Preventing infection
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Identify what microbes need to live and grow.
• List the signs and symptoms of infection.
• Explain the chain of infection.
• Describe healthcare-associated infections and the persons at risk.
• Describe the practices of medical asepsis.
• Describe disinfection and sterilization methods.
• Explain how to care for equipment and supplies.
• Describe Standard Precautions and Transmission-Based Precautions.
• Explain the Bloodborne Pathogen Standard.
• Explain the principles and practices of surgical asepsis.
• Perform the procedures described in this chapter.
Key terms
asepsis Being free of disease-producing microbes
biohazardous waste Items contaminated with blood, body fluids, secretions, or excretions; bio means life, and hazardous means dangerous or harmful
clean technique See “medical asepsis”
communicable disease A disease caused by pathogens that spreads easily; a contagious disease
contagious disease See “communicable disease”
contamination The process of becoming unclean
disinfection The process of destroying pathogens
germicide A disinfectant applied to the skin, tissues, or non-living objects
healthcare-associated infection (HAI) An infection that develops in a person cared for in any setting where health care is given; the infection is related to receiving health care
immunity Protection against a certain disease
infection A disease state resulting from the invasion and growth of microbes in the body
infection control Practices and procedures that prevent the spread of infection
medical asepsis Practices used to remove or destroy pathogens and to prevent their spread from one person or place to another person or place; clean technique
microbe See “microorganism”
microorganism A small (micro) living plant or animal (organism) seen only with a microscope; a microbe
non-pathogen A microbe that does not usually cause an infection
normal flora Microbes that live and grow in a certain area
pathogen A microbe that is harmful and can cause an infection
reservoir The environment in which a microbe lives and grows; host
spore A bacterium protected by a hard shell
sterile The absence of all microbes
sterile field A work area free of all pathogens and non-pathogens (including spores)
sterile technique See “surgical asepsis”
sterilization The process of destroying all microbes
surgical asepsis The practices that keep items free of all microbes; sterile technique
vaccination Giving a vaccine to produce immunity against an infectious disease
vaccine A preparation containing dead or weakened microbes
KEY ABBREVIATIONS
| AIIR | Airborne infection isolation room |
| CDC | Centers for Disease Control and Prevention |
| cm | Centimeter |
| HAI | Healthcare-associated infection |
| HBV | Hepatitis B virus |
| HIV | Human immunodeficiency virus |
| MDRO | Multidrug-resistant organism |
| MRSA | Methicillin-resistant Staphylococcus aureus |
| OPIM | Other potentially infectious materials |
| OSHA | Occupational Safety and Health Administration |
| PPE | Personal protective equipment |
| TB | Tuberculosis |
| VRE | Vancomycin-resistant Enterococcus |
An infection is a disease state resulting from the invasion and growth of microbes in the body. Infection is a major safety and health hazard. Minor infections cause short illnesses. Some infections are serious and can cause death. Older and disabled persons are at risk. The health team follows certain practices and procedures to prevent the spread of infection. Called infection control, such practices and procedures protect residents, visitors, and staff from infection.
Microorganisms
A microorganism (microbe) is a small (micro) living plant or animal (organism). It is seen only with a microscope. Microbes are everywhere—in the mouth, nose, respiratory tract, stomach, and intestines. They are on the skin and in the air, soil, water, and food. They are on animals, clothing, and furniture.
Some microbes are harmful and can cause infections. They are called pathogens. Non-pathogens are microbes that do not usually cause an infection.
Types of microbes
There are five types of microbes:
Requirements of microbes
Microbes need a reservoir to live and grow. The reservoir (host) is the environment in which a microbe lives and grows. People, plants, animals, the soil, food, and water are common reservoirs. Microbes need water and nourishment from the reservoir. Most need oxygen to live. A warm and dark environment is needed. Most grow best at body temperature. They are destroyed by heat and light.
Normal flora
Normal flora are microbes that live and grow in a certain area. Certain microbes are in the respiratory tract, in the intestines, and on the skin. They are non-pathogens when in or on a natural reservoir. When a non-pathogen is transmitted from its natural site to another site or host, it becomes a pathogen. Escherichia coli (E. coli) is found in the colon. If it enters the urinary system, it can cause an infection.
Multidrug-resistant organisms
Multidrug-resistant organisms (MDROs) are microbes that can resist the effects of antibiotics. Antibiotics are drugs that kill microbes that cause infections. Some microbes can change their structures. This makes them harder to kill. They can survive in the presence of antibiotics. Therefore the infections they cause are hard to treat.
MDROs are caused by doctors prescribing antibiotics when they are not needed (over-prescribing). Not taking antibiotics for the length of time prescribed is another cause.
Two common MDROs are resistant to many antibiotics:
Infection
A local infection is in a body part. A systemic infection involves the whole body. (Systemic means entire.) The person has some or all of the signs and symptoms listed in Box 15-1.
Infection in older persons
The immune system protects the body from disease and infection (Chapter 9). Like other body systems, changes occur in the immune system with aging. Therefore older persons are at risk for infection.
During an infection, an older person may not show the signs and symptoms listed in Box 15-1. The person may have only a slight fever or no fever at all. Redness and swelling may be very slight. The person may not complain of pain. Confusion and delirium may occur (Chapter 44).
An infection can become life-threatening before the older person has obvious signs and symptoms. You must be alert to the most minor changes in the person’s behavior or condition. Report any concerns to the nurse at once.
Healing takes longer than when younger. Therefore an infection can prolong the rehabilitation process. Independence and quality of life are affected.
The chain of infection
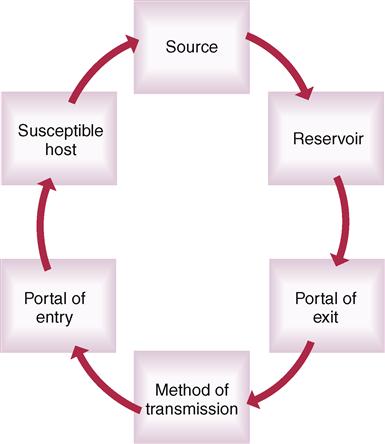
The chain of infection (Fig. 15-1) is a process involving a:
• Source
The source is a pathogen. It must have a reservoir where it can grow and multiply. Humans and animals are reservoirs. If they do not have signs and symptoms of infection, they are carriers. A carrier is a human or animal that is a reservoir for microbes but does not have the signs and symptoms of infection. Carriers can pass the pathogen to others. To leave the reservoir, the pathogen needs a portal of exit. Exits are the respiratory, gastro-intestinal (GI), urinary, and reproductive tracts; breaks in the skin; and the blood.
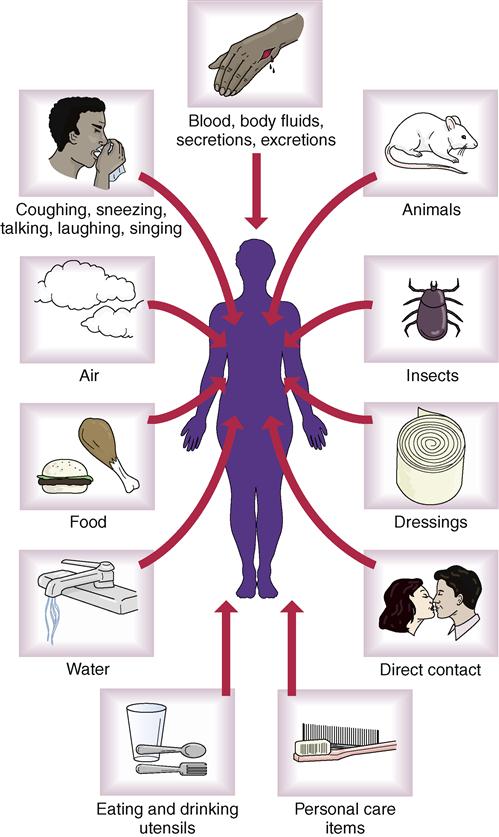
After leaving the reservoir, the pathogen must be transmitted to another host (Fig. 15-2). The pathogen enters the body through a portal of entry. Portals of entry and exit are the same (respiratory, GI, urinary, and reproductive tracts; breaks in the skin; blood). A susceptible host is needed for the microbe to grow and multiply. Susceptible hosts are persons at risk for infection. They include persons who:
The human body can protect itself from infection. The ability to resist infection relates to age, nutrition, stress, fatigue, and health. Drugs, disease, and injury also are factors.
Healthcare-associated infection
A healthcare-associated infection (HAI) is an infection that develops in a person cared for in any setting where health care is given. The infection is related to receiving health care. Hospitals, nursing centers, clinics, and home care settings are examples. HAIs also are called nosocomial infections. (Nosocomial comes from the Greek word for hospital.) HAIs are caused by normal flora. Or they are caused by microbes transmitted to the person from other sources.
For example, E. coli is normally in the colon. Feces contain E. coli. Poor wiping after bowel movements can cause E. coli to enter the urinary system. The hands can transmit E. coli to other body areas. If hand washing is poor, E. coli spreads to any body part or anything the hands touch. It also can be transmitted to other people.
Microbes can enter the body through equipment used in treatments, therapies, and tests. Such items must be free of microbes. Staff can transfer microbes from one person to another and from themselves to others. Common sites for HAIs are:
Older persons have a hard time fighting infections. The health team must prevent the spread of infection. HAIs are prevented by:
Medical asepsis
Asepsis is being free of disease-producing microbes. Microbes are everywhere. Measures are needed to achieve asepsis. Medical asepsis (clean technique) is the practices used to:
• Remove or destroy pathogens. The number of pathogens is reduced.
• Prevent pathogens from spreading from one person or place to another person or place.
Microbes cannot be present during surgery or when instruments are inserted into the body. Open wounds (cuts, burns, incisions) require the absence of microbes. They are portals of entry for microbes. Surgical asepsis (sterile technique) is the practices that keep items free of all microbes. Sterile means the absence of all microbes—pathogens and non-pathogens. Sterilization is the process of destroying all microbes (pathogens and non-pathogens).
Contamination is the process of becoming unclean. In medical asepsis, an item or area is clean when it is free of pathogens. The item or area is contaminated if pathogens are present. A sterile item or area is contaminated when pathogens or non-pathogens are present.
Common aseptic practices
Aseptic practices break the chain of infection. To prevent the spread of microbes, wash your hands:
• After urinating or having a bowel movement.
• After changing tampons or sanitary pads.
• After coughing, sneezing, or blowing your nose.
• Before and after handling, preparing, or eating food.
• Provide all persons with their own linens and personal care items.
• Bathe, wash hair, and brush your teeth regularly.
• Wash fruits and raw vegetables before eating or serving them.
• Wash cooking and eating utensils with soap and water after use.
See Residents With Dementia: Common Aseptic Practices.
 Hand hygiene
Hand hygiene
Hand hygiene is the easiest and most important way to prevent the spread of infection. Your hands are used for almost everything. They are easily contaminated. They can spread microbes to other persons or items. Practice hand hygiene before and after giving care. See Box 15-2 for the rules of hand hygiene.
See Promoting Safety and Comfort: Hand Hygiene, p. 188.
Supplies and equipment
Most health care equipment is disposable. Single-use items are discarded after use. A person uses multi-use items many times. They include bedpans, urinals, wash basins, water pitchers, drinking cups, and glasses. Do not “borrow” them for another person. Disposable items help prevent the spread of infection.
Non-disposable items are cleaned and then disinfected. Then they are sterilized.
Cleaning
Cleaning reduces the number of microbes present. It also removes organic matter such as blood, body fluids, secretions, and excretions. To clean equipment:
• Wash the item with soap and hot water.
• Scrub thoroughly. Use a brush if necessary.
• Rinse the item in warm water.
• Disinfect or sterilize the item.
• Disinfect equipment and the sink used in the cleaning procedure.
Nursing centers have “clean” and “dirty” utility rooms. Equipment is cleaned in the “dirty” utility room. Then it is disinfected or sterilized in the “clean” utility room.
Disinfection
Disinfection is the process of destroying pathogens. Spores are not destroyed. Spores are bacteria protected by a hard shell. Spores are killed by very high temperatures.
Germicides are disinfectants applied to skin, tissues, and non-living objects. Alcohol is a common germicide.
Chemical disinfectants are used to clean surfaces. Counters, tubs, and showers are examples. They also are used to clean re-usable items. Such items include:
See Promoting Safety and Comfort: Disinfection.
Sterilization
Sterilizing destroys all non-pathogens and pathogens, including spores. Very high temperatures are used. Microbes are destroyed by heat.
Boiling water, radiation, liquid or gas chemicals, dry heat, and steam under pressure are sterilization methods. An autoclave (Fig. 15-8) is a pressure steam sterilizer. Glass, surgical items, and metal objects are autoclaved. High temperatures destroy plastic and rubber items. They are not autoclaved. Steam under pressure sterilizes objects in 30 to 45 minutes.

Other aseptic measures
Hand hygiene, cleaning, disinfection, and sterilization are important aseptic measures. So are the measures listed in Box 15-3. They are useful in home, work, and everyday life.