Barbara Lauritsen Christensen
Care of the patient with cancer
Objectives
1. Discuss the incidence of cancer as one of the leading causes of death in the United States.
2. Compare the three most common sites for cancer in men and women.
3. Discuss development, prevention, and detection of cancer.
4. List seven risk factors for the development of cancer.
6. State seven warning signs of cancer.
7. Explain common reasons for delay in seeking medical care when a diagnosis of cancer is suspected.
10. Describe the process of metastasis.
11. Define the systems of tumor classification: grading and staging.
12. List common diagnostic tests used to identify cancer.
13. Explain why biopsy is essential in confirming a diagnosis of cancer.
15. Describe the major categories of chemotherapeutic agents.
17. Discuss six general pain relief guidelines for the patient with advanced cancer.
Key terms
alopecia ( l-
l- -P
-P -sh
-sh –
– , p. 796)
, p. 796)
autologous (aw-T L-
L- -g
-g s, p. 800)
s, p. 800)
carcinogen (k r-S
r-S N-
N- -j
-j n, p. 780)
n, p. 780)
carcinogenesis (k r-s
r-s n-
n- -J
-J N-
N- -s
-s s, p. 780)
s, p. 780)
carcinoma (k r-s
r-s -N
-N -m
-m , p. 785)
, p. 785)
differentiated (d f-
f- r-
r- N-sh
N-sh –
– -t
-t d, p. 786)
d, p. 786)
immunosurveillance ( m-
m- -n
-n -s
-s r-V
r-V -l
-l ns, p. 785)
ns, p. 785)
leukopenia (l -k
-k -P
-P -n
-n –
– , p. 791)
, p. 791)
malignant (m -L
-L G-n
G-n nt, p. 785)
nt, p. 785)
metastasis (m -T
-T S-t
S-t -s
-s s, p. 785)
s, p. 785)
Papanicolaou’s test (smear) (p -p
-p -N
-N -k
-k -l
-l z t
z t st, sm
st, sm r, p. 786)
r, p. 786)
stomatitis (st -m
-m -T
-T -t
-t s, p. 796)
s, p. 796)
thrombocytopenia (thr m-b
m-b -s
-s t-
t- -P
-P -n
-n –
– , p. 796)
, p. 796)
tumor lysis syndrome (T-m r L
r L -s
-s s S
s S N-dr
N-dr m, p. 799)
m, p. 799)
Oncology
Oncology is the sum of knowledge about tumors; it is the branch of medicine concerning the study of tumors. Oncology nursing is the care of people with cancer.
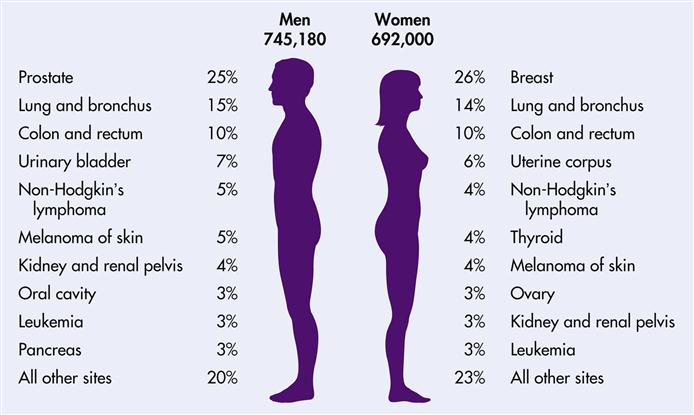
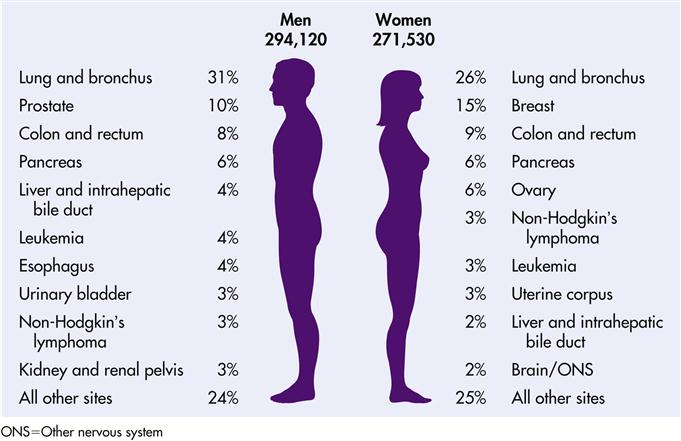
Until the appearance of acquired immunodeficiency syndrome (AIDS), probably no other medical diagnosis produced as much fear as a diagnosis of cancer. Cancer is feared far more than heart disease. The word cancer is viewed as synonymous with death, pain, and disfigurement. However, attitudes toward cancer have not kept pace with advances in the treatment and control of cancer. Education of health care professionals and the public is essential to promote more positive and realistic attitudes about cancer and cancer treatment (Lewis et al., 2007). The American Cancer Society (ACS) indicates that in the United States men have a 1 in 2 lifetime risk of developing cancer; for women, the risk is 1 in 3. The leading cancer sites for the male are prostate, lung, colon, and rectum. The leading cancer sites for the female are breast, lung, colon, and rectum (ACS, 2008a). Of every five deaths in the United States, one is from cancer, making it the second leading cause of death (heart disease is the most common).
Cancer is not one disease, but a group of more than 200 diseases characterized by the uncontrolled and unregulated growth and spread of abnormal cells. Early detection and prompt treatment can cure some cancers and slow the progression of others. If not detected and controlled, cancer can result in death. Overall, it affects people of all ages, but most cases (76%) are diagnosed in those over the age of 55 (see Life Span Considerations box). Cancer incidence is higher in blacks than in whites and other minority groups (see Cultural Considerations box). An estimated 30% of Americans now living will experience cancer at some point in their lives. In 2006, 564,830 Americans died from cancer, which is more than 1500 persons per day (ACS, Cancer facts and figures, 2009). The death rate from all cancers combined has decreased by 2.6% per year among men and by 1.8% per year among women since 2002. Cancer death rates have been decreasing since 1991 in men and since 1992 in women. Compared to the peak rates in 1990 for men and 1991 for women, the cancer death rate for all sites combined in 2004 was 18.4% lower in men and 10.5% lower in women (ACS, 2009). The 5-year survival rate is now 65%.
Lung cancer is the leading cause of cancer-related death in both men and women. Other cancers, such as breast and prostate, occur more often than lung cancer, but they have better cure and survival rates because of early detection and treatment (Figures 17-1 and 17-2).
Development, prevention, and detection of cancer
Carcinogenesis is the process by which normal cells are transformed into cancer cells. Although numerous theories have been proposed to explain it, no single cause has been accepted. The exact cause of most human cancers is still unknown, but most types are likely to have multiple causes. It is not known how many tumors have a chemical, environmental, genetic, immunologic, or viral origin. Cancers may arise spontaneously from causes that are thus far unexplained.
Primary prevention of cancer consists of changes in lifestyle habits to eliminate or reduce exposure to carcinogens, substances known to increase the risk for developing cancer. Risk factors include the following:
• Dietary habits: When it comes to preventing cancer, is diet really important? Experts believe that it is. An estimated one third of cancer deaths are attributable to nutritional factors such as high-fat, low-fiber diets (ACS, Cancer facts and figures, 2009). The National Cancer Institute (NCI) estimates that dietary modifications could prevent as many as one third of all cancer deaths in the United States. Obesity is a risk factor for breast, prostate, gallbladder, ovarian, and uterine cancer (National Cancer Institute, 2004). Diet also plays a role in the development of colon, rectal, and breast cancer. The NCI has launched a program called “5 a Day for Better Health” to show how easy it is to add at least five servings of fruits and vegetables to the daily diet as a way of reducing the risks of cancer (see Health Promotion box). Fruit and vegetable consumption may protect against cancers of the mouth and pharynx, esophagus, lung, stomach, and colon and rectum. However, consumption has seen little improvement since the mid-1990s. Less than one in four adults was eating the recommended servings in 2005 (ACS, 2009). At present only 20% of the U.S. population consumes five daily servings of fruits and vegetables.
Hereditary cancers
About 90% of cancers are not inherited. Hereditary cancers arise from germline mutations. They are diagnosed usually 15 to 20 years earlier than cancers that are not inherited. Often, several relatives have the same or related cancers. They are more likely to be bilateral, and the same person may have multiple cancers. These multiple cancers are often seen in unusual organ combinations, such as breast and sarcoma, breast and thyroid, leukemia and brain tumors. Hereditary cancers are characterized by precursor lesions, such as polyps in colorectal cancer and dysplastic nevi in melanoma (Lewis et al., 2007).
Genetic susceptibility
For many years scientists have searched for genetic patterns in the most common cancer sites. Only 10% of cancers have an etiology of a strong genetic link (Tannock et al., 2005). The following patterns have emerged:
Cancer risk assessment and genetic counseling
When an individual or family is suspected of having a mutation in a cancer-causing gene, a cancer risk assessment is performed. This is the first step toward identifying hereditary cancer predisposition. The assessment begins with a comprehensive family history, included information on first-, second-, and third-degree relatives. Next obtain medical records to confirm the cancer diagnoses identified in the family history. The records usually requested include pathology reports, autopsy reports, death certificates, and discharge summaries from hospitalizations. Confirmation of cancer diagnoses through medical record analysis provides the patient with the most accurate risk analysis possible.
Genetic counseling is an essential component of the genetic evaluation. It is comprehensive and includes obtaining informed consent and proving education, health promotion, and support to individuals and families facing the uncertainty of hereditary cancer and cancer syndromes.
Cancer prevention and early detection
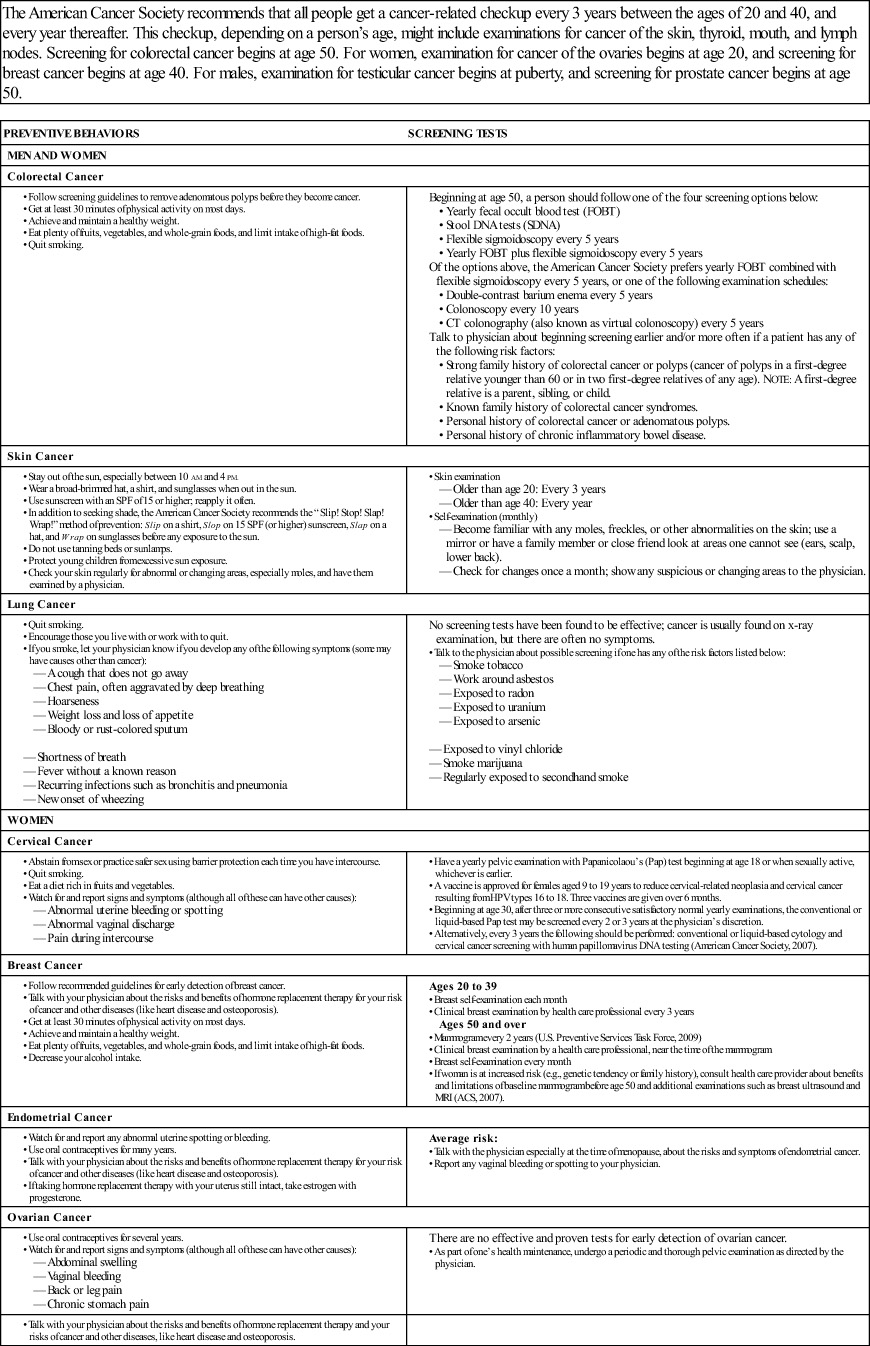
Prevention and early detection of cancer includes recognition of cancer’s warning signals (Box 17-1). The American Cancer Society advises specific preventive behaviors and screening tests for men and women (Table 17-1). The nurse plays a prominent role in prevention and detection of cancer. Early detection and prompt treatment are directly responsible for increased survival rates in patients with cancer (see Health Promotion box). It is reported that 65% of patients who are diagnosed with cancer today will be alive 5 years after diagnosis.
Beginning in high school, all women should be taught to perform breast self-examination (BSE) each month, 2 or 3 days after the menstrual period ends. After menopause, a woman should choose a specific day to help her remember, such as the first day of each month. A woman needs to become familiar with the appearance and feel of her breasts. This will help her identify any change from one month to the next. Any abnormality—such as discharge from the nipples; puckering, dimpling, peau d’orange (skin appearance of an orange peel, or scaling of the skin; and the palpation of a lump or thickness)—is significant. (See Chapter 12 for instructions on BSE.) Teach BSE to all patients (men and women), emphasizing that any identifiable problem should be brought to the attention of a physician. Any delay is a waste of valuable time if cancer is present.
Teach males, beginning at puberty, to check the scrotum for enlargement, thickening, or the presence of a lump in the testicles. This should be done monthly, after a warm bath or shower. Emphasize that a physician must be contacted to determine the significance of any changes from the normal, smooth consistency of the testes (see Chapter 12). Some symptoms of testicular cancer include a lump in or enlargement of either testicle, a heavy feeling in the scrotum, dull aching in either the groin or the lower abdomen, fluid collection in the scrotum, and tenderness or enlargement of the breasts (this results from hormones produced by cancer cells) (National Cancer Institute, 2007).
Advise men over age 50 to have a prostate-specific antigen (PSA) test and rectal examination once a year. Symptoms of blood in the urine, difficulty starting to urinate, a weak flow of urine, or other urination problems should be reported to the physician.
A common reason for delay in diagnosing cancer is that early malignant changes do not produce pain. Cancer may be insidious at the onset, and it may be far advanced before the individual has any symptoms.
Pathophysiology of cancer
Cell mechanisms and growth
The basic unit of structure and function in all living things is the cell. The adult human body contains approximately 60,000 billion cells. Although there are many different types of cells, all of them have certain common characteristics. For example, all cells need nourishment to maintain life, and all cells use almost identical nutrients. All cells use oxygen, which combines with fat, protein, or carbohydrates to release the energy needed for cells to function. The mechanisms for changing nutrients into energy are generally the same in all cells, and all cells deliver their end product of chemical reactions into the nearby fluids.
Most cells are able to reproduce. When cells are destroyed, the remaining cells of the same type reproduce until the correct number has been replenished. This orderly replacement of cells is governed by a control mechanism that stops when the loss or damage has been corrected. Dynamic, active, and orderly, the healthy cell is a small powerhouse, laboratory, factory, and duplicating machine, perfectly copying itself over and over. Our immune system helps us from developing cancer by destroying the abnormal cells. Occasionally our immune system fails to recognize these abnormal cells and cancer develops.
Cancer cells are not subject to the usual restrictions placed on cell proliferation by the host. When malignant cells change, they become unlike parent cells; they are not differentiated, or recognizable as being the same in size or shape as normal cells. Cancer cells can divide and multiply, but not in a normal manner. Instead of limiting their growth to meet specific needs of the body, they continue to reproduce in a disorderly and unrestricted manner. The cellular features of cancer cells are a local increase in the number of cells, loss of normal cellular arrangement, variation in cell shape and size, increased nuclear size, increased miotic activity, and abnormal mitosis and chromosomes.
Proliferation is not always indicative of cancer, however. Abnormal cellular growth is classified as nonneoplastic growth and neoplastic growth. The four common nonneoplastic growth patterns are hypertrophy, hyperplasia, metaplasia, and dysplasia. Though not neoplastic conditions, these may precede the development of cancer. Anaplasia means “without form” and is an irreversible change in which the structures of adult cells regress to more primitive levels.
Neoplasm is the term for uncontrolled or abnormal growth of cells. Neoplasms may be benign (not recurrent or progressive; nonmalignant) or malignant (growing worse and resisting treatment, as in cancerous growths [Table 17-2]). The growths are also called tumors, which means swelling or enlargement. They may be localized or invasive. Benign tumors may become serious because their increased size damages surrounding tissues, as in a benign brain tumor. Malignant neoplasms may progress and destroy surrounding tissues. They may also metastasize from the primary site of origin to distant sites.
Table 17-2
General Characteristics of Neoplasms
| BENIGN TUMORS | MALIGNANT TUMORS |
| Slow, steady growth | Rate of growth varies—usually rapid |
| Remains localized | Metastasizes |
| Usually contained within a capsule | Rarely contained within a capsule |
| Smooth, well defined; movable when palpated | Irregular; more immobile when palpated |
| Resembles parent tissue | Little resemblance to parent tissue |
| Crowds normal tissue | Invades normal tissue |
| Rarely recurs after removal | May recur after removal |
| Rarely fatal | Fatal without treatment |
Metastasis is the process by which tumor cells spread from the primary site to a secondary site. Once cancer cells have moved to another area of the body, secondary tumors may grow in that area. Metastasis can occur by (1) direct spread of tumor cells by diffusion to other body cavities or (2) circulation by way of blood and lymphatic channels.
In addition to the identified carcinogenic factors that may cause malignant cellular changes, certain viruses have been suspected. There is also evidence to suggest that certain genetic factors result in a predisposition to the development of cancer.
The body’s immune system is responsible for recognizing and destroying malignant cells. The immune system may be weakened by cancer-producing substances, tumor cells, and the aging process. Some T cells are responsible for immunosurveillance (the immune system’s recognition and destruction of newly developed abnormal cells). When a cell becomes malignant, it carries a tumor-specific antigen on its membranes that is recognized by the body as nonself and destroyed. If T-cell function is suppressed by age, drugs (e.g., corticosteroids), poor nutrition, alcohol, serious infections, or certain disease processes (e.g., neoplastic invasion of bone and lymph tissue), the risk of cancer increases. To suppress T-cell rejection of a transplanted organ, steroids and other drugs are given. The resultant loss of immunosurveillance increases the risk of certain cancers.
Description, grading, and staging of tumors
Cancers are described according to the original site of the primary tumor. Carcinoma is the term used for malignant tumors composed of epithelial cells, which tend to metastasize. Carcinomas originate from embryonal ectoderm (skin and glands) and endoderm (mucous membrane linings of the respiratory tract, gastrointestinal [GI] tract, and genitourinary tract). Sarcoma refers to malignant tumors of connective tissues; they originate from embryonal mesoderm, such as muscle, bone, or fat, usually manifesting as a painless swelling. Sarcoma may affect bone, bladder, kidneys, liver, lungs, parotids, and spleen. Lymphomas and leukemias originate from the hematopoietic system.
A tumor may be named for its location, its cellular makeup, or the person by whom it was identified.
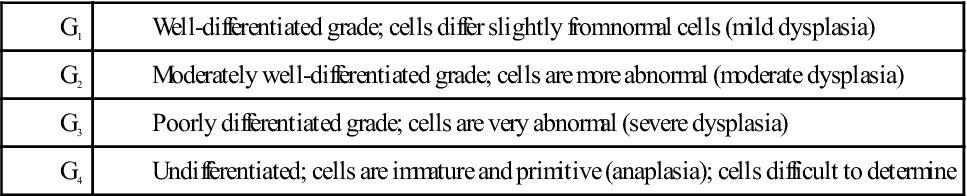
Grading of tumors
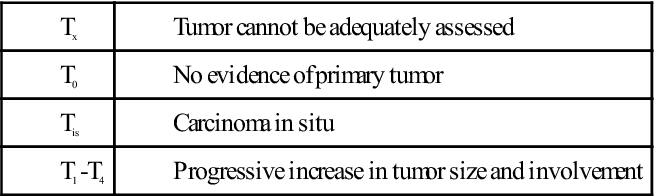
Tumors are classified grade 1 to grade 4 by the degree of malignancy. Grade 1 is the most differentiated (most like the parent tissue) tumor and the least malignant. Grade 4 is the least differentiated (unlike parent tissue) tumor and the most malignant (Box 17-2).
Extent of disease classification
Classifying the extent and spread of disease is termed staging. This classification system is based on a description of the extent of the disease rather than on cell appearance. Although staging for different types of cancer has similarities, there are many differences, based on a thorough knowledge of the natural history of each specific type of cancer.
Clinical staging
The clinical staging classification system determines the extent of the disease process of cancer by stages:
| Stage 0: | Cancer in situ |
| Stage I: | Tumor limited to the tissue of origin; localized tumor growth |
| Stage II: | Limited local spread |
| Stage III: | Extensive local and regional spread |
| Stage IV: | Metastasis |
TNM classification system
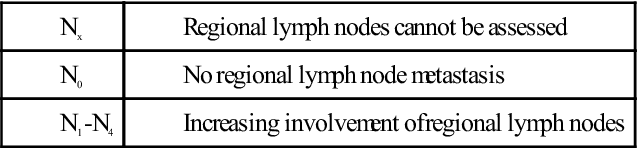
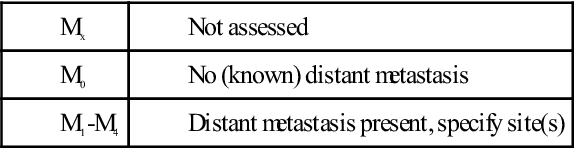
The TNM classification system represents the standardization of the clinical staging of cancer. This classification system is used to determine the extent of the disease process of cancer according to three parameters: tumor size (T), degree of regional spread to the lymph nodes (N), and metastasis (M) (see Box 17-2). This system is used to direct treatment, predict prognosis, and contribute to cancer research by ensuring reliable comparison of different patients.
Bethesda system
Exfoliative (pertaining to the shedding of something) cytology (e.g., Papanicolaou’s test [smear] [Pap]) is a means of studying cells that the body has shed during the normal sequence of growth and replacement of body tissues. If cancer is present, cancer cells are also shed. The method is most commonly used to detect cancers of the cervix, but it may be used for tissue specimens from any organ.
The results of the Pap test, as given by the Bethesda system (the preferred system), are as follows:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 -N
-N N,
N,  –
– p-s
p-s ,
,  -K
-K K-s
K-s –
– ,
,  –
– -pl
-pl zm,
zm,  n-K
n-K L-
L- -j
-j ,
,  L-
L- –
– -t
-t v,
v,  r-K
r-K -m
-m ,
,