Barbara Lauritsen Christensen
Care of the patient with an endocrine disorder
Objectives
1. List and describe the endocrine glands and their hormones.
2. Define the negative feedback system.
3. Explain the action of the hormones on their target organs.
4. Describe how the hypothalamus controls the anterior and posterior pituitary glands.
6. List four tests used in the diagnosis of hyperthyroidism.
7. Explain how to test for Chvostek’s sign, Trousseau’s sign, and carpopedal spasms.
8. List two significant complications that may occur after thyroidectomy.
9. Discuss the medications commonly used to treat hyperthyroidism and hypothyroidism.
10. Differentiate between the clinical manifestations of Cushing’s syndrome and Addison’s disease.
12. Differentiate between the signs and symptoms of hyperglycemia and hypoglycemia.
14. Explain the roles of nutrition, exercise, and medication in the control of diabetes mellitus.
17. Discuss the various insulin types and their characteristics.
18. Describe the correct way to draw up and administer insulin.
19. Discuss the various classes of oral hypoglycemic medications to treat type 2 diabetes mellitus.
20. Discuss the acute and long-term complications of diabetes mellitus.
Key terms
Chvostek’s sign (KHV S-t
S-t ks s
ks s n, p. 498)
n, p. 498)
endocrinologist ( n-d
n-d -kr
-kr -N
-N L-
L- -j
-j st, p. 491)
st, p. 491)
glycosuria (gl -k
-k s-
s- -r
-r –
– , p. 511)
, p. 511)
hirsutism (H R-s
R-s
 t-
t- szm, p. 505)
szm, p. 505)
hyperglycemia (h -p
-p r-gl
r-gl -S
-S -m
-m –
– , p. 511)
, p. 511)
hypocalcemia (h -p
-p -k
-k l-S
l-S -m
-m –
– , p. 503)
, p. 503)
hypoglycemia (h -p
-p -gl
-gl -S
-S -m
-m –
– , p. 518)
, p. 518)
hypokalemia (h -p
-p -k
-k -L
-L -m
-m –
– , p. 504)
, p. 504)
idiopathic hyperplasia ( d-
d- –
– -P
-P TH-
TH- k h
k h -p
-p r-PL
r-PL -zh
-zh , p. 489)
, p. 489)
ketoacidosis (k -t
-t –
– -s
-s -D
-D -s
-s s, p. 511)
s, p. 511)
ketone bodies (K -t
-t n b
n b d-
d- z, p. 510)
z, p. 510)
lipodystrophy (l p-
p- -D
-D S-tr
S-tr -f
-f , p. 517)
, p. 517)
neuropathy (n-R P-
P- -th
-th , p. 522)
, p. 522)
polydipsia (p l-
l- -D
-D P-s
P-s –
– , p. 511)
, p. 511)
Trousseau’s sign (tr-S Z s
Z s n, p. 498)
n, p. 498)
type 1 diabetes mellitus (t p 1 d
p 1 d –
– -B
-B -t
-t z M
z M L-
L- -t
-t s, p. 509)
s, p. 509)
type 2 diabetes mellitus (t p 2 d
p 2 d –
– -B
-B -t
-t z M
z M L-
L- -t
-t s, p. 510)
s, p. 510)
Anatomy and physiology of the endocrine system
Endocrine glands and hormones
Glands can be divided into two broad categories: exocrine and endocrine. Exocrine glands secrete through a series of ducts (sebaceous and sudoriferous glands of the skin). Their secretions are protective and functional. Endocrine glands are ductless; they release their secretions directly into the bloodstream. Their secretions have a regulatory function.
The endocrine system is composed of a series of ductless glands whose work is closely related to the nervous system. Both systems control homeostasis through communication within the systems. The endocrine system communicates more slowly through the use of hormones, which are chemical messengers that travel through the bloodstream to their target organ. When the hormone reaches its target, a metabolic change occurs.
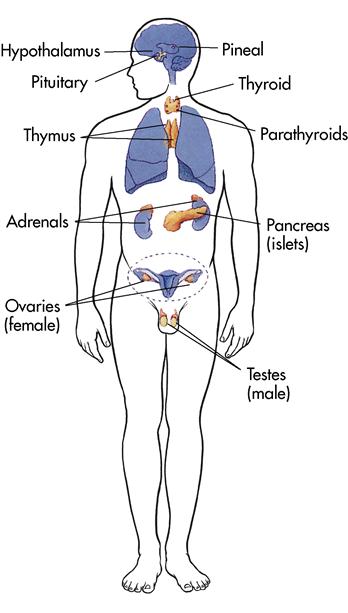
The total weight of all the endocrine glands is less than half a pound, yet they have a powerful influence. The slightest change in hormonal levels can upset the metabolic balance of the entire body. Hormones can increase or decrease a normal body process by affecting a target organ. Too much or too little of a given hormone can affect other hormones, and for this reason they are somewhat interrelated. The endocrine glands (Figure 11-1) have a generalized effect on the patient’s metabolism, growth, development, reproduction, and many other bodily activities.
The amount of hormonal release is controlled by a negative feedback (a decrease in function in response to stimuli) system. Information is constantly being exchanged between the target organ and the pituitary gland via the bloodstream regarding the effect of the hormone on the target organ.
Pituitary gland
The pea-sized pituitary gland (hypophysis) is one of the most powerful glands in the body. It has been called the “master gland” because, through the negative feedback system, it controls the other endocrine glands. It works closely with the hypothalamus of the brain and is located in the cranial cavity in a small saddlelike depression in the sphenoid bone. It is divided into two segments, the anterior pituitary (adenohypophysis) and the posterior pituitary (neurohypophysis). Each segment has specialized hormones. The hypothalamus actually produces the hormones of the posterior pituitary and releases them for storage in the posterior pituitary gland; they are released from here as a result of nerve impulses received from the hypothalamus.
Anterior pituitary gland
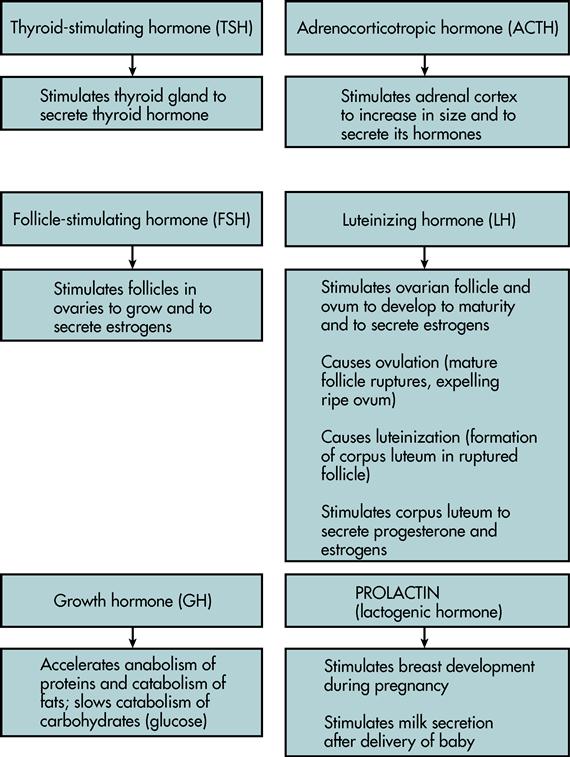
Six major hormones are secreted by the anterior pituitary gland; the hormones make up about 75% of the gland’s total weight. Five hormones are called tropic hormones, because they are responsible for the stimulation of other endocrine glands. Prolactin, the remaining hormone, causes the mammary glands to produce milk. These hormones and their functions are shown in Figures 11-2 and 11-3.
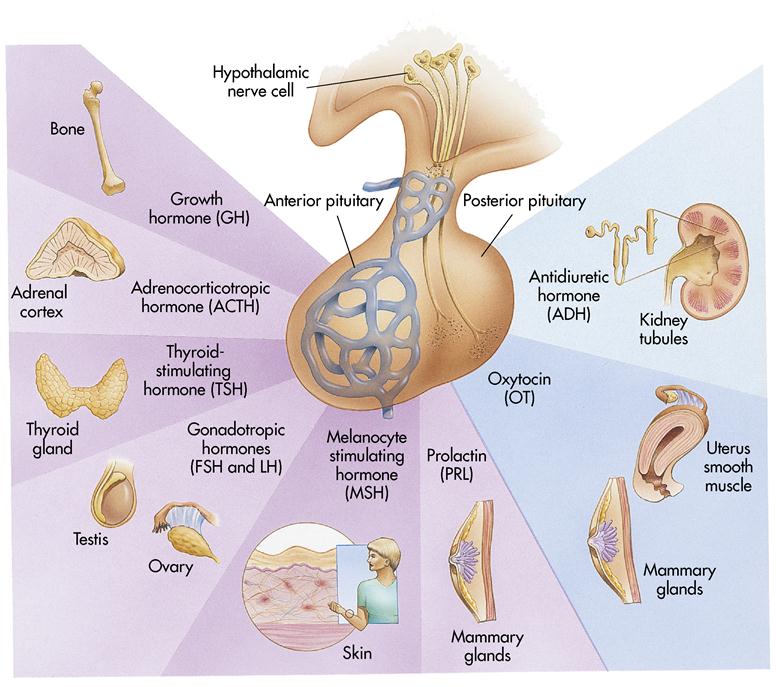
Posterior pituitary gland
Two hormones are released by the posterior pituitary when the hypothalamus stimulates their release. They are oxytocin and antidiuretic hormone (ADH) (see Figure 11-2). Oxytocin promotes the release of milk and stimulates uterine contractions during labor. ADH, also called vasopressin, causes the kidneys to conserve water by decreasing the amount of urine produced. ADH/vasopressin also causes constriction of the arterioles in the body and a pressor effect, which results in increased blood pressure.
Thyroid gland
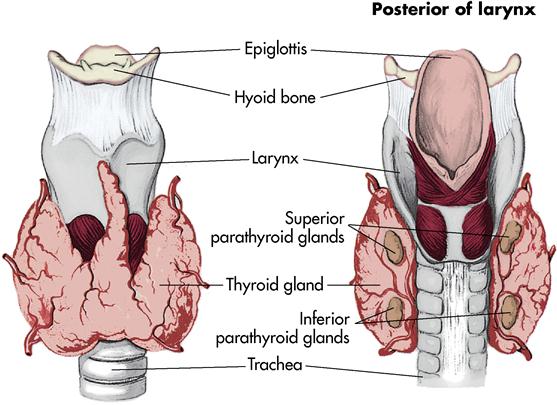
The thyroid gland is butterfly shaped, with one lobe lying on either side of the trachea just below the larynx (Figure 11-4). The lobes are connected by the isthmus. The gland is very vascular and receives approximately 80 to 120 mL of blood per minute.
The thyroid gland secretes the hormones thyroxine (T4) and triiodothyronine (T3). Adequate oral intake of iodine is necessary for the formation of thyroid hormones. These hormones regulate three main functions: (1) growth and development, (2) metabolism, and (3) activity of the nervous system. Their function is controlled by the release of thyroid-stimulating hormone (TSH) from the pituitary gland.
Calcitonin is a hormone also released by the thyroid gland. It decreases blood calcium levels by causing calcium to be stored in the bones.
Parathyroid glands
The four parathyroid glands are located on the posterior surface of the thyroid gland (see Figure 11-4) and secrete parathyroid hormone (PTH, parathormone). As an antagonist to calcitonin from the thyroid, PTH tends to increase the concentration of calcium in the blood. It also regulates the amount of phosphorus in the blood.
The delicate balance of calcium in the blood is extremely important for normal body function. When calcium blood levels are low, the nerve cells become excited and stimulate the muscles with too many impulses, resulting in spasms (tetany). When blood calcium levels are abnormally high, heart function becomes impaired; this can result in death. Under the influence of PTH, two changes occur in the kidneys: It increases the reabsorption of calcium and magnesium from the kidney tubules and accelerates the elimination of phosphorus in the urine.
Adrenal glands
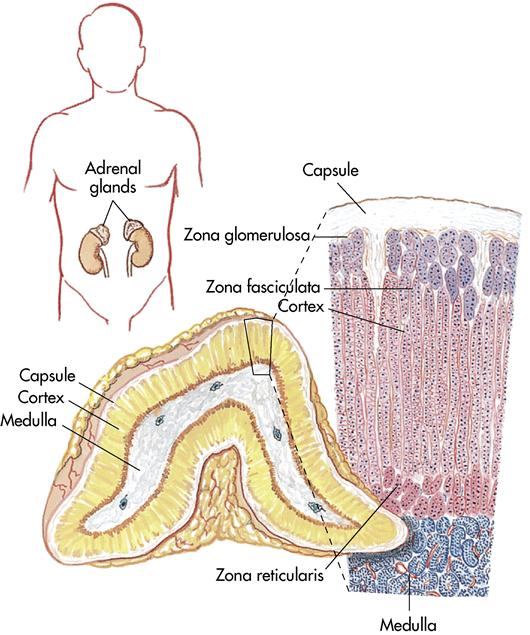
The adrenal glands (suprarenal glands) are small, yellow masses that lie atop the kidneys. Both glands contain an outer section, the adrenal cortex, and a smaller inner section, the adrenal medulla (Figure 11-5).
Adrenal cortex
The adrenal cortex is divided into three separate layers. Each layer secretes a particular hormone, called a steroid:
Adrenal medulla
The cells composing the adrenal medulla arise from the same type of cells as the sympathetic nervous system. Two hormones are released during times of stress: (1) epinephrine (adrenaline), and (2) norepinephrine. They cause the heart rate and blood pressure to increase, the blood vessels to constrict, and the liver to release glucose reserves for immediate energy. This is a systemic preparation of the body for a “fight-or-flight” response needed in times of crisis.
Pancreas
The pancreas is an elongated gland that lies posterior to the stomach. It is an active organ, composed of both exocrine and endocrine tissue. The endocrine tissue of the pancreas contains more than a million tiny clusters of cells known collectively as the islets of Langerhans. These cells secrete two major hormones. The first, insulin, is secreted by the beta cells in response to increased levels of glucose in the blood. Insulin’s secretion pattern is a physiologic example of negative feedback between insulin and glucose. Elevated blood glucose levels stimulate the pancreas to secrete insulin. The stimulus for insulin secretion decreases as blood glucose levels decrease. The homeostatic mechanism is considered negative feedback because it reverses the change in blood glucose level. The second pancreatic hormone is glucagon, which is secreted by the alpha cells in response to decreased levels of glucose in the blood. Insulin and glucagon play a major role in carbohydrate, fat, and protein metabolism.
Female sex glands
Deep in the lower abdominal region, lying to the left and the right of the uterus, are two almond-shaped ovaries, the major sex glands of the woman. At puberty the ovaries begin producing two hormones: estrogen (responsible for the development of secondary sex characteristics, such as axillary hair and pubic hair, and for maturation of the reproductive organs) and progesterone (continues the preparation of the reproductive organs that was initiated by the estrogen). (See Chapter 12 for more information.)
The placenta is a temporary endocrine gland that forms and functions during pregnancy. During this time the ovaries become inactive and the placenta releases the estrogen and progesterone needed to maintain the pregnancy. (For a more in-depth discussion, refer to Chapter 12.)
Male sex glands
Suspended outside the body in the scrotum, a saclike structure, are the two oval sex glands called the testes. They release the hormone testosterone, which is responsible for the development of the male secondary sex characteristics, including axillary, pubic, and facial hair; maturation of the reproductive organs; deepening of the voice; and development of muscle and bone mass. Testosterone is necessary for sperm formation.
Thymus gland
The thymus gland lies in the upper thorax, posterior to the sternum (see Figure 11-1). It produces the hormone thymosin, which plays an active role in the immune system. T lymphocytes (a type of white blood cell) are stimulated to carry out immune reactions to certain types of antigens. The thymus gland programs this information into the T lymphocytes in utero and during the first few months of life.
Pineal gland
The pineal gland is a small, cone-shaped gland located in the roof of the third ventricle of the brain (see Figure 11-1). It secretes the hormone melatonin, which seems to inhibit reproductive activities by inhibiting the gonadotropic hormones. This is particularly important in preventing the sexual maturation of the child’s body until adulthood. It is thought to induce sleep, may affect mood, and has an impact on menstrual cycles.
Disorders of the pituitary gland (hypophysis)
Acromegaly
Etiology and pathophysiology
An overproduction of somatotropin (growth hormone [GH]) in the adult causes acromegaly, a condition that affects an estimated 250 people in the United States each year. The cause may be either (1) idiopathic hyperplasia (an increase in number of cells without a known cause) of the anterior lobe of the pituitary gland or (2) tumor growth. Unfortunately, growth changes that occur in acromegaly are irreversible, even with adequate medical or surgical intervention.
Clinical manifestations
Manifestations of acromegaly begin gradually, usually in the third or fourth decade of life. Typically an average of 7 to 9 years passes between the initial onset of signs and symptoms and final diagnosis. The subsequent overabundance of GH produces many changes throughout the patient’s body, including enlarged cranium and lower jaw, separated and maloccluded teeth, bulging forehead, bulbous nose, thick lips, enlarged tongue, and generalized coarsening of the facial features (Figure 11-6). Enlargement of the tongue results in speech difficulties, and the voice deepens as a result of hypertrophy of the vocal cords. The hands and feet grow larger; the fingertips develop a tufted or clubbed appearance (Lewis et al., 2007). There is enlargement of the heart, the liver, and the spleen. Muscle weakness usually develops. Joints may hypertrophy and become painful and stiff. Male patients may become impotent, and female patients may develop a deepened voice, increased facial hair, and amenorrhea. If a tumor is present, pressure on the optic nerve may cause partial or complete blindness. Severe headaches are common.
Assessment
Subjective data include headaches or visual disturbances and painful, stiff joints. Evaluate muscle weakness and its effect on the patient’s ability to perform activities. Encourage patients to share their emotional responses to sexual problems (such as impotence in men and masculinization in women).
Collection of objective data includes ongoing assessment of bone enlargement and joint involvement, evidenced by gait changes and decreasing ability to perform activities. Changes in vital signs that may herald the onset of early heart failure include dyspnea, tachycardia, weak pulse, and hypotension.
Diagnostic tests
Diagnosis of acromegaly is based on the history and the clinical manifestations, computed tomography (CT) scan, magnetic resonance imaging (MRI), and cranial radiographic evaluation. A complete ophthalmologic examination, including visual fields, is usually performed because a large tumor of the pituitary gland potentially causes pressure on the optic chiasm or optic nerves. Laboratory tests confirm the elevated levels of serum GH and plasma insulin-like growth factor–1. The definitive test for acromegaly is the oral glucose challenge test. Normally GH concentration falls during an oral glucose challenge test, but in acromegaly these levels do not fall (Lewis et al., 2007). Restrict the patient’s oral intake for 8 hours before this test.
Medical management
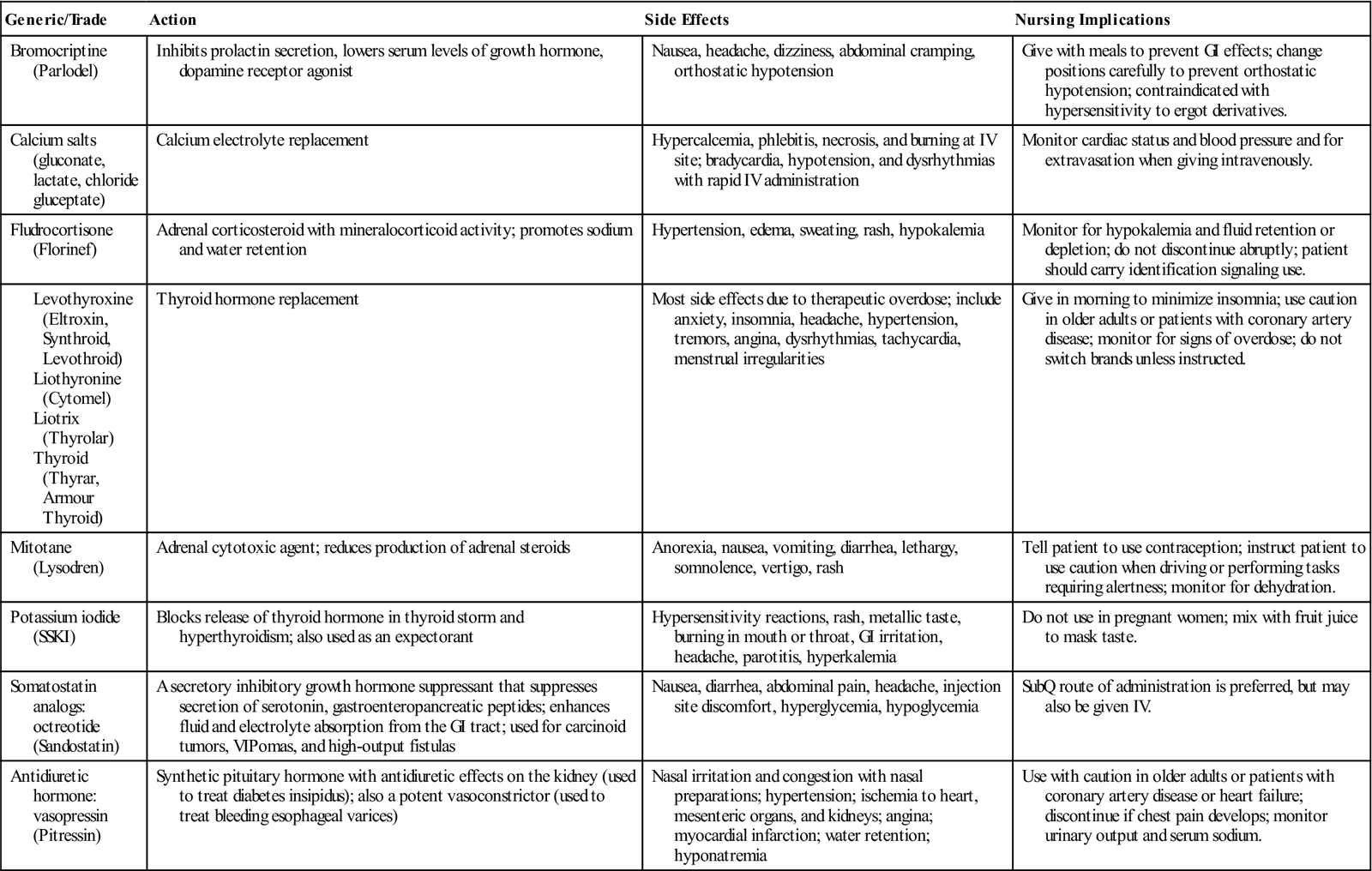
Medical treatments include dopamine agonists such as cabergoline (Dostinex) and somatostatin analogs (which inhibit GH), such as octreotide (Sandostatin, Sandostatin Depot) (Table 11-1), especially in patients who are not candidates for surgery or radiation therapy. These drugs are used in an attempt to suppress GH secretion. Surgical treatment to remove pituitary tumors associated with acromegaly is accomplished with the transsphenoidal removal of tumor tissue. The goal of transsphenoidal surgery is to remove only the tumor that is causing GH secretion. Irradiation procedures using proton beam therapy have been used to destroy GH-secreting tumors. Proton beam treatment uses very low doses of radiation and therefore is much less destructive to adjacent tissues, such as the hypothalamus and temporal lobes, than conventional radiation therapy.
![]() Table 11-1
Table 11-1
Medications for Endocrine Disorders
Nursing interventions and patient teaching
Nursing interventions are mainly supportive. Muscle weakness, joint pain, or stiffness warrant assessment of the ability to perform activities of daily living (ADLs). Headache may impair the patient’s ability to socialize and may also impede education. Worsening headaches may indicate tumor progression. The diet should be soft and easy to chew, since jaw muscles and the temporomandibular joint may be involved. Encourage the patient to chew thoroughly, and allow adequate time during meals, assisting when necessary. Encourage frequent fluid intake. Nonopioid analgesics may be given for pain relief. Visual impairment may increase the risk of injury for these patients, so take care to prevent them from stumbling into furniture or dropping objects.
As the body changes, the patient may develop problems with self-esteem and may feel physically unattractive. He or she may have difficulty communicating with significant others, which can disrupt individual or family coping methods. Other complications of acromegaly are related to enlargement of the liver, the spleen, and the heart. Cardiac dysrhythmias may develop, and the patient may experience heart failure. Abdominal girth may increase as a result of weight gain and inactivity, and respiratory difficulty may occur.
Nursing diagnoses and interventions for the patient with acromegaly include but are not limited to the following:
| Nursing Diagnoses | Nursing Interventions |
| Disturbed body image, related to enlargement of hands, feet, tongue, jaw, and soft tissue | |
| Activity intolerance, related to physical weakness |
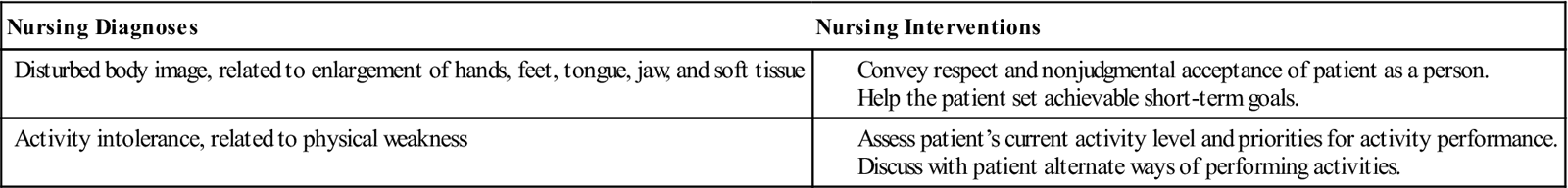
The patient should remain under the supervision of a physician so that any complications can be promptly diagnosed and adequately treated. Teach the patient exercises that can be performed at home, such as active range-of-motion of joints of the extremities and of the neck, to help prevent muscle atrophy and loss of movement.
Prognosis
Even with adequate medical or surgical treatment, the physical changes are irreversible, and the patient is prone to developing complications.
Gigantism
Etiology and pathophysiology
Gigantism usually results from an oversecretion of GH as a result of hyperplasia of the anterior pituitary; this hyperplastic tissue may develop into a tumor. Another possible cause is a defect in the hypothalamus, which directs the anterior pituitary to release excess amounts of GH.
Clinical manifestations
When overproduction of GH occurs in a child before closure of the epiphyses, there is an overgrowth of the long bones. This results in the attainment of great height, accompanied by increased muscle and visceral development. Weight increases, but body proportions are usually normal. Despite their size, these patients are usually weak. Other kinds of gigantism may be caused by certain genetic disorders or by disturbances in sex hormone production. Once identified, these children should be referred for further medical evaluation and follow-up.
Assessment
Collection of subjective data includes assessment of the patient’s understanding of the disease process and his or her ability to verbalize emotional responses.
Collection of objective data requires frequent measurement of height. Assess the patient’s use of adaptive coping measures and family interactions.
Diagnostic tests
The GH-suppression test (also called the glucose-loading test) may be done to evaluate GH levels. In the patient with gigantism, baseline levels of GH are high.
Medical management
Medical management of children with gigantism may include surgical removal of tumor tissue or irradiation of the anterior pituitary gland, with subsequent replacement of pituitary hormones as indicated. The physician then observes the child for the development of related complications, such as hypertension, heart failure, osteoporosis, thickened bones, and delayed sexual development.
Nursing interventions and patient teaching
Nursing interventions primarily include early identification of children who are experiencing increased growth rates compared with other children their age. The condition causes potential problems with self-image, especially if the child is a preteen who is a great deal taller than peers. Girls usually suffer more emotional trauma in this situation than boys do. Be understanding and compassionate and accentuate the positive aspects of being tall.
Early diagnosis of these patients is essential, since proper medical management can retard the height a child will reach. Stress to the parents the importance of regular visits to the pediatrician or pediatric endocrinologist (a physician who specializes in endocrinology).
Prognosis
With new medical and surgical advances, the expected life span of these patients is longer than it was previously. However, their life expectancy is still shorter than that of the average individual.
Dwarfism
Etiology and pathophysiology
Hypopituitary dwarfism is a condition caused by deficiency in GH. Most cases are idiopathic, but a small number can be attributed to an autosomal recessive trait. In some cases the patients also lack adrenocorticotropic hormone (ACTH), TSH, and the gonadotropins.
Clinical manifestations
The most common clinical manifestation of dwarfism is that the child is a great deal shorter than his or her peers. These patients usually appear well proportioned and well nourished but appear younger than their chronologic age. They may have problems with dentition as the permanent teeth erupt, since the jaws are underdeveloped. Sexual development is usually normal but delayed. Many people with hypopituitary dwarfism are able to reproduce normal offspring, unless there is an accompanying deficiency in gonadotropins. Because only a small number of children who experience short stature or delayed growth suffer from dwarfism, a thorough diagnostic workup is crucial.
Assessment
Subjective data include the patient’s understanding of the disease process and emotional responses to it. A family history of dwarfism may reveal previously successful coping strategies. Encourage the patient to verbalize feelings. Most of these children display normal intelligence. The child’s history usually reveals a normal birth weight. It is important to determine when the child’s growth retardation was first noted.
Collection of objective data includes regular measurement of height and weight to determine responses to GH and other hormones that may be administered. Compare current height and weight with standard growth charts, and compare the child’s growth pattern with that of siblings and other relatives at comparable age periods.
Diagnostic tests
Diagnostic tests include radiographic evaluation of the wrist for bone age and an MRI or a CT scan to rule out a pituitary tumor. Definitive diagnosis is based on decreased plasma levels of GH. Restrict the patient’s oral intake after midnight for this test.
Medical management
Medical treatment involves replacement of GH by injection and the addition of other hormones as needed to correct deficiencies. If a tumor is the cause of dwarfism, surgery is usually indicated.
Nursing interventions and patient teaching
Exercise particular care to identify children with growth problems. The physician correlates the onset of growth retardation with symptoms of headache, visual disturbances, or behavior changes that might indicate tumor, so be alert for these symptoms. Be careful not to make the parents feel guilty about any delay in seeking medical attention for their child.
Encourage the child to wear age-appropriate clothing and engage in activities with peers, since major problems with self-esteem can occur in dwarfism. Emphasize the child’s abilities and strengths instead of his or her physical size.
Prognosis
Most of these patients lead fairly normal lives, and many become parents of normal children. Complications experienced are often of the musculoskeletal and cardiovascular systems.
Diabetes insipidus
Etiology and pathophysiology
Diabetes insipidus (diabetes, “like a sieve or siphon”; and insipidus, “tasteless”) is a transient or permanent metabolic disorder of the posterior pituitary in which ADH is deficient. The condition may be either primary or secondary to other conditions, such as head injury, intracranial tumor, intracranial aneurysm, or infarct. Infections such as encephalitis or meningitis have been known to cause diabetes insipidus. Diabetes insipidus occurs when either the secretion or action of ADH goes awry. A decrease in ADH results in electrolyte and fluid imbalances. The imbalances are caused by increased plasma osmolality and increased urinary output.
Clinical manifestations
Diabetes insipidus is characterized by marked polyuria and intense polydipsia. The urine is very dilute, looking much like water, with a low specific gravity (1.001 to 1.005; the normal range is 1.003 to 1.030). Urinary output may exceed 5 to 20 L/24 hr, whereas the average is 1.5 L/24 hr. Patients typically lose as much as 200 mL of urine an hour for more than 2 consecutive hours. The patient craves cold or iced water and may drink 4 to 20 L of fluid daily, yet may become severely dehydrated and have increased levels of sodium in the blood (hypernatremia). Even when unconscious after surgery or head trauma, these patients continue to produce copious quantities of urine. If untreated, diabetes insipidus can lead to signs and symptoms of hypovolemic shock, including changes in level of consciousness, tachycardia, tachypnea, and hypotension. However, unlike hypovolemic shock, diabetes insipidus causes an increase in urinary output rather than a decrease.
Assessment
Subjective data include the patient’s understanding of the relationship of symptoms (such as thirst and polyuria) to the underlying cause. The patient should be able to state the importance of not restricting oral fluids. Assess the severity of thirst. The patient may be embarrassed about the constant need to drink and then empty the bladder and may voluntarily restrict social contacts and work activities. The patient is weak, tired, and lethargic.
Collection of objective data includes assessment of skin turgor (the normal resiliency of the skin) and color and specific gravity of the urine. Carefully monitor intake and output (I&O). The skin is dry, turgor is poor, and body weight is lost. Constipation may occur. Weigh the patient daily in the early morning, before breakfast. Determine whether the patient has nocturia.
Diagnostic tests
Diagnosis is based on clinical manifestations, urine specific gravity, and urine ADH measurement. The urine specific gravity often drops below 1.003, and the serum sodium level increases to more than 145 mEq/L (normal serum sodium level is 135 to 145 mEq/L). The serum osmolality may be greater than 300 mOsm/kg (normal is 280 to 300 mOsm/kg). The fluid deprivation (water deprivation) test may be ordered to determine how well the pituitary is producing ADH and to help rule out other causes. A CT scan and radiographic evaluation of the sella turcica (the “Turkish saddle”–shaped depression in the sphenoid bone that houses the pituitary gland) may be done.
Medical management
Medical treatment involves intravenous (IV), subcutaneous, intranasal, or oral administration of ADH preparations in the form of desmopressin acetate (DDAVP). Several other drugs are available for ADH replacement, including aqueous vasopressin (Pitressin intramuscular [IM] or intranasal), vasopressin tannate IM, and lypressin (Diapid intranasal). Coffee, tea, and other beverages containing caffeine are usually eliminated from the diet because of their possible diuretic effect. If the patient cannot match the urinary losses through oral intake, he or she is at risk for dehydration and severe hypernatremia. IV fluids of hypotonic saline or dextrose 5% in water are needed.
Nursing interventions and patient teaching
Because of the potential for fluid volume deficiency, carefully monitor the urinary output of pediatric and unconscious patients. Assess skin turgor frequently, along with the condition of oral mucous membranes. Weigh the patient and record I&O daily. Do not limit oral fluids in an effort to reduce urinary output.
Nursing diagnoses and interventions for the patient with diabetes insipidus include but are not limited to the following:
| Nursing Diagnoses | Nursing Interventions |
| Deficient fluid volume, risk for, related to excessive urine production | Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
 s-F
s-F -j
-j –
– ,
,  l-
l- -F
-F -j
-j ,
,  l-
l- –
– -r
-r –
– ,
,  R-g
R-g r,
r,