Urinary elimination
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Describe the rules for normal urinary elimination.
• Identify the observations to report to the nurse.
• Describe urinary incontinence and the care required.
• Describe straight, indwelling, and condom catheters.
• Explain why catheters are used.
• Explain how to care for persons with catheters.
• Describe two methods of bladder training.
• Perform the procedures described in this chapter.
Key terms
catheter A tube used to drain or inject fluid through a body opening
catheterization The process of inserting a catheter
dysuria Painful or difficult (dys) urination (uria)
Foley catheter See “indwelling catheter”
functional incontinence The person has bladder control but cannot use the toilet in time
hematuria Blood (hemat) in the urine (uria)
indwelling catheter A catheter left in the bladder so urine drains constantly into a drainage bag; retention or Foley catheter
mixed incontinence The combination of stress incontinence and urge incontinence
nocturia Frequent urination (uria) at night (noct)
oliguria Scant amount (olig) of urine (uria); less than 500 mL in 24 hours
overflow incontinence Small amounts of urine leak from a full bladder
polyuria Abnormally large amounts (poly) of urine (uria)
reflex incontinence Urine is lost at predictable intervals when the bladder is full
retention catheter See “indwelling catheter”
straight catheter A catheter that drains the bladder and then is removed
stress incontinence When urine leaks during exercise and certain movements that cause pressure on the bladder
transient incontinence Temporary or occasional incontinence that is reversed when the cause is treated
urge incontinence The loss of urine in response to a sudden, urgent need to void; the person cannot get to a toilet in time
urinary frequency Voiding at frequent intervals
urinary incontinence The involuntary loss or leakage of urine
urinary urgency The need to void at once
urination The process of emptying urine from the bladder; micturition or voiding
KEY ABBREVIATIONS
| C | Centigrade |
| CMS | Centers for Medicare & Medicaid Services |
| F | Fahrenheit |
| ID | Identification |
| IV | Intravenous |
| mL | Milliliter |
| OBRA | Omnibus Budget Reconciliation Act of 1987 |
| UTI | Urinary tract infection |
Eliminating waste is a physical need. The respiratory, digestive, integumentary, and urinary systems remove body wastes. The digestive system rids the body of solid wastes. The lungs remove carbon dioxide. Sweat contains water and other substances. Blood contains waste products from body cells burning food for energy. The urinary system removes waste products from the blood. It also maintains the body’s water balance.
Normal urination
The healthy adult produces about 1500 mL (milliliters) or 3 pints of urine a day. Many factors affect urine production. They include age, disease, the amount and kinds of fluid ingested, dietary salt, body temperature, perspiration, and drugs. Some substances increase urine production—coffee, tea, alcohol, and some drugs. A diet high in salt causes the body to retain water. When water is retained, less urine is produced.
Urination, micturition, and voiding mean the process of emptying urine from the bladder. The amount of fluid intake, habits, and available toilet facilities affect frequency. So do activity, work, and illness. People usually void at bedtime, after sleep, and before meals. Some people void every 2 to 3 hours. The need to void at night disturbs sleep.
Some persons need help getting to the bathroom. Others use bedpans, urinals, or commodes. Follow the rules in Box 22-1 and the person’s care plan.
See Focus on Communication: Normal Urination.
See Teamwork and Time Management: Normal Urination.
Observations
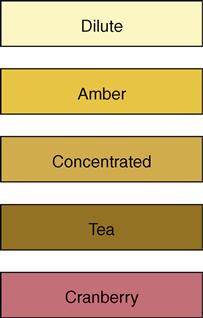
Normal urine is pale yellow, straw-colored, or amber (Fig. 22-1). It is clear with no particles. A faint odor is normal. Observe urine for color, clarity, odor, amount, and particles.
Some foods affect urine color. Red food dyes, beets, blackberries, and rhubarb cause red-colored urine. Carrots and sweet potatoes cause bright yellow urine. Certain drugs change urine color. Asparagus causes a urine odor.
Ask the nurse to observe urine that looks or smells abnormal. Report complaints of urgency, burning on urination, or painful or difficult urination. Also report the problems in Table 22-1. The nurse uses the information for the nursing process.
Table 22-1
| Problem | Definition | Causes |
| Dysuria | Painful or difficult (dys) urination (uria) | Urinary tract infection (UTI), trauma, urinary tract obstruction |
| Hematuria | Blood (hemat) in the urine (uria) | Kidney disease, UTI, trauma |
| Nocturia | Frequent urination (uria) at night (noct) | Excess fluid intake, kidney disease, prostate disease |
| Oliguria | Scant amount (olig) of urine (uria); less than 500 mL in 24 hours | Poor fluid intake, shock, burns, kidney disease, heart failure |
| Polyuria | Abnormally large amounts (poly) of urine (uria) | Drugs, excess fluid intake, diabetes, hormone imbalance |
| Urinary frequency | Voiding at frequent intervals | Excess fluid intake, UTI, pressure on the bladder, drugs |
| Urinary incontinence | The involuntary loss or leakage of urine | Trauma, disease, UTI, reproductive or urinary tract surgeries, aging, fecal impaction, constipation, not getting to the bathroom in time |
| Urinary urgency | The need to void at once | UTI, fear of incontinence, full bladder, stress |
 Bedpans
Bedpans
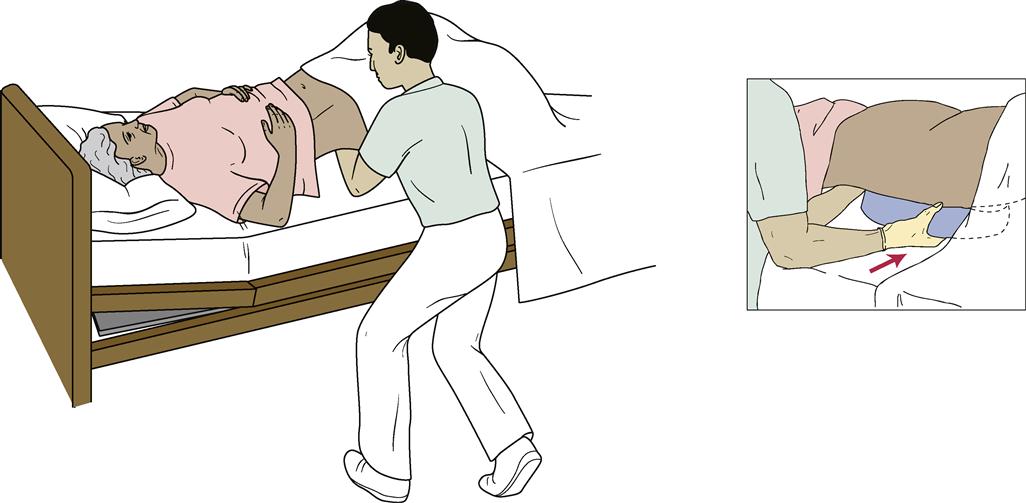
Bedpans are used by persons who cannot be out of bed. Women use bedpans for voiding and bowel movements. Men use them for bowel movements.