Respiratory support and therapies
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Explain how to assist in the care of persons with artificial airways.
• Describe the principles and safety measures for suctioning.
• Explain how to assist in the care of persons on mechanical ventilation.
• Explain how to assist in the care of persons with chest tubes.
Key terms
hemothorax Blood (hemo) in the pleural space (thorax)
intubation Inserting an artificial airway
mechanical ventilation Using a machine to move air into and out of the lungs
patent Open and unblocked
pleural effusion The escape and collection of fluid (effusion) in the pleural space
pneumothorax Air (pneumo) in the pleural space (thorax)
suction The process of withdrawing or sucking up fluid (secretions)
tracheostomy A surgically created opening (stomy) into the trachea (tracheo)
KEY ABBREVIATIONS
| CO2 | Carbon dioxide |
| ET | Endotracheal |
| O2 | Oxygen |
Some persons need artificial airways, suctioning, mechanical ventilation, and chest tubes. Needing respiratory rehabilitation, often they are very ill. They need to recover from problems affecting the airway and lungs. They need complex procedures and equipment.
The nurse may ask you to assist in their care. The center must teach and train you to provide needed care. The goals of care are to help the person:
Artificial airways
Artificial airways keep the airway patent (open and unblocked). They are needed:
• When disease, injury, secretions, or aspiration obstructs the airway
• For mechanical ventilation (p. 461)
Intubation means inserting an artificial airway. Such airways are usually plastic and disposable. They come in various sizes. These airways are common:
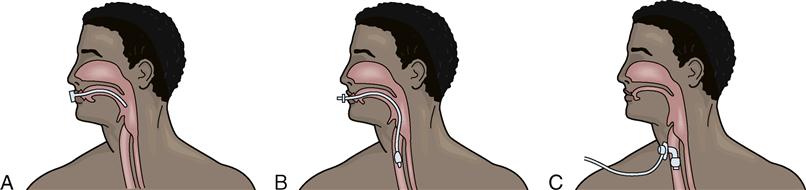
• Oropharyngeal airway—inserted through the mouth and into the pharynx (Fig. 29-1, A). A nurse or respiratory therapist inserts the airway.
• Endotracheal (ET) tube—inserted through the mouth or nose and into the trachea (Fig. 29-1, B). A doctor inserts it using a lighted scope. Some RNs and respiratory therapists are trained to insert ET tubes. A cuff is inflated to keep the airway in place.
• Tracheostomy tube—inserted through a surgically created opening (stomy) into the trachea (tracheo) (Fig. 29-1, C). Cuffed tubes are common. The cuff is inflated to keep the tube in place. Doctors perform tracheostomies.
Vital signs are checked often. Observe for hypoxia and other signs and symptoms. If an airway comes out or is dislodged, tell the nurse at once. Frequent oral hygiene is needed. Follow the care plan.
Gagging and choking feelings are common. Imagine something in your mouth, nose, or throat. Comfort and reassure the person. Remind the person that the airway helps breathing. Use touch to show you care.
Persons with ET tubes cannot speak. Some tracheostomy tubes allow speech. Paper and pencils, Magic Slates, and communication boards are ways to communicate. Hand signals, nodding the head, and hand squeezes are common for simple “yes” and “no” questions. Follow the care plan. Always keep the signal light within reach.
Tracheostomies
A tracheostomy is a surgically created opening (stomy) into the trachea (tracheo). Tracheostomies are temporary or permanent for mechanical ventilation (p. 461). They are permanent when airway structures are surgically removed. Cancer, severe airway trauma, or brain damage may require a permanent tracheostomy.
A tracheostomy tube is made of plastic, silicone, or metal. It has three parts (Fig. 29-2):
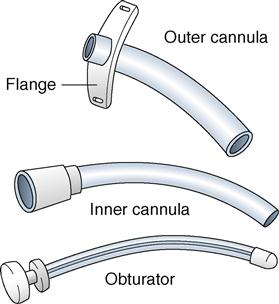
The cuffed tracheostomy tube provides a seal between the cannula and the trachea (see Fig. 29-1, C). This prevents air from leaking around the tube. It also prevents aspiration. A nurse or respiratory therapist inflates and deflates the cuff.
The tube must not come out (extubation). If not secure, it could come out with coughing or if pulled on. A loose tube moves up and down. It can damage the trachea. Call the nurse if the outer cannula comes out.
The tube must remain patent. If able, the person coughs up secretions. Otherwise suctioning is needed. Call for the nurse if you note signs and symptoms of hypoxia or respiratory distress.
Nothing must enter the stoma. Otherwise the person can aspirate. These safety measures are needed:
• Dressings do not have loose gauze or lint.
• The person is assisted with shampooing. Water must not enter the stoma.
• The stoma is covered when shaving.
• Swimming is not allowed. Water will enter the tube or stoma.
• Medical-alert jewelry is worn. The person carries a medical-alert ID card.
The nurse may ask you to assist with tracheostomy care. The care is done daily or every 8 to 12 hours. It also is done as needed for excess secretions, soiled ties or collar, or soiled or moist dressings. The care involves:
• Cleaning the stoma to prevent infection and skin breakdown.
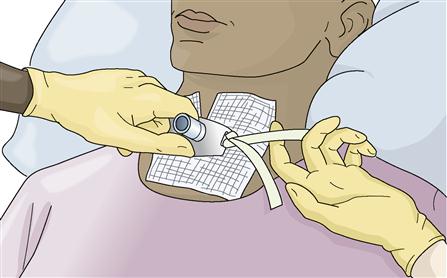
• Applying clean ties or a Velcro collar to prevent infection. Clean ties are applied before removing the dirty ones. Hold the outer cannula in place when the nurse changes the ties or collar. Continue to do so until the nurse secures the new ties or collar. The ties or collar must be secure but not tight. For an adult, a finger should slide under the ties or collar (Fig. 29-3).
See Promoting Safety and Comfort: Tracheostomies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree