Martha E. Spray
Care of the patient with a musculoskeletal disorder
Objectives
1. List the five basic functions of the skeletal system.
2. List the two divisions of the skeleton.
3. Describe the location of major bones of the skeleton.
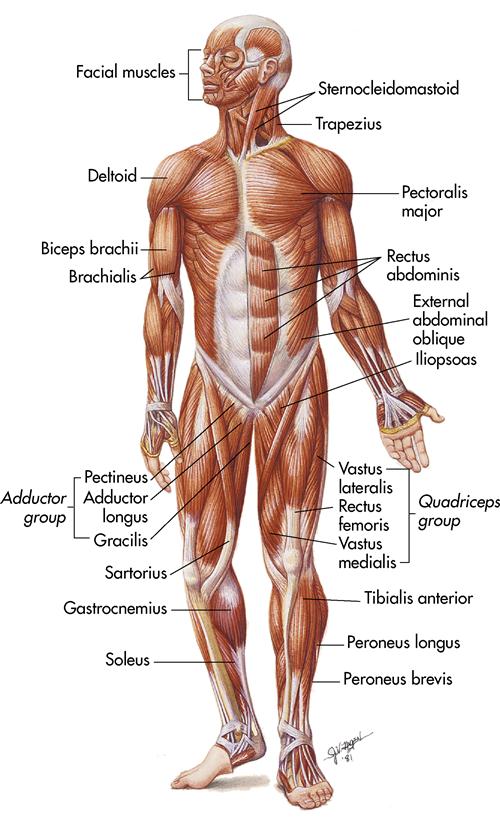
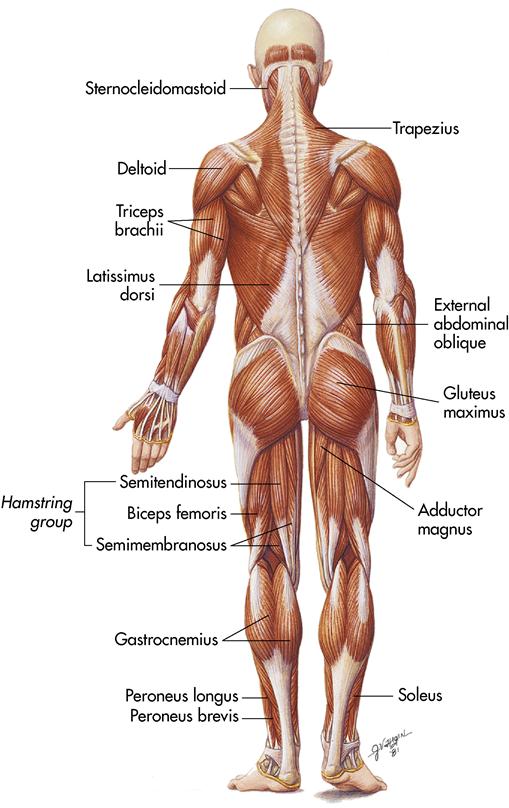
4. Describe the location of the major muscles of the body.
5. List the types of body movements.
6. Describe three vital functions muscles perform when they contract.
7. List diagnostic examinations for musculoskeletal function.
9. Discuss nursing interventions for rheumatoid arthritis.
10. Describe nursing interventions for degenerative joint disease (osteoarthritis).
12. Describe the surgery for arthritis of the hip and knee.
13. Describe nursing interventions for the patient undergoing a total hip or knee replacement.
15. Discuss the physiology of fracture healing (hematoma, granulation tissue, and callus formation).
16. Describe the signs and symptoms of compartment syndrome.
17. List nursing interventions for a fat embolism.
18. List at least two types of skin and skeletal traction.
20. List four nursing interventions for bone cancer.
21. Describe the phenomenon of phantom pain.
Key terms
ankylosis ( ng-k
ng-k -L
-L -s
-s s, p. 124)
s, p. 124)
arthrocentesis ( r-thr
r-thr -s
-s n-T
n-T -s
-s s, p. 116)
s, p. 116)
arthrodesis ( r-thr
r-thr -D
-D -s
-s s, p. 133)
s, p. 133)
arthroplasty ( R-thr
R-thr -pl
-pl s-t
s-t , p. 133)
, p. 133)
bipolar hip replacement (hemiarthroplasty) (h -m
-m –
– R-thr
R-thr -pl
-pl s-t
s-t , p. 139)
, p. 139)
Colles’ fracture (K L-
L- z FR
z FR K-sh
K-sh r, p. 144)
r, p. 144)
fibromyalgia (f -br
-br -m
-m –
– L-j
L-j , p. 131)
, p. 131)
open reduction with internal fixation (ORIF) (p. 145)
paresthesia (p r-
r- s-TH
s-TH -z
-z –
– , pp. 132, 163)
, pp. 132, 163)
scoliosis (sk -l
-l –
– -s
-s s, p. 170)
s, p. 170)
sequestrum (s -KW
-KW S-tr
S-tr m, p. 131)
m, p. 131)
subluxation (s b-l
b-l k-S
k-S -sh
-sh n, p. 162)
n, p. 162)
Volkmann’s contracture (V LK-m
LK-m nz k
nz k n-TR
n-TR K-sh
K-sh r, p. 149)
r, p. 149)
Anatomy and physiology of the musculoskeletal system
Bones and joints form the framework of the body, and muscles contract and relax to allow movement. All movement of the body is orchestrated by the functioning of the bones, the joints, and the muscles attached to the bones. This chapter discusses the structure and the function of bones and muscles and how they serve the body.
Functions of the skeletal system
The human skeletal system is composed of 206 bones. The skeletal system has five basic functions: support, protection, movement, mineral storage, and hematopoiesis.
Support
The skeleton is the the body framework that supports internal tissues and organs.
Protection
The skeleton forms a firm, cagelike structure that protects many internal structures. The cranium (skull) protects the brain, the vertebrae protect the spinal cord, the ribs and the sternum (breastbone) protect the lungs and the heart, and the pelvis protects the digestive and reproductive organs.
Movement
Skeletal muscles are attached to the bones, which enables the bones to provide leverage for movement. As a muscle contracts, it pulls on the bone and movement occurs.
Mineral storage
The bones serve as a storage area for various minerals, particularly calcium and phosphorus. When the body’s intake of these minerals is inadequate, the bones release the minerals.
Hematopoiesis
Hematopoiesis (blood cell formation) takes place in the red bone marrow. The red bone marrow is spongy bone found in the ends of the long bones. A child’s bones contain a proportionately larger amount of red bone marrow than an adult’s. As a person ages, much of the red bone marrow converts to yellow bone marrow, which is composed of fat cells.
Structure of bones
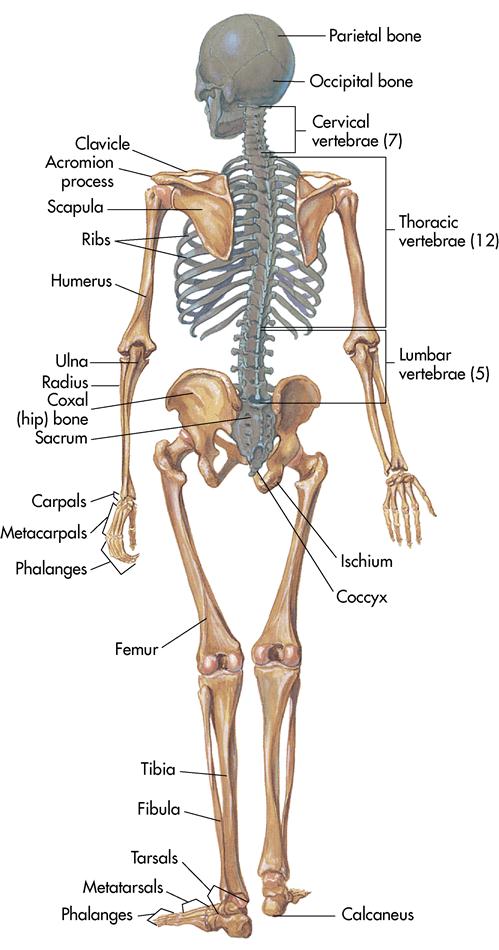
Bones are classified into four groups, based on their form and shape: long, short, flat, and irregular. Long bones are found in the extremities, short bones are found in the hands and feet, flat bones are found in the skull and sternum, and irregular bones make up the vertebrae (backbone).
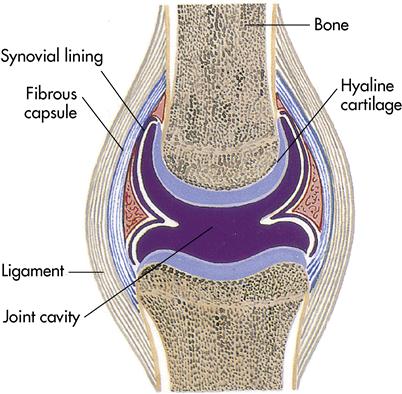
Articulations (joints)
Bones cannot bend without damage. To allow movement, individual bones articulate (join together) at joint sites (Figure 4-1). Bones are held together by flexible connective tissue. The joint is the point of contact between the individual bones. The structure of the individual bones depends on the function of the area. Every bone in the body (except the hyoid bone, which anchors the tongue) connects, or articulates, with at least one other bone.
Joints perform two important functions: they hold the bones together to form the skeleton, and they allow movement and flexibility of the skeleton.
The most common way to classify joints is according to the degree of movement they permit. There are three types of joints:
A goniometer measures the angle of a joint. It is used to determine the degree of joint mobility (Lewis et al., 2007).
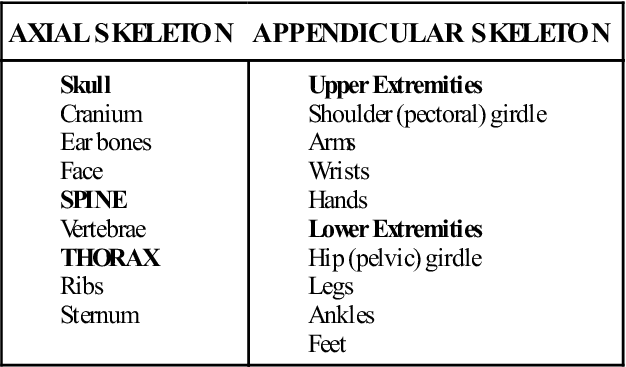
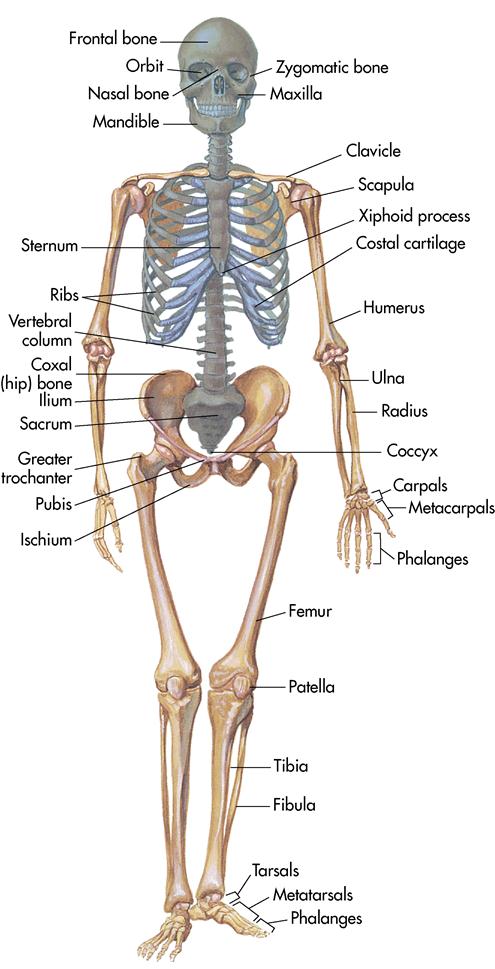
Divisions of the skeleton
The skeleton is divided into the axial and the appendicular skeletons (Box 4-1). The axial skeleton is composed of the skull, hyoid bone in the neck, vertebral column, and thorax (chest). The appendicular skeleton is composed of the upper extremities, lower extremities, shoulder girdle, and pelvic girdle (excluding the sacrum) (Figures 4-2 and 4-3).
Functions of the muscular system
The bones and joints provide the framework of the body, but the muscles are necessary for movement. This motion results from contraction and relaxation of the individual muscles. The body has more than 600 muscles, making up approximately 40% to 50% of the total body weight. They usually act in groups to execute a body movement (Table 4-1).
Table 4-1
| MUSCLE | FUNCTION | INSERTION | ORIGIN |
| MUSCLES OF THE HEAD AND NECK | |||
| Frontal | Raises eyebrow | Skin of eyebrow | Occipital bone |
| Orbicularis oculi | Closes eye | Maxilla and frontal bone | Maxilla and frontal bone (encircles eye) |
| Orbicularis oris | Draws lips together | Encircles lips | Encircles lips |
| Zygomaticus | Elevates corners of mouth and lips | Angle of mouth and upper lip | Zygomatic bone |
| Masseter | Closes jaw | Mandible | Zygomatic arch |
| Temporal | Closes jaw | Mandible | Temporal region of the skull |
| Sternocleidomastoid | Rotates and extends head | Mastoid process | Sternum and clavicle |
| Trapezius | Extends head and neck | Scapula | Skull and upper vertebrae |
| MUSCLES THAT MOVE THE UPPER EXTREMITIES | |||
| Pectoralis major | Flexes and helps adduct upper arms | Humerus | Sternum, clavicle, and upper rib cartilages |
| Latissimus dorsi | Extends and helps adduct upper arm | Humerus | Vertebrae and ilium |
| Deltoid | Abducts upper arm | Humerus | Clavicle and scapula |
| Biceps brachii | Flexes lower arm | Radius | Ulna |
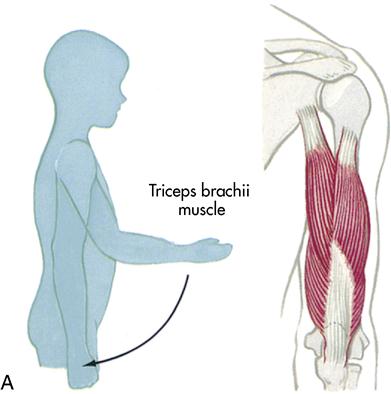
| Triceps brachii | Extends lower arm (called “boxer’s muscle”—straightens the elbow when a blow is delivered) | Ulna | Scapula and humerus |
| MUSCLES OF THE TRUNK | |||
| External oblique | Compresses abdomen | Midline of abdomen | Lower thoracic cage |
| Internal oblique | Compresses abdomen | Midline of abdomen | Pelvis |
| Transversus abdominis | Compresses abdomen | Midline of abdomen | Ribs, vertebrae, and pelvis |
| Rectus abdominis | Flexes trunk | Lower ribcage | Pubis |
| MUSCLES THAT MOVE THE LOWER EXTREMITIES | |||
| Iliopsoas | Flexes thigh or trunk | Ilium and vertebrae | Femur |
| Sartorius | Flexes thigh and rotates lower leg | Tibia | Ilium |
| Gluteus maximus | Extends thigh | Femur | Ilium, sacrum, and coccyx |
| Gluteus medius | Abducts thigh | Femur | Ilium |
| Adductor group | |||
| Adductor longus | Adducts thigh | Femur | Pubis |
| Gracilis | Adducts thigh | Tibia | Pubis |
| Pectineus | Adducts thigh | Femur | Pubis |
| Hamstring group | |||
| Semimembranosus | Flexes lower leg | Tibia | Ischium |
| Semitendinosus | Flexes lower leg | Tibia | Ischium |
| Biceps femoris | Flexes lower leg | Fibula | Ischium and femur |
| Quadriceps group | |||
| Rectus femoris | Extends lower leg | Tibia | Ischium |
| Vastus lateralis, intermedius, and medialis | Extends lower leg | Tibia | Femur |
| Tibialis anterior | Dorsiflexes foot | Metatarsals (foot) | Tibia |
| Gastrocnemius | Plantar flexes foot | Calcaneus (heel) | Femur |
| Soleus | Plantar flexes foot | Calcaneus (heel) | Tibia and fibula |
| Peroneus group | |||
| Peroneus longus and brevis | Plantar flexes foot | Tarsals and metatarsals (ankle and foot) | Tibia and fibula |
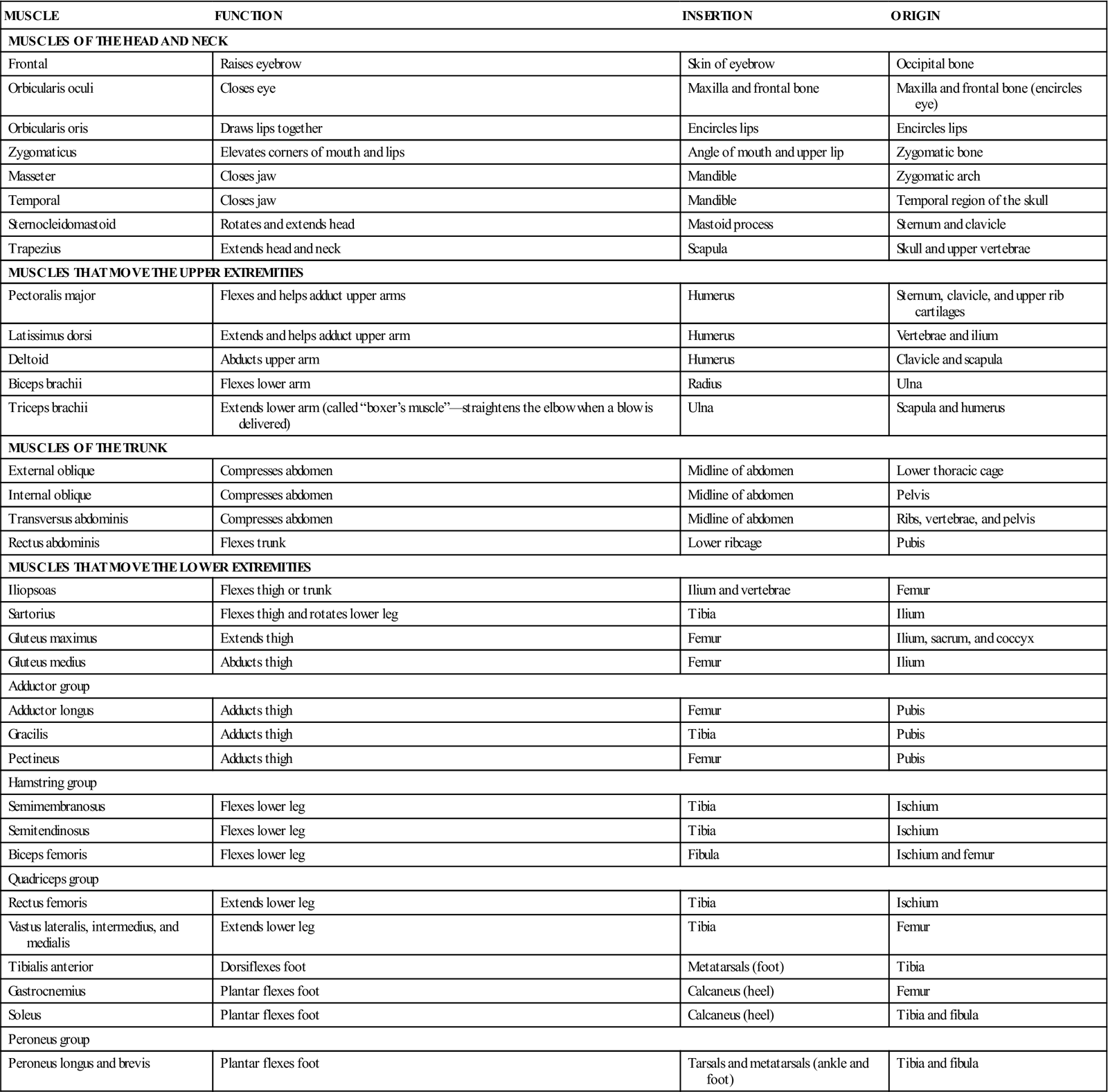
As muscles contract, they perform three vital functions: motion, maintenance of posture, and production of heat. Contraction also assists in return of venous blood and lymph to the right side of the heart.
All body movements rely on the integrated functioning of the bones, joints, and muscles. Muscle tissue is under voluntary or involuntary control. Voluntary muscle is under conscious control, whereas involuntary muscle tissue responds to internal commands without any conscious control of it. Involuntary motions include activities conducted by the internal organs, such as the heart beating, the gallbladder releasing bile, and the stomach churning food.
The contraction of certain skeletal muscles gives the body proper posture. These muscles pull on various bones, allowing the body to sit or stand.
As skeletal muscles contract, they produce body heat. Approximately 85% of all body heat is generated by the contraction of the skeletal muscles.
Skeletal muscle structure
A skeletal muscle is composed of hundreds of muscle fibers (cells). Each skeletal muscle is surrounded by a covering of connective tissue called the epimysium. The epimysium joins with two other inner coverings, the perimysium and the endomysium, and extends beyond the muscle to form a tough cord of connective tissue known as a tendon. Tendons anchor muscles to bones. As a muscle contracts, it pulls the corresponding tendon and bone toward it. This is how movement occurs. Tendons in the ankle and wrist are enclosed in tendon sheaths, which are sleeves or tubelike structures of connective tissue. Tendon sheaths contain synovial fluid and permit the tendons to slide easily; the sheaths also keep the tendons in place. All the tendons, ligaments, and aponeuroses of the body are composed of connective tissue in various sizes, shapes, and densities. These are collectively known as fasciae.
Nerve and blood supply
Because of the physical demands placed on the skeletal muscles, they need a constant supply of oxygen and nutrition. They are well supplied with blood vessels that carry oxygen and nutrition to the area and remove the waste products of metabolism.
The skeletal muscles are voluntary, so they need a constant source of information. Nerve cells or fibers continuously send impulses that stimulate the muscle cells. These impulses enter at the neuromuscular junction, the point of contact between the nerve ending and the muscle fiber. As a nerve impulse passes through this junction, chemicals are released that cause the muscle to contract.
Usually one artery, two veins, and one nerve penetrate a particular muscle. Each muscle cell comes in contact with several capillaries and a portion of a nerve cell. The muscle cells, in union with the nerve cell that controls them, are called a motor unit.
The impulse from the nerve cell must travel across a small gap because the nerve cell and the muscle cell do not directly touch each other. This small gap is called a synaptic cleft and is filled with tissue fluid. A special chemical (neurotransmitter) travels through the fluid to stimulate the muscle fiber. Acetylcholine is the neurotransmitter for skeletal muscle tissue. An enzyme called cholinesterase breaks down the acetylcholine once it has transferred the message. This allows the muscle cell to relax between impulses.
Muscle contraction
Muscle stimulus
Muscle cells are governed by the “all or none” law; that is, when a muscle cell is adequately stimulated or shocked, it will contract completely. Because each skeletal muscle is composed of thousands of muscle cells that react to many different nerve cells, the muscle as a whole contracts according to the principle of graded response. The strength of the muscle contraction, therefore, depends on the number of individual muscle cells responding. These muscle responses allow us to tenderly brush a baby’s cheek or swat an irritating mosquito.
Muscle tone
The skeletal muscles are in a constant state of readiness for action. At any given time, several muscle cells within a certain muscle are contracted; the remainder of the muscle cells are relaxed. Muscle tone is necessary for good posture but does not provide movement. To understand the importance of muscle tone, observe an extremity that has become paralyzed; the muscles are flaccid, limp, or atrophied (wasted) and incapable of producing movement because the cells no longer receive stimuli from the nerve fibers.
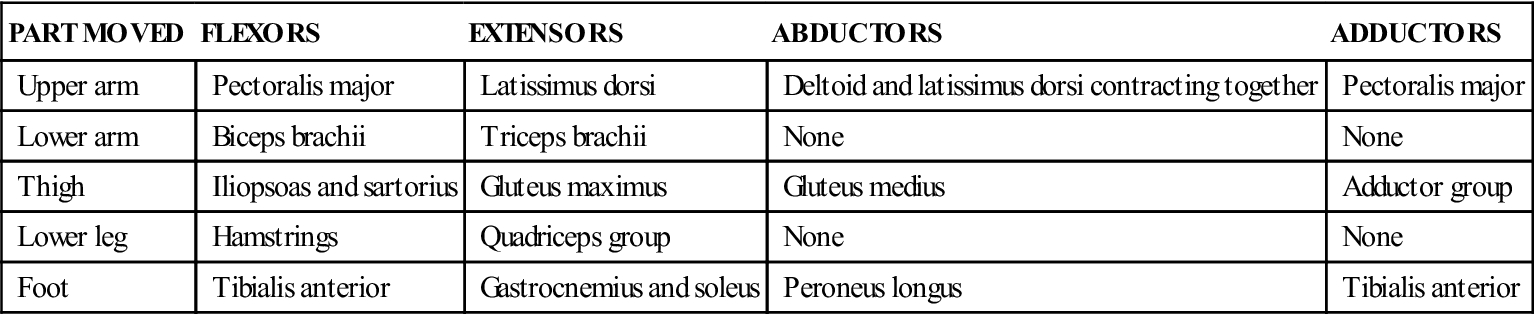
Types of body movements
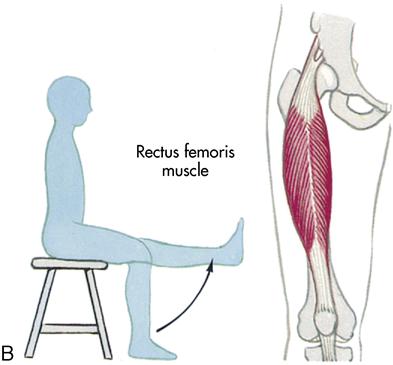
Some muscles can move some body parts in only two directions, whereas others can move certain body parts in several directions. The body’s more common movements include flexion, extension, abduction, adduction, rotation, supination, pronation, dorsiflexion, and plantar flexion (Table 4-2; Box 4-2; Figure 4-4).
Table 4-2
Muscles Grouped According to Function
| PART MOVED | FLEXORS | EXTENSORS | ABDUCTORS | ADDUCTORS |
| Upper arm | Pectoralis major | Latissimus dorsi | Deltoid and latissimus dorsi contracting together | Pectoralis major |
| Lower arm | Biceps brachii | Triceps brachii | None | None |
| Thigh | Iliopsoas and sartorius | Gluteus maximus | Gluteus medius | Adductor group |
| Lower leg | Hamstrings | Quadriceps group | None | None |
| Foot | Tibialis anterior | Gastrocnemius and soleus | Peroneus longus | Tibialis anterior |
Skeletal muscle groups
Skeletal muscles are usually classified into two broad categories: axial and appendicular. The axial muscle groups are located on the head, face, neck, and trunk. The appendicular muscle groups are in the extremities. Figures 4-5 and 4-6 show the location of the muscles of the body.
Laboratory and diagnostic examinations
Radiographic studies
The diagnostic study most often used for determining musculoskeletal system integrity is the radiographic, roentgenographic, or (as it is more commonly known) x-ray examination or diagnostic imaging.
A radiographic examination of a joint reveals fluid, irregularity of the joint with spur formation, or changes in the size of the joint contour. Radiographic examination is used to determine presence of a skeletal fracture. It is important to ask women of childbearing age if there is any possibility that they are pregnant before performing x-ray examinations because pregnant women should not be exposed to radiation except in emergencies because of potential damage to the fetus.
Laminography or planography (also called body section roentgenography) is useful in locating small cavities, foreign bodies, and lesions that are overshadowed by opaque structures.
Scanography, a method of producing a radiograph of internal body organs using a series of parallel beams that eliminate size distortion, allows accurate measurement of bone length.
Myelogram
Myelographic examination involves injection of a radiopaque dye into the subarachnoid space at the lumbar spine to x-ray the spinal cord and the vertebral column to detect herniated disk syndrome (herniated nucleus pulposus) or spinal tumors. The test involves the same procedure as a lumbar puncture (spinal tap), which is discussed in Chapter 14. Contrast medium causes allergic reactions in patients with allergies to iodine and seafood. Notify the physician about such allergies so that a nonionic contrast agent can be used or medications such as steroids or antihistamines can be given before the examination to minimize any reaction to the radiographic dye.
This examination may involve the entire spine or just the cervical or lumbar area. After the myelogram, oil-based dye is removed through the spinal needle to prevent meningeal irritation. Water-soluble dye is used most often and does not need to be removed; the body absorbs it and excretes it in urine. Inform the patient that the test is performed with the patient on a tilting table that is moved during the test to allow contrast medium to flow up to the cervical area.
The most common discomfort after a myelogram is headache. If water-soluble dye is used, the patient should lie quietly in a semi-Fowler’s position for approximately 8 hours. Patient positioning is important to keep the dye in the lower spine. During this time, encouraging fluids helps the body absorb the dye from the spinal column. If oil-based dye is used, the patient rests in a flat position for up to 12 hours. Tell the patient to inform the nurse if he or she has a headache, stiff neck, leg weakness, or difficulty voiding. Rare complications include seizure, infection, drowsiness, severe headache, numbness, and paralysis.
Patients needing a myelogram fear the needle will be inserted into the spinal canal and damage the cord. Inform the patient that the tap is done in the lumbar region of the spine at approximately the fourth or fifth lumbar space (L4-L5). The spinal cord starts at the level of the foramen magnum and ends at the second lumbar space (L2) (lower border of ribcage).
Nuclear scanning
Nuclear scanning tests are done in the nuclear medicine department, which has scanners or camera detectors that record images on radiographic film. Diagnostic tests use low dosages of radioactive isotopes; precautionary measures that are required for radium therapy are not necessary.
Nursing interventions required when patients are scheduled for nuclear scanning procedures involve (1) obtaining written consent from the patient, (2) informing the patient that the radioactive isotopes will not affect family or visitors, and (3) following the nuclear medicine department’s instructions for special preparations for specific scans.
Magnetic resonance imaging
Musculoskeletal magnetic resonance imaging (MRI) assists in diagnosing abnormalities of bones and joints and surrounding soft tissue structures, including cartilage, synovium, ligaments, and tendons. The test uses magnetism and radio waves to make images of cross-sections of the body. MRI can give much more detailed pictures of fluid-filled soft tissue and blood vessels than any other test.
In preparation, have the patient remove any metal, such as jewelry, clothing with metal fasteners, glasses, and hair clips. Patients with metal prostheses such as heart valves, orthopedic screws, or cardiac pacemakers cannot undergo MRI.
The standard machine looks like a narrow tunnel which completely encloses the patient. Patients are required to lie still in this machine for 45 to 60 minutes. The patient enters the tunnel head first and may feel some anxiety or claustrophobia. The procedure is painless; however, if the patient is extremely anxious, a sedative is given. Encourage patients to use relaxation techniques, such as imagery, during the test. New MRI machines called open MRI are designed to be less confining and more comfortable than the traditional machine. Because the procedure requires the patient to be motionless, relaxation techniques that require flexing and relaxing the muscles are not appropriate.
After the test, take routine vital sign measurements and allow the patient to resume pretest activities. There are no adverse effects.
Computed tomography
Body sections can be examined from many different angles using a computed tomography (CT) scanner, which uses a narrow x-ray beam and produces a three-dimensional picture of the structure being studied. The CT scanner is approximately 100 times more sensitive than the radiograph machine and should not be used unnecessarily because of radiation exposure. Iodine contrast dye is sometimes used. CT scan is used for the head and body. It is useful in locating injuries to the ligaments or tendons, tumors of the soft tissue, and fractures in areas difficult to define by other means.
Patient preparation includes (1) having the patient sign a consent form authorizing the examination if not included on the initial hospital consent form, (2) questioning the patient regarding allergies (e.g., iodine and seafood), (3) keeping the patient on NPO (nothing by mouth) status 3 to 4 hours before the test (in case contrast dye is used, since the dye can cause nausea and vomiting), (4) measuring vital signs to be used as a baseline, (5) having the patient void before the test, (6) removing metal articles such as jewelry and hairpins, and (7) telling the patient that he or she must lie still during the test and may feel warm and slightly nauseated for a few minutes when dye is injected.
After the test, observe the patient for delayed allergic reactions (if contrast dye was used). Encourage fluids unless contraindicated. Pretest diet and activity can usually be resumed.
Bone scan
The bone scan test is especially valuable in detecting metastatic and inflammatory bone disease (osteomyelitis). This test involves the intravenous (IV) administration of nuclides (atomic material) approximately 2 to 3 hours before the test is scheduled. There are no food or fluid restrictions, and patients are encouraged to drink water over the next 1 to 3 hours to aid renal clearance of any radioisotope not picked up by the bone. After the patient has voided, a scanning camera reveals the degree of radionuclide uptake; areas of concentrated nucleotide uptake may represent a tumor or other abnormality. These areas of concentration can be detected days or weeks before an ordinary radiograph reveals a metastatic lesion. The test takes approximately 30 to 60 minutes and requires the patient to lie still.
Aspiration
An aspiration procedure is done to obtain a specimen of body fluid. The physician inserts a needle into a cavity with the patient under local anesthesia. This procedure is performed using sterile technique. Commonly the physician takes a biopsy of tissue while doing the aspiration procedure. Nursing interventions are similar for all aspiration tests, with special emphasis on (1) having the consent form signed; (2) reinforcing the physician’s explanation of the procedure; (3) encouraging the patient to remain immobile during the procedure; (4) having the patient void before the procedure; (5) maintaining sterile technique; (6) supporting the patient emotionally; (7) applying a sterile pressure dressing to the puncture site and maintaining the dressing until bleeding has stopped; (8) assisting with collecting, labeling, and transporting a specimen to the laboratory immediately; and (9) observing for emotional and physical distress after the procedure.
Synovial fluid aspiration
Arthrocentesis is the puncture of a patient’s joint with a needle and the withdrawal of synovial fluid for diagnostic purposes. It is helpful in diagnosing trauma, systemic lupus erythematosus, gout, osteoarthritis, and rheumatoid arthritis (RA). It may also be used to instill medications for the patient with septic arthritis or to remove fluid from joints to relieve pain. Normally a patient’s synovial fluid is straw colored, clear, or slightly cloudy. If trauma or a disease is present, the synovial fluid appears cloudy, milky, sanguineous, yellow, green, or gray.
After the procedure, provide proper support to the affected extremity. Placing it on a pillow and maintaining joint rest for approximately 12 hours may be indicated. Apply ice to the affected joint for 24 to 48 hours unless otherwise ordered. An antiinfective or corticosteroid may be prescribed. Assess the patient for signs of infection. After the pressure dressing is removed from the site, an adhesive bandage can be used.
Endoscopic examination
For endoscopy, a lighted tube is used to visualize inside a body cavity. Although some procedures require general anesthesia, most require only local anesthesia. Emotional support and complete explanations help relieve the patient’s anxiety. Preparation for an endoscopic examination is similar to that for surgical preparation: (1) have the patient sign a consent form; (2) complete a preoperative checklist with special attention to removing jewelry, dentures, and contact lenses; (3) initiate NPO status 6 to 12 hours before the examination; (4) give premedications, such as atropine and a sedative; (5) encourage the patient to void; (6) record vital signs; and (7) maintain bed rest with side rails up after giving the premedication.
Arthroscopy
Arthroscopy is an endoscopic examination that enables direct visualization of a joint. The procedure is used to (1) explore the joint to determine the presence of a disease process, (2) drain fluid from the joint cavity, and (3) remove damaged tissue or foreign bodies.
This examination is most commonly done on the knee joint, with the synovium, articular surfaces, and meniscus (a curved, fibrous cartilage in the knee) visualized through the scope. The procedure involves insertion of a large-bore needle into the suprapatellar pouch and saline instillation into the joint. Arthroscopy can also be done on the hip or shoulder. The patient may be given a general or local anesthetic agent. After the arthroscopic examination, advise the patient to limit activities for several days.
Endoscopic spinal microsurgery
Surgeons can perform spinal surgery with less damage to surrounding tissues by passing endoscopic equipment through small incisions. Special scopes enable surgeons to successfully treat spinal column disorders (e.g., herniated disk, spinal stenosis) and spinal deformities (e.g., scoliosis, kyphosis). Spinal microsurgery can be performed with the patient under local anesthesia; discharge occurs after a brief stay. Candidates for microsurgery procedures are evaluated on information obtained from x-ray examinations, MRI scans, CT scans, and bone scans.
Electrographic procedure
Electrographic procedures use electrodes to measure electrical activity in specific areas of the body.
Electromyogram
An electromyogram involves insertion of needle electrodes into the skeletal muscles so that electrical activity can be heard, seen on an oscilloscope (an instrument that displays a graphic representation of electron beams), and recorded on paper at the same time. Muscles do not produce an electrical charge at rest, but with neuromuscular disorders unusual patterns can be observed. Nerves can be observed for neuropathy and muscles for myopathy. Electromyography can be used to detect chronic low back pain based on muscle fatigue patterns.
Laboratory tests
Specific laboratory tests are ordered when musculoskeletal disorders are suspected (Table 4-3).
Table 4-3
Laboratory Tests for Musculoskeletal Disorders
 P-
P- -t
-t s,
s,  -F
-F -s
-s s,
s,  r-D
r-D -s
-s s,
s,  -f
-f ,
,