Wound care
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Describe the process and complications of wound healing.
• Describe what to observe about wounds.
• Explain how to secure dressings.
• Explain the rules for applying dressings.
• Explain the purpose of binders and how to apply them.
• Explain the purpose, effects, and complications of heat and cold applications.
• Describe the rules for applying heat and cold.
• Describe how to meet the basic needs of persons with wounds.
• Perform the procedures described in this chapter.
Key terms
abrasion A partial-thickness wound caused by the scraping away or rubbing of the skin
arterial ulcer An open wound on the lower legs or feet caused by poor arterial blood flow
chronic wound A wound that does not heal easily
circulatory ulcer An open sore on the lower legs or feet caused by decreased blood flow through the arteries or veins; vascular ulcer
clean-contaminated wound Occurs from the surgical entry of the reproductive, urinary, respiratory, or gastro-intestinal system
clean wound A wound that is not infected
closed wound Tissues are injured but the skin is not broken
compress A soft pad applied over a body area
constrict To narrow
contaminated wound A wound with a high risk of infection
contusion A closed wound caused by a blow to the body; a bruise
dehiscence The separation of wound layers
diabetic foot ulcer An open wound on the foot caused by complications from diabetes
dilate To expand or open wider
dirty wound See “infected wound”
edema Swelling caused by fluid collecting in tissues
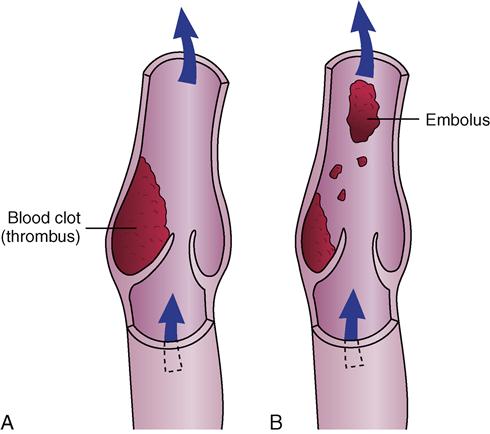
embolus A blood clot that travels through the vascular system until it lodges in a vessel
evisceration The separation of the wound along with the protrusion of abdominal organs
full-thickness wound The dermis, epidermis, and subcutaneous tissue are penetrated; muscle and bone may be involved
gangrene A condition in which there is death of tissue
hyperthermia A body temperature (thermia) that is much higher (hyper) than the person’s normal range
hypothermia A very low (hypo) body temperature (thermia)
incision A cut produced surgically by a sharp instrument; it creates an opening into an organ or body space
infected wound A wound containing large amounts of microbes that shows signs of infection; a dirty wound
intentional wound A wound created for therapy
laceration An open wound with torn tissues and jagged edges
open wound The skin or mucous membrane is broken
pack Wrapping a body part with a wet or dry application
partial-thickness wound The dermis and epidermis of the skin are broken
penetrating wound An open wound that breaks the skin and enters a body area, organ, or cavity
phlebitis Inflammation (itis) of a vein (phleb)
puncture wound An open wound made by a sharp object
purulent drainage Thick green, yellow, or brown drainage
sanguineous drainage Bloody (sanguis) drainage
serosanguineous drainage Thin, watery drainage (sero) that is blood-tinged (sanguineous)
serous drainage Clear, watery fluid (serum)
stasis ulcer See “venous ulcer”
thrombus A blood clot
trauma An accident or violent act that injures the skin, mucous membranes, bones, and organs
ulcer A shallow or deep crater-like sore of the skin or a mucous membrane
unintentional wound A wound resulting from trauma
vascular ulcer See “circulatory ulcer”
venous ulcer An open sore on the lower legs or feet caused by poor venous blood flow; stasis ulcer
wound A break in the skin or mucous membrane
KEY ABBREVIATIONS
| C | Centigrade |
| F | Fahrenheit |
| GI | Gastro-intestinal |
| ID | Identification |
| PPE | Personal protective equipment |
A wound is a break in the skin or mucous membrane. Common causes are:
• Surgery
• Pressure ulcers from unrelieved pressure (Chapter 36).
• Decreased blood flow through the arteries or veins.
Infection is a major threat. Wound care involves preventing infection and further injury to the wound and nearby tissues. Blood loss and pain also are prevented.
The nurse uses the nursing process to keep the person’s skin healthy. Some centers have a skin care team to manage all skin problems. The team includes an RN, physical therapist, and a dietitian.
See Focus on Rehabilitation: Wound Care.
Types of wounds
Types of wounds are described in Box 35-1. Wounds also are described by their cause:
• Abrasion—a partial-thickness wound caused by the scraping away or rubbing of the skin (Fig. 35-1).
• Contusion—a closed wound caused by a blow to the body (a bruise) (Fig. 35-2).
• Incision—a cut produced surgically by a sharp instrument. It creates an opening into an organ or body space (Fig. 35-3, p. 538).
• Laceration—an open wound with torn tissues and jagged edges (Fig. 35-4, p. 538).
• Penetrating wound—an open wound that breaks the skin and enters a body area, organ, or cavity (Fig. 35-5, p. 538).
• Puncture wound—an open wound made by a sharp object (knife, nail, metal, wood, glass). Entry of the skin and underlying tissues may be intentional or unintentional. See Figure 35-6, p. 538.
• Ulcer—a shallow or deep crater-like sore of the skin or a mucous membrane (p. 539).
Skin tears
A skin tear is a break or rip in the outer layers of the skin (Fig. 35-7). The epidermis (top skin layer) separates from the underlying tissues (Chapter 9). The skin is “peeled back.” The hands, arms, and lower legs are common sites for skin tears. Very thin and fragile skin is common in older persons. Slight pressure can cause a skin tear.

Causes
• Friction, shearing (Chapter 17), pulling, or pressure on the skin.
• Holding the person’s arm or leg too tight.
• Bathing, dressing, and other tasks.
• Pulling buttons and zippers across fragile skin.
• Jewelry—yours or the person’s. Rings, watches, and bracelets are examples.
Skin tears are painful. They are portals of entry for microbes. Infection is a risk. Tell the nurse at once if you cause or find a skin tear.
Persons at risk
Persons at risk for skin tears:
See Residents With Dementia: Persons at Risk (Skin Tears).
Prevention and treatment
Careful and safe care helps prevent skin tears and further injury. Follow the measures in Box 35-2. Also follow the care plan and the nurse’s directions. They may include dressings (p. 550) and elastic bandages (p. 543) to protect the skin and promote healing.
Circulatory ulcers
Some diseases affect blood flow to and from the legs and feet. Such poor circulation can lead to pain, open wounds, and edema. Edema is swelling caused by fluid collecting in tissues. Infection and gangrene can result from the open wound and poor circulation. Gangrene is a condition in which there is death of tissue.
Circulatory ulcers (vascular ulcers) are open sores on the lower legs or feet. They are caused by decreased blood flow through the arteries or veins. Persons with diseases affecting the blood vessels are at risk. These wounds are painful and hard to heal.
The doctor orders drugs and treatments as needed. The nurse uses the nursing process to meet the person’s needs (Box 35-3, p. 540). You must help prevent skin breakdown on the legs and feet.
Venous ulcers
Venous ulcers (stasis ulcers) are open sores on the lower legs or feet. Stasis means stopped or slowed fluid flow. These ulcers are caused by poor venous blood flow (Fig. 35-8, p. 540).

Venous ulcers can develop when valves in the leg’s veins do not close well. The veins do not pump blood back to the heart in a normal way. Blood and fluid collect in the legs and feet. Small skin veins rupture. This allows hemoglobin to enter the tissue, causing the skin to turn brown. (Hemoglobin gives blood its red color.) The skin is dry, leathery, and hard. Itching is common.
The heels and inner part of the ankles are common sites for venous ulcers. They can occur from skin injury. Scratching is an example. Or they can occur without trauma.
Venous ulcers are painful and walking is difficult. Fluid may seep from the wound. Infection is a risk. Healing is slow.
Risk factors
Risk factors for venous ulcers include:
Prevention and treatment
• Follow the care plan to prevent skin breakdown. See the measures in Box 35-3.
• Prevent injury. Do not bump the legs and feet.
• Handle, move, and transfer the person carefully and gently.
Persons at risk need professional foot care. Attention is given to toenails, corns, calluses, and other toe and foot problems. You do not cut the toenails of persons with diseases affecting the circulation.
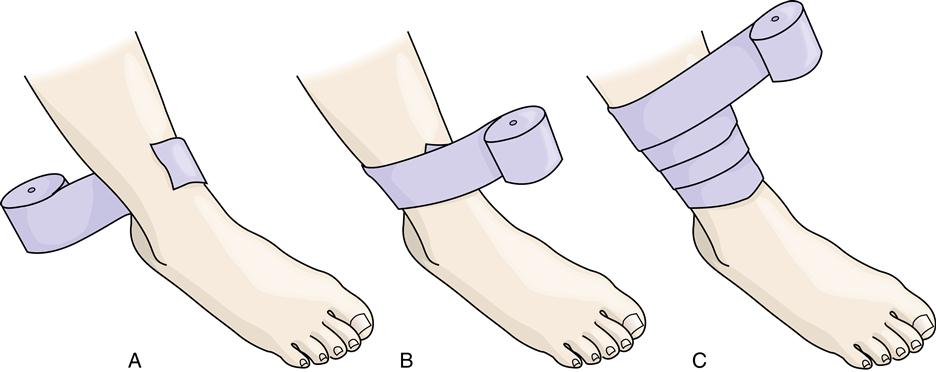
Venous ulcers are hard to heal. The doctor may order drugs for infection and to decrease swelling. Medicated bandages and other wound care products are often ordered. So are devices used for pressure ulcers. The doctor may order elastic stockings or elastic bandages to:
• Promote circulation by providing support and pressure to the veins
 Elastic stockings.
Elastic stockings.
Elastic stockings exert pressure on the veins. The pressure promotes venous blood return to the heart. The stockings help prevent venous ulcers and blood clots in leg veins.