Pressure ulcers
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Describe the causes and risk factors for pressure ulcers.
• Identify the persons at risk for pressure ulcers.
• Describe the stages of pressure ulcers.
• Identify the sites for pressure ulcers.
• Explain how to prevent pressure ulcers.
• Identify the complications from pressure ulcers.
Key terms
avoidable pressure ulcer A pressure ulcer that develops from the improper use of the nursing process
bedfast Confined to bed
bony prominence An area where the bone sticks out or projects from the flat surface of the body
chairfast Confined to a chair
eschar Thick, leathery dead tissue that may be loose or adhered to the skin; it is often black or brown
friction The rubbing of one surface against another
unavoidable pressure ulcer A pressure ulcer that occurs despite efforts to prevent one through proper use of the nursing process
KEY ABBREVIATIONS
| CMS | Centers for Medicare & Medicaid Services |
| TJC | The Joint Commission |
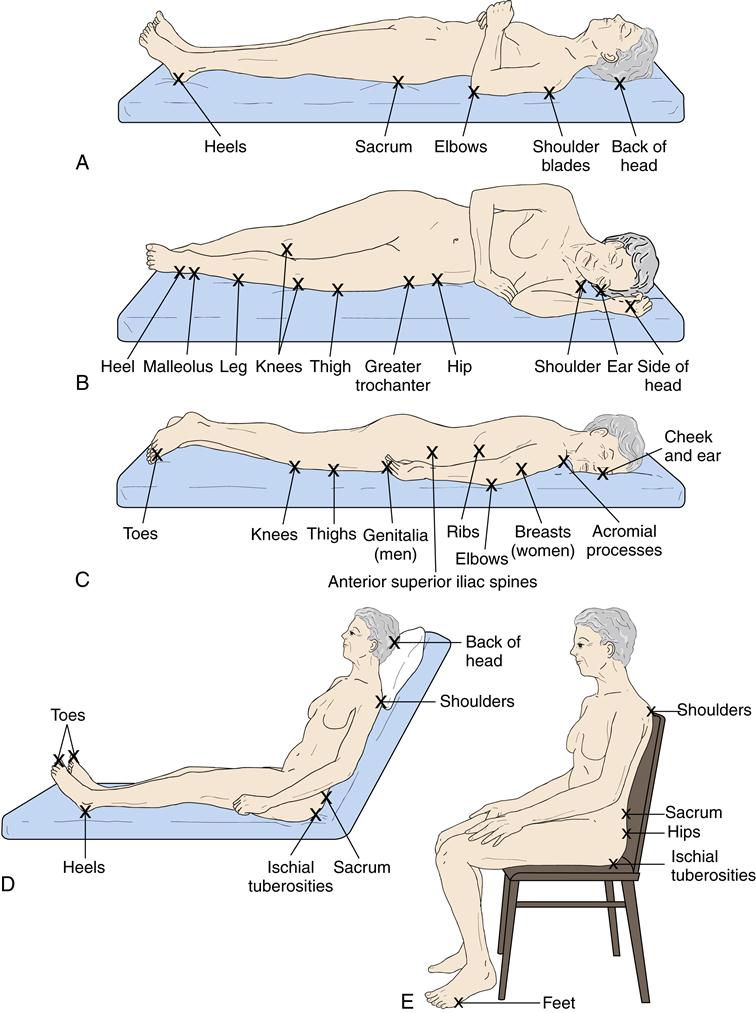
The National Pressure Ulcer Advisory Panel (NPUAP) defines a pressure ulcer as a localized injury to the skin and/or underlying tissue usually over a bony prominence (Fig. 36-1). It is the result of pressure or pressure in combination with shear. Prominence means to stick out. A bony prominence is an area where the bone sticks out or projects from the flat surface of the body. The back of the head, shoulder blades, elbows, hips, spine, sacrum, knees, ankles, heels, and toes are bony prominences (Fig. 36-2). Decubitus ulcer, bed sore, or pressure sore are other terms for pressure ulcer.
![]() The Centers for Medicare & Medicaid Services (CMS) defines a pressure ulcer as any lesion caused by unrelieved pressure that results in damage to underlying tissues. According to the CMS, friction and shear are not the main causes of pressure ulcers. However, friction and shear are important contributing factors. Shear is when layers of the skin rub against each other. Or shear is when the skin remains in place and underlying tissues move and stretch and tear underlying capillaries and blood vessels. Tissue damage occurs. Friction is the rubbing of one surface against another. The skin is dragged across a surface. Friction is always present with shearing.
The Centers for Medicare & Medicaid Services (CMS) defines a pressure ulcer as any lesion caused by unrelieved pressure that results in damage to underlying tissues. According to the CMS, friction and shear are not the main causes of pressure ulcers. However, friction and shear are important contributing factors. Shear is when layers of the skin rub against each other. Or shear is when the skin remains in place and underlying tissues move and stretch and tear underlying capillaries and blood vessels. Tissue damage occurs. Friction is the rubbing of one surface against another. The skin is dragged across a surface. Friction is always present with shearing.
The CMS has standards focusing on pressure ulcers. Some persons are admitted to the center with pressure ulcers. They come from hospitals or from home. According to the CMS, nursing centers must ensure that:
• A person does not develop a pressure ulcer after entering the center. However, for some persons, developing a pressure ulcer cannot be avoided. A pressure ulcer occurs despite efforts to prevent one through proper use of the nursing process. This is called an unavoidable pressure ulcer. An avoidable pressure ulcer is one that develops from the improper use of the nursing process. The center must:
• Evaluate the person’s condition and pressure ulcer risk factors.
• Identify and implement measures that meet the resident’s needs and goals.
• Monitor and evaluate the effect of such measures.
• Revise the measures as needed.
Centers must identify persons at risk for developing pressure ulcers. Some persons are at greater risk than others. And the person’s risk may increase during an illness (cold, flu) or when his or her condition changes. Many pressure ulcers occur within the first 4 weeks of admission to a nursing center. A person at risk can develop a pressure ulcer within 2 to 6 hours after the onset of pressure. The center must develop a comprehensive care plan to meet the person’s needs. The care plan must include measures to reduce or remove the person’s risk factors.
Risk factors
Pressure is the major cause of pressure ulcers. Shearing and friction are important factors. They also cause skin breakdown (Box 36-1) that can lead to a pressure ulcer. Risk factors include breaks in the skin, poor circulation to an area, moisture, dry skin, and irritation by urine and feces. Older and disabled persons are at great risk for pressure ulcers. Their skin is easily injured. Causes include age-related skin changes, chronic disease, and general debility.
Unrelieved pressure squeezes tiny blood vessels. The skin does not receive oxygen and nutrients. Tissues die and a pressure ulcer forms when the skin is starved of oxygen and nutrients for too long. For example, pressure occurs when the skin over a bony area is squeezed between hard surfaces (Fig. 36-3). The bone is one hard surface. The other is usually the mattress or chair seat. Squeezing or pressure prevents blood flow to the skin and underlying tissues. Oxygen and nutrients cannot get to the cells. Involved skin and tissues die.
Friction scrapes the skin, causing an open area. The open area needs to heal. A good blood supply is needed. A poor blood supply or an infection can lead to a pressure ulcer.
Shear occurs when the person slides down in the bed or chair. Blood vessels and tissues are damaged. Blood flow to the area is reduced.
Persons at risk
Persons at risk for pressure ulcers are those who:
• Have poor fluid balance. Fluid balance is needed for healthy skin.
• Are obese or very thin. Friction can damage the skin.
• Refuse care. ![]() The person needs proper care to prevent pressure ulcers. The CMS requires that the person make informed choices. The center and resident must discuss the person’s condition, treatment options, expected outcomes, and problems from refusing treatment. The center must address the person’s concerns and offer options if a certain treatment is refused. The presence of a “Do Not Resuscitate” order (Chapter 48) does not mean the person is refusing measures to prevent or treat a pressure ulcer. It only means that the person will not be resuscitated in the event of a cardiac or respiratory arrest.
The person needs proper care to prevent pressure ulcers. The CMS requires that the person make informed choices. The center and resident must discuss the person’s condition, treatment options, expected outcomes, and problems from refusing treatment. The center must address the person’s concerns and offer options if a certain treatment is refused. The presence of a “Do Not Resuscitate” order (Chapter 48) does not mean the person is refusing measures to prevent or treat a pressure ulcer. It only means that the person will not be resuscitated in the event of a cardiac or respiratory arrest.
• ![]() Have a healed pressure ulcer. According to the CMS, areas of healed Stage 3 or 4 pressure ulcers are more likely to recur. See “Pressure Ulcer Stages.”
Have a healed pressure ulcer. According to the CMS, areas of healed Stage 3 or 4 pressure ulcers are more likely to recur. See “Pressure Ulcer Stages.”
Pressure ulcer stages
In persons with light skin, a reddened bony area is the first sign of a pressure ulcer. In persons with dark skin, skin color may differ from surrounding areas. The color change remains after the pressure is relieved. The area may feel warm or cool. The person may complain of pain, burning, tingling, or itching in the area. Some persons do not feel anything unusual. Box 36-2 describes pressure ulcer stages.