Oxygen needs
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Describe the factors affecting oxygen needs.
• List the signs and symptoms of hypoxia and altered respiratory function.
• Describe the tests used to diagnose respiratory problems.
• Explain the measures that promote oxygenation.
• Describe the devices used to give oxygen.
• Explain how to safely assist with oxygen therapy.
• Perform the procedures described in this chapter.
Key terms
allergy A sensitivity to a substance that causes the body to react with signs and symptoms
apnea The lack or absence (a) of breathing (pnea)
Biot’s respirations Rapid and deep respirations followed by 10 to 30 seconds of apnea
bradypnea Slow (brady) breathing (pnea); respirations are fewer than 12 per minute
Cheyne-Stokes respirations Respirations gradually increase in rate and depth and then become shallow and slow; breathing may stop (apnea) for 10 to 20 seconds
cyanosis Bluish color to the skin, lips, mucous membranes, and nail beds
dyspnea Difficult, labored, or painful (dys) breathing (pnea)
hemoptysis Bloody (hemo) sputum (ptysis means to spit)
hyperventilation Respirations (ventilation) are rapid (hyper) and deeper than normal
hypoventilation Respirations (ventilation) are slow (hypo), shallow, and sometimes irregular
hypoxemia A reduced amount (hypo) of oxygen (ox) in the blood (emia)
hypoxia Cells do not have enough (hypo) oxygen (oxia)
Kussmaul respirations Very deep and rapid respirations
orthopnea Breathing (pnea) deeply and comfortably only when sitting (ortho)
orthopneic position Sitting up (ortho) and leaning over a table to breathe (pneic)
oxygen concentration The amount (percent) of hemoglobin containing oxygen
pollutant A harmful chemical or substance in the air or water
respiratory arrest When breathing stops
respiratory depression Slow, weak respirations at a rate of fewer than 12 per minute
sputum Mucus from the respiratory system that is expectorated (expelled) through the mouth
tachypnea Rapid (tachy) breathing (pnea); respirations are more than 20 per minute
KEY ABBREVIATIONS
| CO2 | Carbon dioxide |
| ID | Identification |
| L/min | Liters per minute |
| O2 | Oxygen |
| RBC | Red blood cell |
| SpO2 | Saturation of peripheral oxygen (pulse oximetry) |
Oxygen (O2) is a gas. It has no taste, odor, or color. It is a basic need required for life. Death occurs within minutes if breathing stops. Brain damage and serious illness can occur without enough oxygen. Illness, surgery, and injuries affect the amount of oxygen in the blood and cells.
You assist in the care of persons with oxygen needs. You must give safe and effective care.
Factors affecting oxygen needs
The respiratory and circulatory systems must function properly for cells to get enough oxygen. Any disease, injury, or surgery involving these systems affects the intake and use of oxygen. Body systems depend on each other. Altered function of any system (for example, the nervous, musculo-skeletal, or urinary system) affects oxygen needs. Oxygen needs are affected by:
• Fever. O2 needs increase. Respiratory rate and depth increase to meet the body’s needs.
• Nutrition. The body needs iron and vitamins (vitamin B12, vitamin C, and folate) to produce RBCs.
Altered respiratory function
Respiratory function involves three processes. Respiratory function is altered if even one process is affected.
• Air moves into and out of the lungs.
• O2 and CO2 are exchanged at the alveoli.
• The blood carries O2 to the cells and removes CO2 from them.
Hypoxia
Hypoxia means that cells do not have enough (hypo) oxygen (oxia). Without enough oxygen, cells cannot function properly. Anything affecting respiratory function can cause hypoxia. The brain is very sensitive to inadequate O2. Restlessness is an early sign. So are dizziness and disorientation. Report the signs and symptoms in Box 28-1 at once.
Hypoxia threatens life. All organs need oxygen to function. Oxygen is given. The cause of hypoxia is treated.
Abnormal respirations
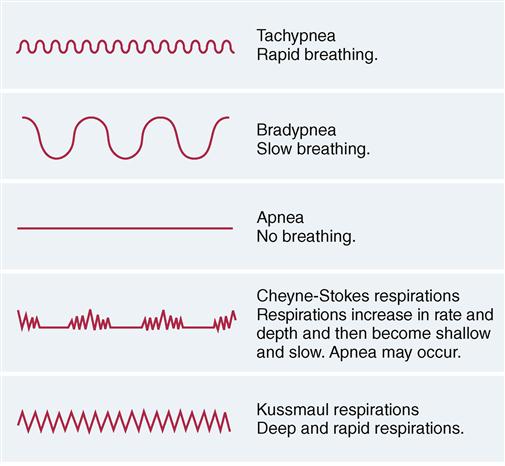
Normal adult respirations are 12 to 20 per minute. They are quiet, effortless, and regular. Both sides of the chest rise and fall equally. These breathing patterns are abnormal (Fig. 28-1):
Assisting with assessment and diagnostic tests
Altered respiratory function may be an acute or chronic problem. Report your observations promptly and accurately (Box 28-2). Quick action is needed to meet the person’s oxygen needs. Measures are taken to correct the problem and to prevent it from becoming worse.
See Focus on Communication: Assisting With Assessment and Diagnostic Tests.
The doctor orders tests to find the cause of the problem. These tests are commonly done in hospitals:
• Chest x-ray (CXR). An x-ray is taken of the chest to study lung changes.
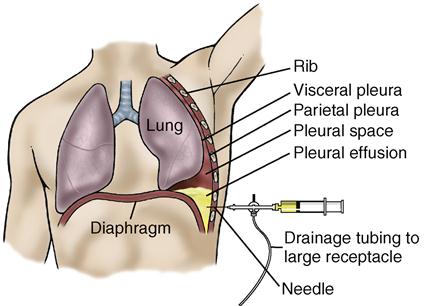
• Thoracentesis. The pleura (thora) is punctured. Air or fluid is removed (centesis) from it. The doctor inserts a needle through the chest wall into the pleural sac (Fig. 28-2, p. 446). Injury or disease can cause the sac to fill with air, blood, or fluid. Anti-cancer drugs can be injected into the pleural sac. The procedure takes a few minutes. Vital signs are taken. Then a local anesthetic is given. The person sits up and leans forward. He or she must not talk, cough, or move suddenly. Afterward a dressing is applied to the puncture site. Vital signs are taken. A chest x-ray is taken to detect lung damage. The person is observed for shortness of breath, dyspnea, cough, sputum, chest pain, cyanosis, vital sign changes, and other respiratory signs and symptoms.
• Pulmonary function tests. These measure the amount of air moving into and out of the lungs (volume). They also measure how much air the lungs can hold (capacity). The person takes as deep a breath as possible. Using a mouthpiece, the person blows into a machine (Fig. 28-3, p. 446). The tests help assess the risk for lung diseases or post-operative lung complications. They also measure the progress of lung disease and its treatment. Fatigue is common after the tests. The person needs to rest.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree