Craig E. Nielsen
Care of the patient with HIV/AIDS
Objectives
1. Describe the agent that causes HIV disease.
3. Explain the differences between HIV infection, HIV disease, and AIDS.
4. Describe the progression of HIV infection.
5. Discuss how HIV is and is not transmitted.
6. Describe patients who are at risk for HIV infection.
7. Discuss the pathophysiology of HIV disease.
8. List signs and symptoms that may be indicative of HIV disease.
9. Discuss the laboratory and diagnostic tests related to HIV disease.
10. Discuss the issues related to HIV antibody testing.
11. Describe the multidisciplinary approach in caring for a patient with HIV disease.
12. List opportunistic infections associated with advanced HIV disease (AIDS).
14. Implement a care plan for the patient with AIDS.
15. Discuss the importance of adherence to HIV treatment.
16. Discuss the use of effective prevention messages in counseling patients.
17. Define the nurse’s role in the prevention of HIV infection.
Key terms
acquired immunodeficiency syndrome (AIDS) ( m-
m- -n
-n -d
-d -F
-F SH-
SH- n-s
n-s , p. 744)
, p. 744)
CD4+ lymphocyte (L M-f
M-f -s
-s t, p. 742)
t, p. 742)
Centers for Disease Control and Prevention (CDC) (p. 734)
enzyme-linked immunosorbent assay (ELISA) ( m-
m- -n
-n -Z
-Z R-b
R-b nt, p. 747)
nt, p. 747)
human immunodeficiency virus (HIV) (p. 734)
Kaposi’s sarcoma (k -P
-P S-s
S-s z s
z s r-K
r-K -m
-m , p. 734)
, p. 734)
opportunistic ( p-p
p-p r-t
r-t -N
-N S-t
S-t k, p. 736)
k, p. 736)
phagocyte (f g-
g- -S
-S T-
T- k, p. 744)
k, p. 744)
Pneumocystis jiroveci (formerly carinii ) pneumonia (PCP) (n -m
-m -S
-S S-t
S-t s k
s k -R
-R N-
N- , p. 734)
, p. 734)
retrovirus (r -tr
-tr -V
-V -r
-r s, p. 742)
s, p. 742)
seroconversion (s r-
r- -k
-k n-V
n-V R-zh
R-zh n, p. 740)
n, p. 740)
seronegative (s r-
r- -N
-N G-
G- -t
-t v, p. 747)
v, p. 747)
vertical transmission (p. 739)
Nursing and the history of HIV disease
As early as 1979, physicians in New York and California were noting cases of Pneumocystis jiroveci (formerly carinii) pneumonia (PCP), an unusual pulmonary disease caused by a fungus and primarily associated with people who have suppressed immune systems. These physicians also noted an increase in the number of people with Kaposi’s sarcoma, a rare cancer of the skin and mucous membranes characterized by blue, red, or purple raised lesions seen mainly in Mediterranean men. The interesting thing was that these two diseases were occurring at alarming rates in clusters of young homosexual men whose immune systems were failing. Researchers at the Centers for Disease Control and Prevention (CDC), a division of the U.S. Public Health Service in Atlanta that investigates and controls various diseases, soon learned that this immune disorder was also affecting injecting drug users and hemophiliacs. They later learned that it also affected heterosexual men and women.
The origins of human immunodeficiency virus (HIV) remain somewhat obscure, and why HIV gave rise to the acquired immunodeficiency syndrome (AIDS) pandemic only in the twentieth century has not yet been determined. The earliest case of HIV infection has been dated to 1959. It was identified in the Democratic Republic of Congo by using different methods of molecular clock analysis. It has also been estimated that HIV began to radiate from its source around the 1930s (Buonaguro et al., 2007). The escalating pandemic likely resulted from the combination of significant cultural and sociobehavioral changes, the use of nonsterile needles for parenteral injections and vaccinations, and the unintended contamination of products used for medical treatments.
HIV/AIDS has been recognized as a clinical syndrome since the early 1980s. But several researchers have identified patients who might have fit the CDC’s Case Surveillance definition before this time. For example, the unusual and rapid death of a 15 year-old black boy from aggressive disseminated Kaposi’s sarcoma suggests he might be the first confirmed case of HIV infection in the United States (Garry et al., 1988). This patient from St. Louis had no international travel experience, which suggests that other individuals were HIV infected as well. This also suggests that HIV has existed in some form in the United States since at least the 1960s.
HIV is known as zoonotic, an organism that has been able to cross from an animal species to humans. A similar virus was noted in primates (called simian immunodeficiency virus) and likely crossed into humans with the hunting and consumption of these animals in Africa. Other examples of zoonotic transmission include severe acute respiratory distress syndrome, anthrax, and Hantavirus and West Nile virus (World Health Organization [WHO], 2009). HIV began to spread in the middle to late 1970s, but because of the long incubation period, in most countries the viral epidemic progressed undetected. When the virus began causing widespread disease in the 1980s, it provoked fear among laypeople and health care providers alike. It was also an exciting time for health care workers because they knew they were seeing a new pathogen with a route of transmission not completely understood. In spite of the stigmas and fears that emerged (which still exist to some extent today), nurses were at the forefront providing care. Nurses met the challenges of providing and coordinating services, organizing community-based organizations, teaching about prevention, and helping patients deal with a terminal disease.
In June 1981, the CDC published a notation about some patients with signs and symptoms that later would be attributed to AIDS (CDC, 1981). The signs and symptoms listed were related to the development of opportunistic infections (OIs). Since that time, AIDS has become known as one of the most challenging infectious diseases of the twentieth and twenty-first centuries. In 1982, the CDC stated that blood and other body fluids may transmit the disease, and they issued a statement about using precautions with other people’s body fluids.
In 1983 French researchers isolated the virus believed to be responsible for AIDS, and they called it lymphadenopathy-associated virus (Barré-Sinoussi et al., 1983). One year later an American scientist claimed the discovery of the etiologic agent and named it the human T-cell lymphotropic virus type III (Gallo et al., 1984). Other researchers discovered viruses that appeared to be the same or close members of the same family. In 1986 the International Committee on Taxonomy of Viruses renamed the virus, calling it the human immunodeficiency virus (HIV). In that same year a second and distinctly different strain of the virus was discovered in West Africa. Researchers believed that this strain may have been present in West Africa for many years. The scientific names assigned to distinguish the two viruses are HIV-1 and HIV-2.
The discovery of a second HIV strain was both major and alarming, since it was the first clue that HIV could change its appearance and mutate rapidly. This capability for rapid mutation, often referred to as genetic promiscuity, has become the trademark of this virus. It represents an immense challenge for scientists as they search for treatment and vaccine strategies. HIV-1 is found worldwide and is the prevalent strain in most places, including the United States, Europe, and Central Africa. HIV-1 and HIV-2 are both spread in the same ways and have similar signs and symptoms. Both of these viral strains also result in OIs. Whereas most HIV-1 infected people develop profound immunodeficiency and high viral loads, resulting in death, most HIV-2 infected people act as long-term nonprogressors (Rowland-Jones & Whittle, 2007). Patients diagnosed with HIV-2 tend to be less infectious during the initial stage of the infection than those diagnosed with HIV-1. As the HIV-2 infection progresses, the patient’s ability to infect other people increases. The prevalence rate of HIV-2 is higher in parts of Africa and in the countries surrounding Africa. This is thought to be related to commercial trading relationships and immigration. There are increased reports of cases in the United States of HIV-2, mainly in refugees and immigrants from countries with HIV-2.
HIV-1 is much more virulent (toxic) than HIV-2. People diagnosed with HIV-2 tend to have a normal life span when compared with their uninfected population cohort. Also, in contrast to HIV-1, HIV-2 does not result in higher mortality risks in patients between the ages of 55 and 80 years old (Rowland-Jones & Whittle, 2007). Patients infected with HIV-2 develop problems with immunodeficiency more slowly. However, HIV-2 patients who are malnourished, without adequate access to health care, and without clean water have an increased mortality risk when compared with a healthier HIV-2 infected patient.
Since the first cases of AIDS were reported in 1981, the CDC has revised the case definition three times in response to improved laboratory and diagnostic methods (CD4+ and viral test results), additional clinical conditions, increased knowledge of the natural history of HIV disease, and improved clinical management (CDC, 2006). The current definition (Table 16-1), used by all states and U.S. territories, allows the disease to be consistently monitored for public health purposes. Because HIV selectively infects and destroys cells that display CD4+ molecules on their surface (primarily lymphocytes), the new definition includes all HIV-infected people who have CD4+ counts of 200 cells/mm3 or fewer (as opposed to the normal 600 to 1200 cells/mm3). These revisions to the AIDS surveillance case definition took into account the advances in diagnostic methods and treatment to provide more accurate information on the numbers of life-threatening opportunistic (caused by normally nonpathogenic organisms in a host whose resistance has been decreased by such disorders as HIV disease) illnesses and deaths among HIV-infected individuals.
Table 16-1
| 1993 CLASSIFICATION SYSTEM FOR HIV INFECTION IN ADOLESCENTS AND ADULTS | |||
| CLINICAL CATEGORIES | |||
| CD4+ CELL CATEGORIES* | A: ASYMPTOMATIC, PGL, ACUTE HIV INFECTION | B: SYMPTOMATIC, NOT (A) OR (C) CONDITIONS | C: AIDS-INDICATOR CONDITIONS |
1. ≥500/mm3 | A1 | B1 | C1 |
2. 200-499/mm3 | A2 | B2 | C2 |
3. <200/mm3 | A3 | B3 | C3 |
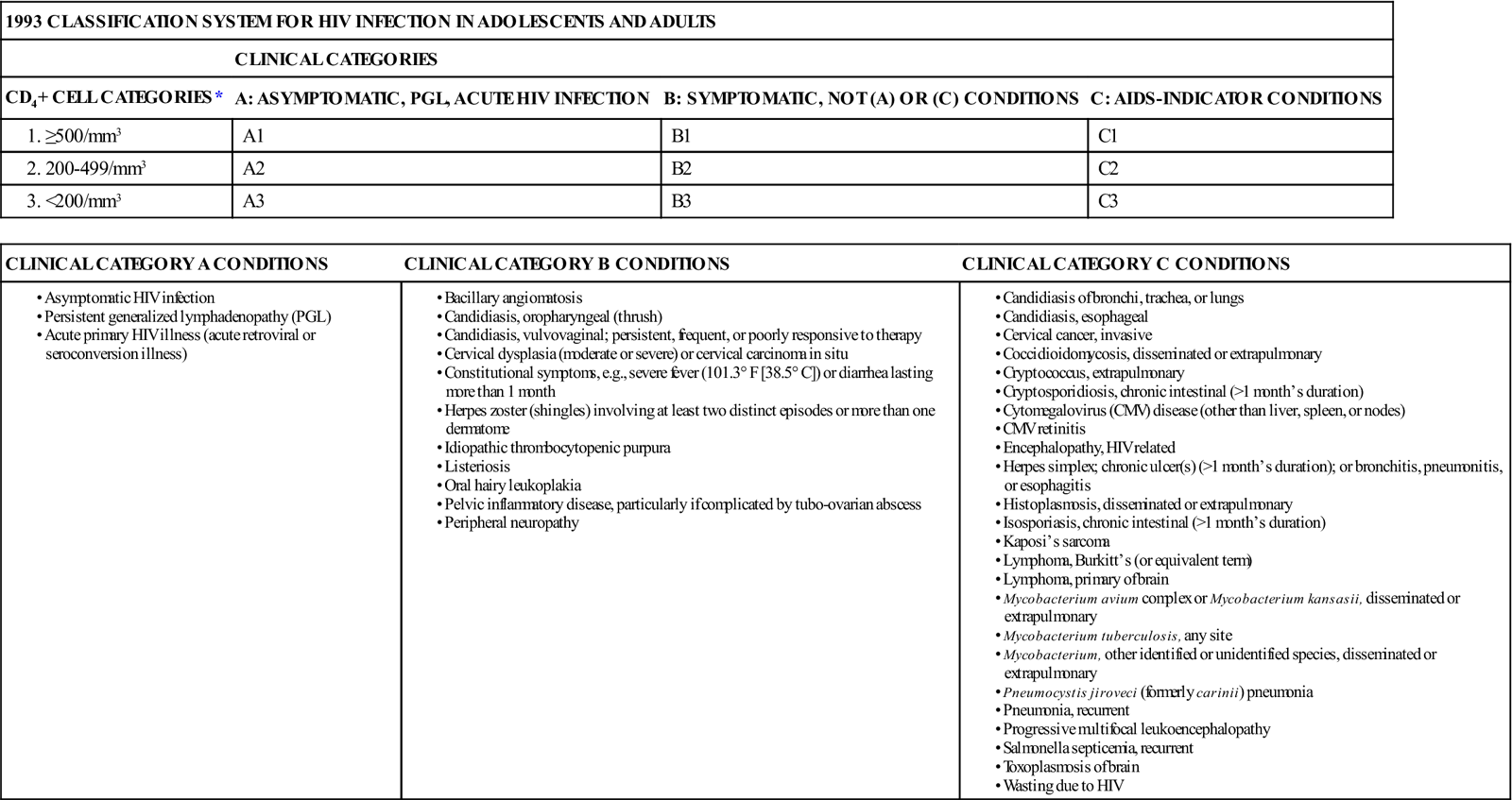
*According to the lowest, most accurate count, not the most recent count.
It was not until 1987, after the CDC reported three cases of occupationally acquired HIV infection in health care providers, that guidelines called universal blood and body fluid precautions, or standard precautions, were developed for the prevention of occupational exposure. This forever changed the way health care personnel protect themselves and others from the spread of bloodborne pathogens. That same year, the Association of Nurses in AIDS Care was established to address the needs of individuals with HIV disease and to provide a professional forum for nurses, who often faced discrimination for providing care to HIV-infected patients.
By now, a broad spectrum of individuals, including children and adults and people from all socioeconomic groups, is affected by this disorder (see Life Span Considerations box). Nurses have been instrumental in establishing education and treatment standards, in collaboration with community-based organizations. Today, nurses comprise the largest group of health care providers who care for individuals with HIV disease, stressing the importance of prevention and influencing policymakers. HIV nursing has imparted lessons that can be useful in other patient populations as well: the importance of patient education, adherence to medical regimens, prevention, and health-promoting behaviors.
Significance of the problem
Disease burden
Throughout the world, HIV is one of the leading causes of death and results in more deaths than any other disease caused by infection. As of 2007, approximately 33.2 million people were infected with HIV. Approximately 2.5 million living with this infection were children, and 2.5 million new diagnoses were made that year—7400 new cases each day. More than 2 million people die every year due to AIDS. Almost all of those people living with HIV reside in countries with low or middle incomes.
Sub-Saharan Africa has been hit especially hard (WHO, 2008). This region contains more than 65% of the world’s HIV population and accounts for 76% of the total mortality rate attributed to AIDS (Henry J. Kaiser Family Foundation, 2007). It is estimated that by the year 2010, 18 million children in that region will lose both of their parents to AIDS. Death related to AIDS is largely associated with poor health care access for prevention and treatment services (Henry J. Kaiser Family Foundation, 2007). During the past 2 years the number of people infected with HIV has declined. This decreasing infection rate is thought to be related to increased access to antiretroviral treatments. Managing and treating this disease will remain a challenge for years to come, especially in the sub-Saharan region of Africa.
In the United States approximately 56,000 new cases of HIV are diagnosed each year (Hall et al., 2008). More than 1 million people in the United States are currently living with HIV/AIDS (Henry J. Kaiser Family Foundation, 2007). Between 2003 and 2006, the number of new HIV/AIDS cases in the United States stabilized, while the number of people who were living with the disease increased. At the end of 2006, almost 500,000 people were infected and living with HIV/AIDS (CDC, 2008). California, Florida, and New York accounted for most of the patients with AIDS diagnoses (CDC, 2008).
Trends and most affected populations
Beginning in 1996 the use of highly active antiretroviral therapy (HAART) greatly increased among persons with HIV infection in the United States. Since that time, fewer people have developed AIDS (CDC, 2009a). New HIV and AIDS cases affect varied racial groups, ethnic groups, geographic areas, and demographic populations. This epidemic has affected nonwhite people, women, heterosexuals, and intravenous drug users. However, people with HIV are living longer (CDC, 2008).
Men who have sex with other men (MSM) comprise the biggest proportion of HIV/AIDS patients, accounting for 71% of the total number of HIV infections in adult and adolescent males (CDC, 2007). The HIV infection rates of MSM decreased from 71% in 1983 to 44% in 1996. A prediction was made that this rate would continue to decrease to approximately 25% (Holmberg, 1996). Instead of decreasing, however, new HIV infections for MSM have stayed about the same. Despite media campaigns to educate MSM about high-risk behaviors, many believe that HIV is now a chronic and treatable disease, and this has led to an increase in high-risk sexual behaviors (Holmberg, 1996).
During the first 25 years of this epidemic, the distribution of new cases based on ethnicity and race changed (see Cultural Considerations box). Hispanics and blacks have been disproportionately infected with HIV. In 2006, although blacks made up only 13% of the population in the United States, they accounted for almost half of the total number of HIV/AIDS cases that were diagnosed. Black adults and adolescents are 10 times more likely to be diagnosed with AIDS than white adults and adolescents. The primary risk factor for black men who developed HIV is sexual contact. In 2005, black MSM were much more likely to be infected with HIV. Another risk factor is when black men engage in high-risk heterosexual behavior (CDC, 2009a).
Some black men who engage in sex with other men identify themselves as heterosexuals because of the stigma and homophobia issues. Many black MSM are secretive about their homosexuality or choose not to identify their sexual orientation. This phenomenon is known as keeping it on the “down low.” Prevention programs are challenged when people do not identify themselves as engaging in risky behaviors or having increased risk factors.
The number of women who have been infected is growing. In 2005 females accounted for 26% of new HIV/AIDS diagnoses, and most of the females were black (CDC, 2007c). HIV was the leading cause of mortality in black women between 25 and 34 years of age. Black women are 23 times more likely to be diagnosed with AIDS than white women. Young people between 15 and 24 years old make up 40% of the new diagnoses (CDC, 2007d). Most people are diagnosed between 25 and 44 years of age. In 2007, an estimated one half of all people infected with HIV/AIDS did not receive appropriate health care, and 25% were not yet diagnosed (Henry J. Kaiser Family Foundation, 2007).
During 2006, Hispanics accounted for almost 20% of the total number of HIV/AIDS cases in the United States (CDC, 2007b). Many socioeconomic and cultural factors have contributed to this epidemic and associated prevention challenges in the U.S. Hispanic and Latino communities. The primary risk factor for developing HIV in Hispanic men and women is sex with men. Hispanics also have higher rates than non-Hispanic whites of other sexually transmitted infections (STIs), including chlamydia, gonorrhea, and syphilis (CDC, 2007b). Transient Hispanic populations often have difficulty receiving access to health care because of social structure, language barriers, and migration patterns (CDC, 2008). The predicaments caused by poverty lead to limited access to appropriate health care, housing, and HIV prevention. All of these factors may directly or indirectly increase risk factors for HIV infection in the Hispanic population.
In 1996 researchers falsely predicted that HIV cases would increase for injecting drug users (Holmberg, 1996). The biggest increase in new HIV cases has occurred in heterosexual populations. In 1983 heterosexuals made up 5% of new HIV cases. In 2006 that number grew to 36% (CDC, 2008). Drugs that are not injected also affect the spread of HIV because drug users often engage in high-risk behaviors when they are under the influence (CDC, 2008).
As treatment for HIV has advanced, the progression from HIV to AIDS has slowed, resulting in a decreased mortality rate for those infected with HIV. Data from 2006 indicates that, although AIDS cases have remained stable, the death rate has decreased (CDC, 2008). Advanced treatment options mean that people are living longer after their AIDS diagnoses. Unfortunately, in countries where HIV-infected people are without adequate access to health care, HIV infection is still one of the leading causes of death.
Transmission of HIV
Despite significant research into the modes of transmission of HIV, considerable fear and misinformation about HIV transmission, perhaps more than for any other disease, still exists. It is imperative that health care providers and patients be knowledgeable about modes of transmission and behaviors that put them at risk for HIV infection. Modes of transmission have remained constant throughout the course of the HIV pandemic. Health care providers also need to remember that transmission of HIV occurs through sexual practices, not sexual preferences.
The patterns in the spread of HIV changed considerably during the first two decades of the epidemic in the United States. Worldwide, sexual intercourse is by far the most common mode of HIV transmission, but in the United States, as many as one half of all new HIV infections are now associated either directly or indirectly with injection drug use—that is, using HIV-contaminated needles to inject drugs or having sexual contact with an HIV-infected drug user. Overall, compared to the 1980s, HIV infection is spreading fastest in the United States among young people, injecting drug users, women, blacks, and Hispanics. The number of estimated pediatric AIDS cases diagnosed each year has declined since 1992. This decline is associated with the increased compliance with universal counseling and testing of pregnant women and the use of zidovudine (Retrovir, ZDV, AZT) by HIV-infected pregnant women and their newborn infants.
HIV is an obligate virus, meaning it must have a host organism to survive. The virus cannot live long outside the human body. HIV transmission depends on the presence of the virus, the infectiousness of the virus, the susceptibility of the uninfected host, and any conditions that may help put the person at risk. HIV is transmitted from human to human through infected blood, semen, cervicovaginal secretions, and breast milk. If these infected fluids are introduced into an uninfected person, the potential for HIV transmission exists. In addition to the aforementioned body fluids, HIV is also found in pericardial, synovial, cerebrospinal, peritoneal, and amniotic fluids. Vertical transmission of HIV, or transmission from a mother to a fetus, can occur during pregnancy, during delivery, or through postpartum breastfeeding (transmitted in the breast milk). Conditions that affect the likelihood of infection include the duration and frequency of exposure, the amount of virus inoculated, the virulence of the organism, and the host’s defense capability (immune system). Although HIV has been found in other body fluids such as saliva, urine, tears, and feces, there has been no evidence that these substances are capable of transmission, unless the fluids contain visible blood.
HIV is generally transmitted by behaviors and not by casual contacts, such as hugging, dry kissing, shaking hands, or sharing food and utensils. HIV is not transmitted by animals or insects; coughing or sneezing; or sharing objects such as pencils, computer keyboards, or telephones. The three most common modes of HIV transmission are anal or vaginal intercourse, contaminated injecting drug equipment and paraphernalia, and transmission from mother to child.
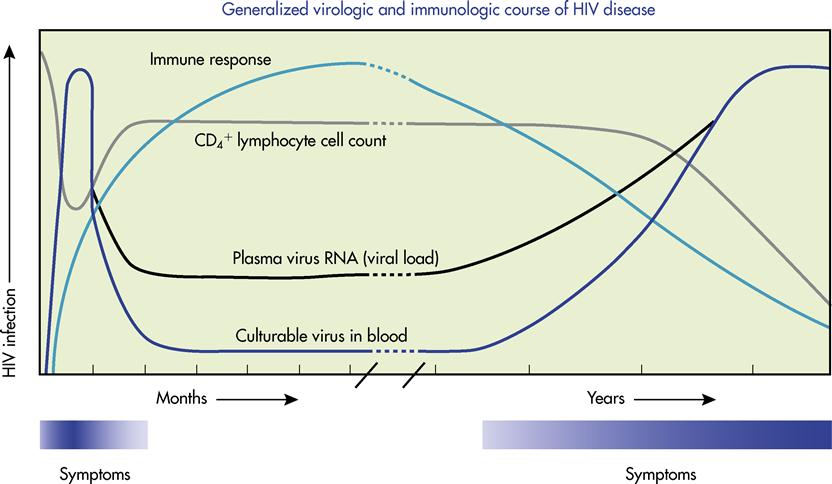
Once infected, an individual is capable of transmitting HIV to others at any time throughout the disease spectrum, even when the host appears healthy and has no obvious signs of immune destruction. In HIV infection the viral load (amount of measurable HIV virions in the blood) is highest immediately after infection and during the later stages of the disease (Figure 16-1). During these periods, unprotected exposure (through sexual behaviors or blood) to an infected individual increases the likelihood that transmission will occur. However, it is important to remember that HIV can be transmitted during the entire disease spectrum.
Sexual transmission
Sexual transmission of HIV remains the most common mode of transmission in the world today and is responsible for the majority of the world’s total AIDS cases. Sexual activity provides the potential for the exchange of semen, cervicovaginal secretions, and blood. The sexual orientation or sexual practices of an individual are irrelevant in HIV transmission. Factors that are important are the presence of HIV in one or both partners and the occurrence of behaviors that puts one or both partners at risk for transmission. Some individuals become infected with HIV after a single unprotected sexual encounter, whereas others remain free from infection after hundreds of such encounters.
Although the majority of HIV transmissions in the United States occur in the MSM category via receptive anal intercourse, heterosexual transmission via anal intercourse is becoming increasingly prevalent. Heterosexual couples may prefer this method of sexual expression or use it because it eliminates the risk of pregnancy. Unfortunately, the most risky sexual activity is unprotected receptive anal intercourse. Because the rectum is generally tighter and less well lubricated than the vagina, the rectal mucosa may be torn, providing an excellent portal for the virus to enter the bloodstream.
During any form of sexual intercourse (anal, vaginal, oral), the risk of infection is considerably higher for the receptive partner, although infection can be transmitted to an insertive partner as well. The receptive partner generally has prolonged exposure to semen (National Institute of Allergy and Infectious Diseases, 2006). Other factors that may increase the risk of sexual transmission include ulcerating genital diseases, such as herpes simplex virus (HSV) and syphilis; chancres secondary to STIs; intact (uncircumcised) foreskin; sex that is “rough”; and immunosuppression due to drug use, including the use of nicotine and alcohol. Infection risk for HIV can also be increased during intercourse when the infected partner has a high viral load. An increased viral load is often found in the primary and late stages of infection (Klimas et al., 2008). Oral-genital transmissions have been reported but are considered rare, and experts disagree on whether this constitutes an actual mode of transmission.
Parenteral exposure
Injecting drug use
HIV may be transmitted by exposure to contaminated blood through the accidental or intentional sharing of injecting equipment and paraphernalia. Such equipment includes syringes, needles, cookers (spoons or bottle caps used for mixing the drug), and filtering devices (such as cotton balls). Injecting drug users represent the second highest exposure category, following the MSM category (CDC, 2006). Although typically seen in large metropolitan areas, injecting drug use occurs in smaller cities and rural areas as well. Injection is not limited to illicit drugs; HIV can be transmitted via contaminated “works” used to inject steroids, vitamins, and insulin.
Injecting drug users confirm needle placement in a vein by drawing back blood into the syringe; the substance is then injected into the vein. They may also draw blood back into the syringe and inject numerous times, a procedure called “booting.” This ensures that no substance remains in the syringe. Other factors that put injecting drug users at risk for HIV include poor nutritional status, poor hygiene, and impaired judgment due to mood-altering substances. The long-term effects of injecting drug use put individuals at increased risk for other diseases, such as hepatitis B, hepatitis C, and other bloodborne illnesses.
Blood and blood products
Since 1985, blood banks in the United States have screened all donated blood for HIV-1 antibodies, and since 1992 they have also screened for HIV-2. Blood banks have also implemented procedures to find blood donors who might be at high risk for being infected with HIV. Blood from donors who are deemed high risk or that tests positive for HIV is discarded. In addition to HIV, blood is currently screened for HTLV-1, HTLV-2, hepatitis B virus, syphilis, and hepatitis C virus.
Every year, a small number of blood donations come from donors who are infected with HIV but in whom the HIV antibody was undetected. When a blood donor has not yet undergone seroconversion (a change in serologic test results from negative to positive as antibodies develop in reaction to an infection), the current HIV antibody test is unable to detect the infection. In the past there was a 22-day window where the donor could donate HIV-infected blood that would not be detected by the HIV-1 and HIV-2 antibody test. Since 1995, however, blood has also been screened for HIV-1 p24 antigen. With this addition, this window has been reduced to 16 days. In 1999, another test called the nucleic acid amplification test was introduced. This test detects HIV-1 ribonucleic acid (RNA) and has reduced the window again to only 11 days. By 2003, after 25 million donations, only three people were infected with HIV after receiving a blood product transfusion. The blood came from two separate donors, and the blood tested negative for HIV with all currently available HIV tests (Donnegan, 2003).
Before 1985, people who received replacement clotting factors for blood coagulation difficulties had an increased risk of contracting HIV. Since 1985, a recombinant technique is used to manufacture the clotting factors or the clotting factors are treated with chemicals or heated to kill the HIV.
Occupational exposure
Almost 25,000 adults who developed AIDS before 2003 were health care workers. This represents 5% of all AIDS cases among adults who had a known occupation.
According to the CDC, there is a distinction between a “documented” and a “possible” HIV seroconversion. When the infection is documented, it means that the individual had a documented exposure related to the occupation and developed HIV. A possible infection indicates that the individual worked in a high-risk setting with exposure to blood or other body fluids related to his or her occupation. However, there was no documented exposure event.
In the United States at the time this was written, 46% (26) of the 57 health care workers who were infected with HIV as a result of a documented occupational exposure had developed AIDS. Of those health care workers with possible exposures, 121 of 138 developed AIDS (Sepkowitz & Eisenberg, 2005). Of all health care workers with HIV, most did not have a documented exposure, and the source of their infection is thought to be from high-risk sexual behavior.
Most of the health care workers who have been infected with HIV are nurses. The second largest group is laboratory clinicians, and the third largest group is physicians (nonsurgical). Other health care workers with possible exposures included emergency medical technicians, health care aides, housekeepers, and maintenance workers. Most of the infections occurred after a needlestick injury with resulting puncture wound. There is thought to be some underreporting of exposures because it is voluntary. If a health care worker does have a needlestick resulting in exposure to a known HIV-infected person, the risk for contracting HIV is low, at just about 0.3%.
As of this writing, the last new HIV case involving a possible exposure to an HIV/AIDS patient was in 2000 (CDC, 2007f). Some cases are still being investigated.
Needlesticks that occur when a health care worker is exposed to known HIV-infected persons are known as percutaneous exposure. If the exposure involves a hollow-bore needle filled with blood that is placed in the patient’s vein or artery, then the transmission risk of HIV is increased. Also, the transmission risk is increased if the health care worker suffers a deep injury at the time of the exposure. Scalpels, suture needles, and smaller gauge injection needles also pose a risk for transmission, but it is much smaller. If only the mucous membranes are exposed during the incident, then the risk for seroconversion is only 0.09%. There is a small risk for seroconverting if the health care worker’s skin is not intact and is exposed to blood or body fluids.
Unfortunately, postexposure antiviral therapy given to health care workers after a documented exposure may result in severe hepatitis that may require a liver transplant. Some health care workers have died after documented or possible exposure to HIV, but that number has not been reported at this time.
Perinatal (vertical) transmission
HIV infection can be transmitted from a mother to her infant during pregnancy, at the time of delivery, or after birth through breastfeeding. In the United States, it is estimated that approximately 30% of infected mothers will transmit HIV to their infants, with approximately 50% to 70% of the transmissions occurring late in utero or intrapartum. For unknown reasons, the rate of vertical transmission varies around the world; the rate in France is around 11%, but it is nearly 50% in parts of Africa. Factors such as the stage of maternal HIV disease (it is more likely to be transmitted during the initial and later stages of infection, when more of the virus is circulating in the mother’s blood and body fluids), a decreased CD4+ count or high viral load, the presence or absence of STIs, and the mother’s nutritional status all play a role in vertical transmission. Factors that increase the risk of transmission during delivery include extreme prematurity; complicated pregnancies leading to extended labor; the mixing of maternal and fetal blood; newborn ingestion of maternal blood, amniotic fluid, or vaginal secretions; skin excoriation in the newborn; and being the first child born in a multiple gestation.
In 1994 the AIDS Clinical Trials Group (ACTG) 076 study demonstrated that a plan of zidovudine therapy started after the 14th week of gestation, given intravenously to the mother during delivery and including zidovudine syrup given to the infant after birth, reduces the risk of HIV transmission by 67% (Perinatal HIV Guidelines Working Group, 2001). The long-term effects of zidovudine or combination therapy are not known, but anecdotal evidence suggests that polydactyly (the congenital presence of more than the normal number of fingers and toes) and ventricular septal defect may be caused by zidovudine. It is difficult to determine whether these defects are caused by in utero exposure to the drug or whether the incidence is the same as in the general population. Children who received zidovudine in the womb and for the first 6 weeks of life are closely monitored by authorities to document any long-term side effects.
In addition to drug therapy, substantial advances have been made in understanding the pathophysiology, treatment, and monitoring of HIV infection. These advances have resulted in changes in the standard of care for individuals, including pregnant women, with HIV infection. More aggressive combination drug regimens that provide maximal viral suppression are now recommended. Although pregnancy alone is not a reason to defer treatment, the use of anti-HIV drugs during pregnancy requires special consideration. Unfortunately, no long-term data regarding the long-term effects on the fetus exist. Because of this, offering antiretroviral therapy (ART) to HIV-infected women—whether to primarily treat HIV infection or to reduce the likelihood of perinatal transmission—should be accompanied by a discussion of the known and unknown short- and long-term benefits and potential risks. Because of the findings of ACTG 076, zidovudine should be a part of this treatment regimen.
An HIV-positive pregnant woman should be given this information to make an informed decision about treatment options. Current recommendations call for routine HIV counseling and voluntary HIV testing of pregnant women and those women considering pregnancy. However, there are no legal requirements that a woman take zidovudine during pregnancy or that she be tested for HIV antibodies.
The HIV transmission rates from mother to child have been reduced due to several recommended interventions. This includes ART, formula feeding, and cesarean section. In developed countries, this number has decreased from 25% (without interventions) to less than 2%. In countries where ART is not available and mothers continue to breastfeed, by age 2 the infection rate for babies born to HIV-infected mothers can be as high as 25%. Infants born to HIV-infected mothers have positive HIV antibody results as long as 15 to 18 months after birth. This is caused by maternal antibodies that cross the placenta during gestation and remain in the infant’s circulatory system. An earlier diagnosis of HIV infection can be made by doing an HIV viral culture or by measuring the amount of HIV RNA or viral load through a technique called polymerase chain reaction (PCR) or branched chain DNA testing (bDNA).
Pathophysiology
HIV is classified as “slow” retrovirus or a lentevirus. After infection with these types of viruses, a long time passes before specific signs and symptoms appear. HIV requires cells for replication. The virus takes over the host cell and reproduces viral copies of itself. Retroviruses are made of RNA. Most organisms’ genetic material is made up of deoxyribonucleic acid (DNA). The retrovirus uses an enzyme called reverse transcriptase to make its RNA change to DNA. This process allows the virus to be incorporated into the host’s genetic material (Smith & Daniel, 2006).
HIV can cross over into the host at the dendritic immune cells that are located in the mucosal layer of the vulva, the vagina, the rectum, and the penis. The exterior layer of the dendritic cell passes the virus into the interior portion of the cell. The HIV virus is released into the lymphatic system via tissue or lymph nodes. Then the virus binds to a CD4+ lymphocyte (a type of white blood cell; a protein on the surface of cells that normally helps the body’s immune system combat disease), where it can travel farther into the lymphatic system and begin the initial infectious cycle (Lekkerkerker et al., 2006).
When the viral particle attaches to the host cell’s CD4+ receptor and coreceptor (CCR5 or CXCR4), this is the first step in replication of the virus (see Figure 16-1). The HIV virion enters the host cell when the virus binds with the cell. After binding to the cell, coreceptors are needed to continue the fusion process and to allow the viral particle to eject two copies of the virus’s RNA. Inside the cell, HIV reverse transcriptase changes the viral RNA into DNA. A full copy of this DNA is created and broken down into smaller more functional pieces that are moved to the nucleus of the cell (Smith & Daniel, 2006). The HIV DNA moves into the nucleus of the cell, where viral integrase helps insert it into the DNA of the host. The inserted virus is called a provirus. After activation, the cell makes a new copy of HIV by using viral proteins. Afterward, there is an abnormal amount of immune activation, and this perpetuates the progress of the HIV infection because it creates more CD4+ cells that will be under attack by HIV and will eventually exhaust the immune system (Potter et al., 2007). The number of CD8+ T cells that are activated at this time is directly related to an increased risk of developing advanced HIV infection, or AIDS. However, the HIV can remain dormant for years if the CD4+ cell remains inactivated (Potter et al., 2007). It has been difficult to completely control HIV because of its ability to remain undetected. Patients with HIV are advised to continue taking their antiretroviral medications.
New viral proteins are created when the infected CD4+ cell converts DNA into RNA. This process is called transcription. The process relies on the host cell and the viral genetic material. The new RNA is called messenger RNA (mRNA), and it is returned from the nucleus back into the cytoplasm. In the cytoplasm, mRNA is used as a template to begin making HIV protein. This process is called translation. The protein sequence of the mRNA is changed back into RNA, and this makes up the outer envelope and inner core of HIV. After translation the genetic materials become smaller and smaller pieces of viral material. The viral protease chunks the genetic products into smaller pieces so that they can infect more CD4+ host cells. This HIV protease is specific to this virus and is targeted by a class of medications called protease inhibitors that is used to manage HIV. The envelope’s viral proteins are joined together inside the host cell’s membrane, with the core proteins, RNA, and enzymes just inside the membrane.
HIV then “buds” by pinching off this cell (Smith & Daniel, 2006). One infected CD4+ cell has the ability to quickly make thousands of cell copies. The CD4+ cell dies due to this replication process. As time goes on, so many CD4+ cells are destroyed that the immune system becomes dysfunctional and OIs develop within the host.
Influences on viral load and disease progression
HIV replicates quickly after entering the host body. It can rapidly produce billions of copies, which infect CD4+ cells and the lymphatic system. The viral load of the host during the early stage of the infection can be extremely high and increases transmission risk to others who are exposed. The severity and progression of the infection are related to the host’s infection with other STIs, age, and immune response (Fletcher & Klimas, 2007). Basic host immune defenses (cellular and humoral) help limit replication and slow progression of HIV. Unfortunately, these immune responses cannot completely eliminate HIV from the host. The host can remain healthy appearing even when infected with the virus (Table 16-2). Some patients live with the virus for at least 10 years without any treatment and appear healthy. They are referred to as long-term nonprogressors. When HIV patients who were also coinfected with another type of virus took ART, their CD4+ count was low (Cheng et al., 2007). When older people do not use ART, their rate of disease progression is much faster than in younger people. It is thought to be related to more pathogen exposure over their life, an increased number of memory CD4+ cells (which are targeted by HIV), and fewer numbers of naïve CD4+ cells. Older people tend to have a harder time keeping up with the demand to produce more CD4+ cells.
Table 16-2
Types of White Blood Cells and their Involvement in HIV Disease
| WHITE BLOOD CELL (WBC) TYPE | DESCRIPTION OF FUNCTION | ROLE IN HIV DISEASE |
| Neutrophils | Neutrophils normally constitute 50%-75% of all circulating leukocytes and are capable of phagocytosis. Important in the inflammatory response and the first line of defense against infection. Short life span. | Neutropenia (decreased WBC) commonly occurs in advanced HIV disease. Drug-induced neutropenia is common, especially with drugs used to treat PCP, toxoplasmosis, CMV retinitis or colitis, and with NRTI usage. |
| Monocytes, macrophages | Constitute about 3%-7% of all WBCs. Macrophages are distributed throughout tissue and are capable of phagocytosis. Involved in the inflammatory response. Capable of processing antigens for presentation to T cells. They have CD4+ receptors. | Monocytes and macrophages serve as a reservoir for HIV. When activated by stimulation with interferon (inflammatory response), they produce neopterin. Neopterin levels are increased in HIV disease. |
| Basophils, mast cells | Basophils and mast cells are involved in acute inflammation; breakdown of mast cells releases histamine and other factors. | In HIV infection, may inhibit leukocyte migration. |
| T-helper cells (CD4+ or T4 cells) | T-helper cells contain CD4+ receptors. They are considered the “conductor” of the immune system because of their secretion of cytokines, which control most aspects of the immune response. | Major target of HIV. Progressive infection gradually destroys the available pool of T-helper cells so that the overall CD4+ cell count drops. Lower CD4+ cell counts correspond with more immunodeficiency and the onset of opportunistic infections. Infection with HIV can impair T-helper cell function without killing the cell. |
| Cytotoxic T cells or cytotoxic T lymphocytes (CTL, CD8+ cell) | Cytotoxic T cells contain CD8+ receptors and produce cytokines in a more limited fashion than CD4+ cells. They regulate viral and bacterial infections and are involved in direct killing of target cells by binding to them and releasing a substance that can perforate the cell membrane. | Increase in HIV infection. Represent the cellular response to infection. The strength of this initial cellular response has been shown to predict progression to AIDS (i.e., better cell response equals slower disease progression). Cytotoxic T cells kill T-helper cells infected with HIV. |
| Natural killer (NK) cells | Large granular lymphocytes involved in cell-mediated immune response. Target cells are coated with antibody that binds to receptors on the surface of NK cells, allowing the NK cell to attach to the target cell and kill them. NK cells kill target cells by releasing a substance that triggers lysis (breakdown of cell wall) of cell. | Retain normal counts and normal structure in patients with HIV infection, but they are functionally defective. |
| B cells | B cells produce antibodies specific to an antigen. They are capable of being stimulated by T-helper cells. | B cells are involved in the humoral response to HIV infection and produce a variety of antibodies against HIV. Present throughout the course of HIV disease. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 d-H
d-H R-
R- ns,
ns,  R-
R- -l
-l nt,
nt,