renal transplantation) may also cause an increase in serum amylase. Lipase appears in the bloodstream after damage to the pancreas. The lipase levels rise a little later than amylase levels (4 to 48 hours after the onset of pancreatitis), peak around 24 hours, and remain elevated for at least 14 days. Because lipase peaks later and remains elevated longer than amylase, it is more useful in the diagnosis of acute pancreatitis later in the course of the disease.
Nursing interventions
Instruct the patient to remain on NPO status from midnight, except for water.
Ultrasonography of the pancreas
Rationale
With the use of reflected sound waves, ultrasonography of the pancreas provides diagnostic information of this inaccessible abdominal organ. Ultrasound examination of the pancreas is mainly used to diagnose carcinoma, pseudocyst, pancreatitis, and pancreatic abscess. Because abnormalities seen on ultrasound persist from several days to weeks, it can support the diagnosis of pancreatitis even after the serum amylase and lipase levels have returned to normal. Furthermore, follow-up ultrasound study is used to monitor the resolution of pancreatic inflammation and a tumor’s response to therapy.
Nursing interventions
Fluids and food are withheld for 8 hours before the examination, but fasting is not mandatory to obtain accurate results. If the patient’s abdomen is distended with gas or if the patient has had a recent barium examination, postpone this study, since gas or barium interferes with sound wave transmission.
Computed tomography of the abdomen
Rationale
CT scan of the abdomen is a noninvasive, accurate radiographic procedure used to diagnose pathologic pancreatic conditions such as inflammation, tumors, pseudocyst formation, ascites, aneurysms, cirrhosis, abscesses, trauma, cysts, and anatomical abnormalities. The recognizable cross-sectional image produced by a CT scan is especially important for studying the pancreas, since this organ is well hidden by the overlying peritoneal organs.
Nursing interventions
Fluids and food are withheld from midnight until the examination is complete; however, this test can be performed on an emergency basis on patients who have recently eaten. If possible, show the patient a picture of the machine and encourage the patient to verbalize fears because some patients suffer claustrophobia when enclosed in the machine.
Endoscopic retrograde cholangiopancreatography of the pancreatic duct
Rationale
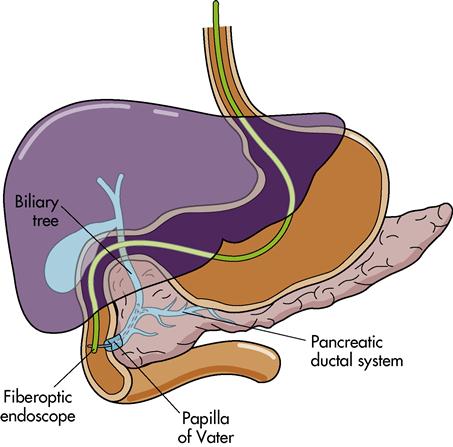
Endoscopic retrograde cholangiopancreatography (ERCP) enables visualization not only of the biliary system but also of the pancreatic duct. The test involves inserting a fiberoptic duodenoscope through the oral pharynx, through the esophagus and the stomach, and into the duodenum (Figure 6-1). Dye is injected for radiographic visualization of the common bile duct and pancreatic duct. ERCP of the pancreas is a sensitive and reliable procedure for detecting clinically significant degrees of pancreatic dysfunction. It can also be used to evaluate obstructive jaundice, remove common bile duct stones, and place biliary and pancreatic duct stents to bypass obstruction. Localized pancreatic duct narrowing indicates tumor. Chronic pancreatitis is demonstrated by multiple areas of ductal narrowing, which can be visualized by ERCP.
Nursing interventions
Withhold food and fluids for 8 hours before the examination, and obtain the patient’s signature on a consent form. Assess prothrombin time and INR before the procedure. Tell patients that the test takes approximately 1 to 2 hours, during which time they must lie completely motionless on a hard x-ray table, which may be uncomfortable. After the procedure, keep the patient on NPO status until the gag reflex returns; assess for abdominal pain, tenderness, and guarding. Assess for signs and symptoms of pancreatitis (the most common ERCP complication), including increasingly intense abdominal pain, nausea, fever, chills, vomiting, and diminished or absent bowel sounds. Assess for hypovolemic shock.
Disorders of the liver, biliary tract, gallbladder, and exocrine pancreas
The liver, the gallbladder, and the exocrine pancreas are all organs that assist with digestion. Review anatomy and physiology of accessory organs of digestion (see Chapter 5) and hepatic portal circulation.
Cirrhosis
Etiology and pathophysiology
Cirrhosis is a chronic, degenerative disease of the liver in which the lobes are covered with fibrous tissue, the parenchyma (tissue of an organ, as opposed to supporting or connective tissue) degenerates, and the lobules are infiltrated with fat. The liver tries unsuccessfully to regenerate and, as a result, forms abnormal blood vessels and biliary duct abnormalities (Lewis et al., 2007). The overgrowth of new and fibrous (scar) tissue restricts the flow of blood to the organ, which contributes to its destruction. Hepatomegaly (enlargement of the liver) and, later, liver contraction cause loss of the organ’s function.
Cirrhosis is ranked as the ninth leading cause of death in the United States and fourth leading cause of death in people between ages 35 and 54. The highest incidence occurs between ages 40 and 60.
There are several forms of cirrhosis, caused by different factors. Alcoholic cirrhosis, previously called Laennec’s cirrhosis, is most commonly found in the Western world. It affects more men than women and occurs in patients with a history of chronic alcohol ingestion. Postnecrotic cirrhosis, found worldwide, is caused by viral hepatitis, exposure to hepatotoxins (e.g., industrial chemicals), or infection. Primary biliary cirrhosis occurs more often in women and results from destruction of the bile ducts. Secondary biliary cirrhosis is caused by chronic biliary tree obstruction from gallstones, a tumor, or biliary atresia in children. Cardiac cirrhosis results from longstanding, severe right-sided heart failure in patients with cor pulmonale, constrictive pericarditis, and tricuspid insufficiency.
The cause of cirrhosis is not always known. Alcoholism is by far the greatest factor leading to cirrhosis. It is believed to result from the combination of alcohol’s hepatotoxic effect on the liver coupled with the common problem of protein malnutrition seen in alcoholics. Cirrhosis of the liver from severe malnutrition without alcoholism has also occurred. Patients with a diagnosis of chronic hepatitis B and C have a 10% to 20% chance of developing cirrhosis of the liver (Lewis et al., 2007).
With repeated insults, the liver progresses through the following stages: destruction, inflammation, fibrotic regeneration, and hepatic insufficiency. Although liver cells have a great potential for regeneration, repeated scarring decreases their ability to be replaced. As the blood supply continues to diminish and scar tissue increases, the organ atrophies.
Functions of the liver are altered in several ways. The liver’s ability to synthesize albumin is reduced as a result of liver cell damage. Obstruction of the portal vein as it enters the liver results in portal hypertension—increased venous pressure in the portal circulation caused by compression or by occlusion in the portal or hepatic vascular system. In most instances, portal hypertension that is caused by cirrhosis is irreversible.
This increased pressure causes ascites (an accumulation of fluid and albumin in the peritoneal cavity). The damaged liver cannot metabolize protein in the usual manner; therefore protein intake may result in an elevation of blood ammonia levels. Reduced synthesis of protein and the leaking of existing protein result in hypoalbuminemia (reduced protein or albumin level in the blood), which reduces the blood’s ability to regain fluids through osmosis. Protein must be present in adequate amounts to create colloidal osmotic pressure and “attract” the fluid to pass back into the blood vessels after it escapes in the capillaries. As fluid leaves the blood and the circulating volume decreases, the receptors in the brain signal the adrenal cortex to increase secretion of aldosterone to stimulate the kidneys to retain sodium and water. The normal liver inactivates the hormone aldosterone, but the damaged liver allows its effect to continue (hyperaldosteronism). Retention of fluid and sodium results in increased pressure in blood vessels and lymphatic channels, resulting in portal hypertension. Ascites is thus a result of portal hypertension, hypoalbuminemia, and hyperaldosteronism.
Hepatic insufficiency gradually causes distention in veins in the upper part of the body, including the esophageal vein. Esophageal varicosities develop and may rupture, causing severe hemorrhage.
Clinical manifestations
Clinical manifestations of cirrhosis of the liver differ, depending on the stage of the disease. In the early stages the liver is firm and therefore easier to palpate, and abdominal pain may be present because rapid enlargement produces tension on the organ’s fibrous covering. Later stages of the disease are characterized by dyspepsia, changes in bowel habits, gradual weight loss, ascites, enlarged spleen, malaise, nausea, jaundice, ecchymosis, and spider telangiectases (small, dilated blood vessels with a bright red center point and spiderlike branches). Spider telangiectases occur on the nose, cheeks, upper trunk, neck, and shoulders. These later manifestations are the result of scarring of liver tissue that produces chronic failure of liver function and also fibrotic changes that cause obstruction of the portal circulation.
When enough cells of the liver become involved to interfere with its function and obstruct its circulation, the GI organs and the spleen become congested and cannot function properly. Anemia occurs because of the body’s decreased ability to produce red blood cells (RBCs). The cirrhotic liver cannot absorb vitamin K or produce the clotting factors VII, IX, and X. Thus the patient with cirrhosis develops bleeding tendencies.
Assessment
Subjective data in the early stages includes the patient’s description of flulike symptoms, including loss of appetite, nausea and vomiting, general weakness, fatigue, indigestion, abnormal bowel function (either constipation or diarrhea), flatulence, and abdominal discomfort. The anatomical area most commonly affected is in the epigastric region or the right upper quadrant of the abdomen.
Collection of subjective data in the later stages includes noting those subjective symptoms listed under early stages, although they are more intense in later stages. The patient may complain of dyspnea, pruritus, and severe fatigue that interfere with the ability to carry out routine activities. Pruritus is a result of an accumulation of bile salts under the skin from the jaundice.
Collection of objective data in the early stages includes observing low hemoglobin, fever, jaundice (yellow discoloration of the skin, mucous membranes, and sclerae of the eyes [scleral icterus], caused by greater than normal amounts of bilirubin in the serum), and weight loss.
Collection of objective data in the later stages includes noting epistaxis, purpura, hematuria, spider angiomas (telangiectasis), and bleeding gums. Late symptoms are ascites, hematologic disorders, splenic enlargement, and hemorrhage from esophageal varices or other distended GI veins. The patient may also appear mentally disoriented and display abnormal behaviors and speech patterns. Any prolonged interference with gas exchange leads to hypoxia, coma, and ultimately death.
Diagnostic tests
Many diagnostic tests aid in the diagnosis of cirrhosis. Poor liver functioning may be manifested in abnormal electrolyte values; elevated serum bilirubin, AST, ALT, LDH, and gamma GT; decreased total protein and serum albumin; elevated ammonia; low blood glucose (hypoglycemia) from impaired gluconeogenesis; prolonged prothrombin time; increased INR; and decreased cholesterol levels. Visualization through ERCP (to detect common bile duct obstruction), esophagoscopy with barium esophagography to visualize esophageal varices, scans and biopsy of the liver, and ultrasonography are used to diagnose cirrhosis. Paracentesis (a procedure in which fluid is withdrawn from the abdominal cavity) relieves ascites and also provides fluid for laboratory examination.
Medical management
When possible causes have been identified, the initial treatment is to eliminate these causes, decrease the buildup of fluids in the body, prevent further damage to the liver, and provide individual supportive care. Eliminating alcohol, hepatotoxins (e.g., acetaminophen [Tylenol]), or environmental exposure to harmful chemicals is essential to prevent further damage to the liver. Diet therapy is aimed at correcting malnutrition, promoting the regeneration of functional liver tissue, and compensating for the liver’s inability to store vitamins, while avoiding fluid retention and hepatic encephalopathy. A diet that is well balanced, high in calories (2500 to 3000 calories/day), moderately high in protein (75 g of high-quality protein per day), low in fat, low in sodium (1000 to 2000 mg/day), and with additional vitamins and folic acid will usually meet the needs of the patient with cirrhosis and improve deficiencies. A protein-restricted diet may be prescribed for a patient recovering from an acute episode of hepatic encephalopathy.
Antiemetics may be prescribed to control nausea or vomiting. Monitor the patient closely for toxicity, which develops quickly when the poorly functioning liver cannot clear these drugs from the system. Diphenhydramine (Benadryl) or dimenhydrinate (Dramamine) may be given, whereas prochlorperazine maleate (Compazine), hydroxyzine pamoate (Vistaril), or hydroxyzine hydrochloride (Atarax) are contraindicated in severe liver dysfunction.
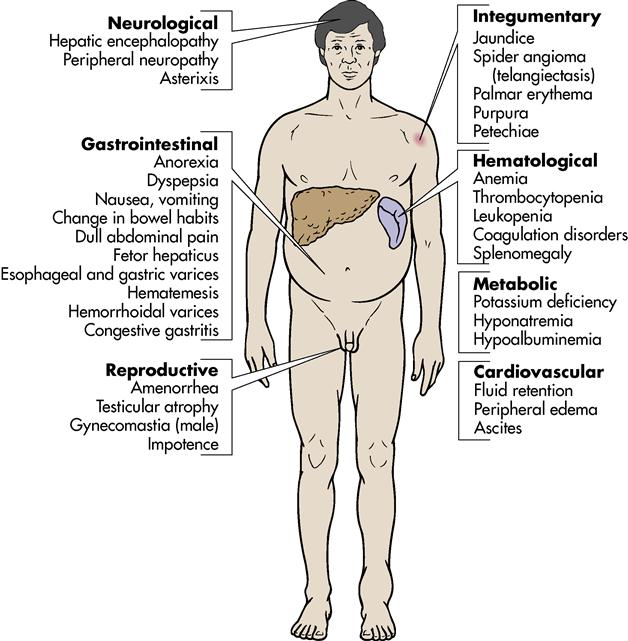
Later manifestations may be severe and result from liver failure and portal hypertension. Jaundice, peripheral edema, esophageal varices, hepatic encephalopathy, and ascites develop gradually (Figure 6-2).
Complications and treatment
Ascites is the presence of excessive fluid in the peritoneal cavity. The severity of fluid retention determines the treatment. Initially the patient is placed on bed rest with accurate monitoring of intake and output (I&O). Restrictions are placed on the amount of fluid (500 to 1000 mL) and sodium (1000 to 2000 mg). Diuretic therapy may be added if the diet does not control the ascites and edema. Spironolactone (Aldactone) 300 to 1,000 mg/day may be used to obtain the desired diuresis. Other diuretics may be added, including furosemide (Lasix) or hydrochlorothiazide (HydroDIURIL). Vitamin supplements include vitamin K, vitamin C, and folic acid. Salt-poor albumin may be administered in an attempt to restore plasma volume if the intravascular volume is decreased significantly. Complications of diuretic therapy include plasma volume deficit, decreased renal function, and electrolyte imbalance.
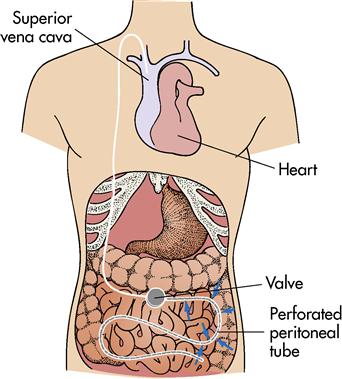
Another method of treatment for ascites and edema is the LeVeen continuous peritoneal jugular shunt (Figure 6-3). This procedure allows the continuous shunting of ascitic fluid from the abdominal cavity through a one-way, pressure-sensitive valve into a silicone tube that empties into the superior vena cava. Monitor the patient carefully for complications, which include congestive heart failure, leakage of ascitic fluid, infection at the insertion sites, peritonitis, septicemia, and shunt thrombosis.
Paracentesis is a temporary method of removing fluid by withdrawing it from the abdominal cavity by either gravity or vacuum. Have the patient void immediately before the procedure to prevent puncture of the bladder. The patient should sit on the side of the bed or be placed in high Fowler’s position. An incision is made in the skin, and a hollow trocar, cannula, or catheter is passed through the incision and into the cavity. The fluid is removed over a period of 30 to 90 minutes to prevent sudden changes in blood pressure, which could lead to syncope. Monitor the patient closely for signs of hypovolemia and electrolyte imbalances. Apply a dressing over the insertion site, and observe for bleeding and drainage.
Esophageal varices (a complex of longitudinal, tortuous veins at the lower end of the esophagus) enlarge and become edematous as the result of portal hypertension. They are susceptible to ulceration and hemorrhage; avoiding this is a main goal of treatment. For patients who have not bled from esophageal varices, prophylactic treatment with nonselective beta blockers (e.g., propranolol [Inderal]) has been shown to reduce the risk of bleeding and bleeding-related deaths. Varices can rupture as a result of anything that increases abdominal venous pressure, such as coughing, sneezing, vomiting, or the Valsalva maneuver. Rupture may occur slowly over several days or suddenly and without pain. An endoscopy may be performed to identify the varices or to rule out bleeding from other sources. Endoscopic therapies include sclerotherapy and ligation of varices.
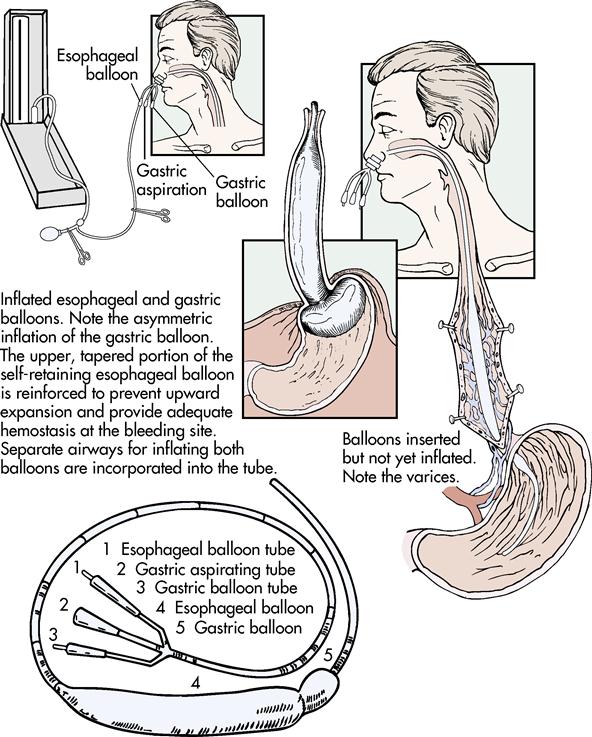
Therapeutic management of a ruptured esophageal varix is a medical emergency. The patient’s airway must be maintained, the bleeding varix controlled, and IV lines established for fluids and blood replacement as needed. The hormone vasopressin (VP), administered intravenously or directly into the superior vena cava, is used to decrease or stop the hemorrhaging. VP produces vasoconstriction of the vessels, decreases portal blood flow, and decreases portal hypertension. Current drug therapy in some institutions is a combination of VP and nitroglycerin (NTG). The NTG reduces the detrimental effects of VP, which are decreased coronary blood flow and increased blood pressure. VP should be avoided or used cautiously in the older adult because of the risk of cardiac ischemia. If the VP drip does not stop or control bleeding, a Sengstaken-Blakemore tube with openings at the tip may be inserted. This triple-lumen tube has a lumen for inflating the esophageal balloon, one for inflating the gastric balloon, and one for gastric lavage (Figure 6-4). The tube is passed through the nose, and the balloon in the stomach, the one in the esophagus, or both are inflated to press against the bleeding vessels and control the hemorrhage. The gastric aspiration is attached to low, intermittent suction. When either balloon is inflated, a Levin tube is passed into the esophagus through the mouth and attached to low suction to drain the saliva that cannot drain into the stomach. The balloon must be deflated periodically to prevent necrosis. Give the patient nothing by mouth and elevate the head of the bed 30 to 45 degrees to help prevent aspiration of stomach contents and help the patient breathe.
Gastric lavage is performed to remove any swallowed blood from the stomach. Some facilities use iced isotonic saline solutions for the lavage to facilitate vasoconstriction. Endoscopic sclerotherapy may also be used to control the bleeding.
Patients suffering from portal hypertension and esophageal varices may benefit from surgical shunting procedures that divert blood from the portal system to the venous system. The portacaval shunt diverts blood from the portal vein to the inferior vena cava. The splenorenal shunt requires the removal of the spleen, and the splenic vein is anastomosed to the left renal vein. The mesocaval shunt involves anastomosis of the superior mesenteric vein to the inferior vena cava. These procedures are associated with a high mortality rate. They may be performed in an emergency to control acute esophageal varix bleeding or in a therapeutic situation when a patient has already bled. Complications of surgical shunting procedures are hepatic encephalopathy, GI bleeding, ascites, and liver failure.
Care of the patient who has hemorrhaged from an esophageal varix includes maintenance of oxygen content levels within the blood and administration of fresh frozen plasma and packed RBCs, vitamin K (AquaMEPHYTON), histamine (H2) receptor blockers such as cimetidine (Tagamet), and electrolyte replacements as needed without fluid overload. Avoid ammonia buildup with the use of cathartics (e.g., lactulose [Chronulac]) and neomycin. Preventing ammonia buildup keeps hepatic encephalopathy from breaking down blood and releasing ammonia in the intestine.
Hepatic encephalopathy is a type of brain damage caused by liver disease and consequent ammonia intoxication. It is thought to result from a damaged liver being unable to metabolize substances that can be toxic to the brain, such as ammonia. The patient’s signs and symptoms progress from inappropriate behavior, disorientation, flapping tremors, and twitching of the extremities to stupor and coma. Treatment of the patient with hepatic encephalopathy consists of supportive care to prevent further damage to the liver.
In the past, a low-protein diet was often prescribed for patients with cirrhosis of the liver. Restricting protein intake was thought to decrease the amount of ammonia produced in the intestine, thus preventing hepatic encephalopathy. It is now believed that protein should not be restricted because these patients often have existing malnutrition. Occasionally, protein is decreased in the diet of a patient with an exacerbation of hepatic encephalopathy (Lewis et al., 2007).
Patients with cirrhosis of the liver require adequate carbohydrates. To provide extra calories, a protein-free supplement such as glucose polymer (Polycose) can be used. Other supplemental enteral formulas such as Hepatic-Aid II may be given to the patient who has protein-calorie malnutrition (Lewis et al., 2007).
Teach the patient to avoid potentially hepatotoxic over-the-counter drugs such as acetaminophen and to abstain from alcohol. Medications may be given to cleanse the bowel and help decrease the serum ammonia. Lactulose decreases the bowel’s pH from 7 to 5, thus decreasing the production of ammonia by bacteria within the bowel. Lactulose may be administered orally, as a retention enema, or via NG tube. It also functions as a cathartic. The lactulose traps the ammonia in the gut, and the drug’s laxative effect expels the ammonia from the colon. Antibiotics such as neomycin, which are poorly absorbed from the GI tract, are given orally or rectally. They reduce the bacterial flora of the colon. Bacterial action on protein in feces results in ammonia production. Because neomycin may cause renal toxicity and hearing impairment, lactulose is frequently preferred.
Asterixis is a hand-flapping tremor in which the patient stretches out an arm and hyperextends the wrist with the fingers separated, relaxed, and extended. A rapid, irregular flexion and extension (flapping) of the wrist occurs in the patient who is acutely ill.
Nursing interventions and patient teaching
Check vital signs every 4 hours, or more often if evidence of hemorrhage is present. Observe the patient for GI hemorrhage as evidenced by hematemesis, melena, anxiety, and restlessness.
Most patients require a well-balanced, moderate, high-protein, high-carbohydrate diet with adequate vitamins. With impending liver failure, protein and fluids are restricted. Sodium restriction is frequently necessary, which can make providing a palatable diet more difficult. Provide frequent oral hygiene and a pleasant environment to help the patient increase food intake.
A major nursing focus for many patients is helping them deal with alcoholism. This requires establishing trust that the health team is interested in the patient’s well-being. Patients must admit that they have a drinking problem. Confrontation is sometimes used to help patients accept the problem. Provide information regarding community support programs, such as Alcoholics Anonymous, for help with alcohol abuse.
Because of pruritus, malnutrition, and edema, the patient with cirrhosis is prone to skin lesions and pressure sores. Initiate preventive nursing interventions to avoid impairment of skin integrity, such as alternating–air pressure mattress, frequent turning, and back rubs. Apply soothing lotion to relieve pruritus.
Observe the patient’s mental status and report changes such as disorientation, headache, or lethargy. Assist in activities of daily living (ADLs) as needed to promote good hygiene while allowing the patient to conserve energy. Observe for edema by measuring ankles daily, and observe for ascites by measuring abdominal girth. Record an accurate I&O and daily weight. Nursing intervention with concern and warmth regardless of physical changes is essential in helping the patient maintain self-esteem.
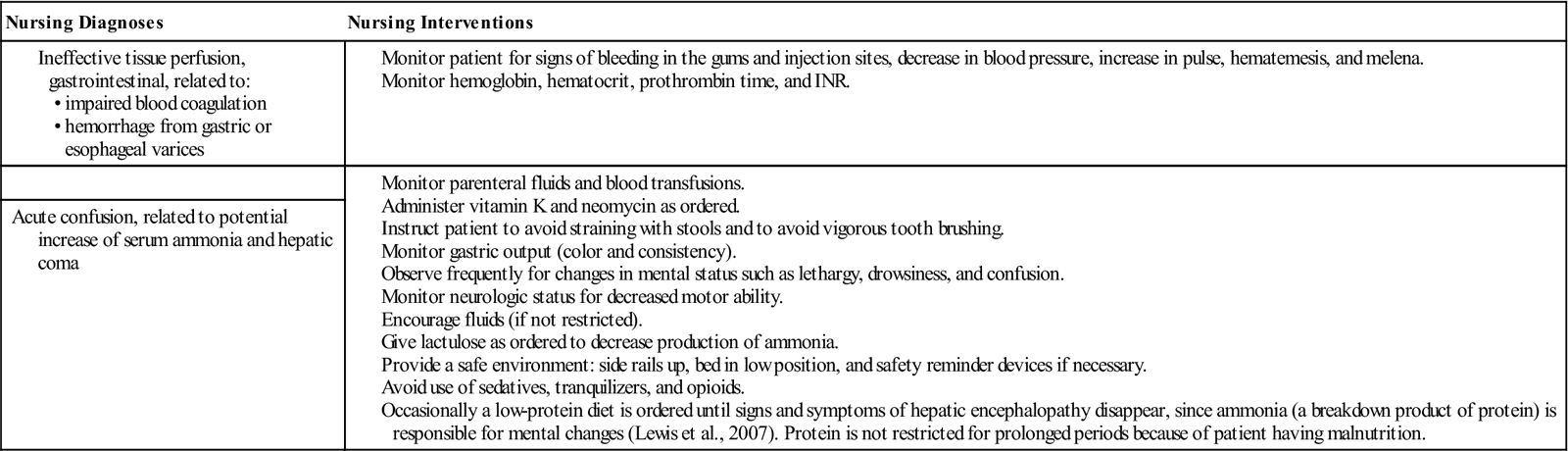
Nursing diagnoses and interventions for the patient with cirrhosis include but are not limited to the following:
The patient with cirrhosis must understand the need for getting adequate rest and avoiding infections. Plan activity around complete bed rest until strength is regained. Turning the patient at least every 2 hours and providing range-of-motion exercises will help avoid infection and prevent thrombophlebitis. Instruct the patient to use a soft-bristled toothbrush, use an electric razor, blow nose cautiously, and avoid straining at stools to prevent bleeding as a result of a lack of vitamin K and certain clotting factors. Avoid soap, perfumed lotion, and rubbing alcohol because they will further dry the skin. For pruritus and dry skin, administer diphenhydramine (Benadryl). Explain the relationship of the therapeutic diet to the diagnosis and the liver’s ability to function.
Help the patient and family identify community resources for home health care and alcohol rehabilitation to help them deal with problems that arise after discharge. Because of the seriousness of the disease, the patient and the family need understanding and support throughout the treatment (see Home Care Considerations box).
 -S
-S -t
-t z,
z,  WN-d
WN-d s,
s,  -KL-zh
-KL-zh n,
n,