Barbara Lauritsen Christensen
Care of the patient with an immune disorder
Objectives
1. Differentiate between natural and acquired immunity.
2. Compare and contrast humoral and cell-mediated immunity.
3. Explain the concepts of immunocompetence, immunodeficiency, and autoimmunity.
4. Review the mechanisms of immune response.
5. Discuss five factors that influence the development of hypersensitivity.
6. Identify the clinical manifestations of anaphylaxis.
7. Outline the immediate aggressive treatment of systemic anaphylactic reaction.
10. Explain an immunodeficiency disease.
11. Discuss the cause of autoimmune disorders.
12. Explain plasmapheresis in the treatment of autoimmune diseases.
Key terms
adaptive immunity ( -D
-D P-t
P-t v
v  -M
-M -n
-n -t
-t , p. 720)
, p. 720)
anaphylactic shock ( n-
n- -fl
-fl k-t
k-t c, p. 727)
c, p. 727)
attenuated ( -T
-T N-
N- –
– t-
t- d, p. 723)
d, p. 723)
autologous ( w-T
w-T L-
L- -g
-g s, p. 729)
s, p. 729)
cellular immunity (S L-
L- -l
-l r
r  -M
-M -n
-n -t
-t , p. 722)
, p. 722)
humoral immunity (H -m
-m r-
r- l
l  -M
-M -n
-n -t
-t , p. 721)
, p. 721)
hypersensitivity (h -p
-p r-s
r-s n-s
n-s -T
-T V-
V- -t
-t , p. 724)
, p. 724)
immunization ( m-
m- -n
-n -Z
-Z -sh
-sh n, p. 721)
n, p. 721)
immunocompetence ( m-
m- -n
-n -K
-K M-p
M-p -t
-t ns, p. 719)
ns, p. 719)
immunodeficiency ( m-
m- -n
-n -d
-d -F
-F SH-
SH- n-s
n-s , p. 730)
, p. 730)
immunology ( m-
m- -N
-N L-
L- -j
-j , p. 720)
, p. 720)
immunosuppressive ( m-
m- -n
-n -s
-s -PR
-PR -s
-s v, p. 729)
v, p. 729)
immunotherapy ( m-
m- -n
-n -TH
-TH R-
R- -p
-p , p. 723)
, p. 723)
innate immunity ( -N
-N T
T  -M
-M -n
-n -t
-t , p. 720)
, p. 720)
plasmapheresis (pl z-m
z-m -f
-f -R
-R -s
-s s, p. 731)
s, p. 731)
proliferation (pr -l
-l f-
f- -R
-R -sh
-sh n, p. 721)
n, p. 721)
Nature of immunity
The human body exists in an environment of antagonistic forces that are constantly attacking and threatening its integrity. In response to these onslaughts, the body exhibits a wide array of adaptations to protect against external and internal harmful agents. This chapter deals with those mechanisms.
The word immune is derived from the Latin word immunis, meaning “free from burden.” Immunology is an evolving science that essentially deals with the body’s ability to distinguish self from nonself. The body makes this distinction through a complex network of highly specialized cells and tissues that are collectively called the immune system. The immune system (also called the host defense system) is critical to our survival.
The immune system has three main functions: (1) to protect the body’s internal environment against invading microorganisms by destroying foreign antigens and pathogens thus preventing the development of infections (Lewis et al., 2007); (2) to maintain homeostasis by removing damaged cells from the circulation, thereby maintaining the body’s various cell types in an unchanged and uniform form (Lewis et al., 2007); and (3) to serve as a surveillance network for recognizing and guarding against the development and growth of abnormal cells. Abnormal cells (mutations) are constantly being formed in the body but are recognized as abnormal cells and are destroyed (Lewis et al., 2007). When the immune system responds appropriately to a foreign stimulus, the body’s integrity is maintained; this is called immunocompetence.
Immunocompetence is the immune system’s ability to mobilize and use its antibodies and other responses to stimulation by an antigen. If the immune response is too weak or too vigorous, homeostasis is disrupted, causing a malfunction in the system. This is called immunoincompetence. With disruption of the homeostatic balance of the immune system, a number of diseases develop. Inappropriate immune responses are classified into four categories: (1) hyperactive responses against environmental antigens (e.g., allergy); (2) inability to protect the body, as in immunodeficiency disorders (e.g., acquired immunodeficiency syndrome [AIDS]); (3) failure to recognize the body as self, as in autoimmune disorders (e.g., systemic lupus erythematosus); and (4) attacks on beneficial foreign tissue (e.g., organ transplant rejection or transfusion reaction).
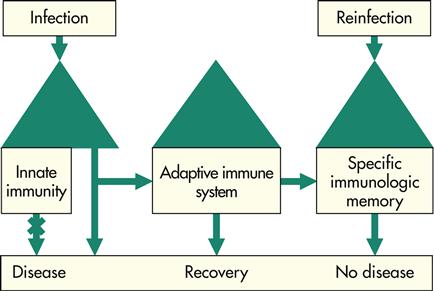
Immunity is the quality of being insusceptible to or unaffected by a particular disease or condition. Immunity has two major subclassifications: innate (natural) and adaptive (acquired) (Figure 15-1). Innate immunity is nonspecific, whereas adaptive immunity is specific. The study of the immune system is immunology.
Innate, or natural, immunity
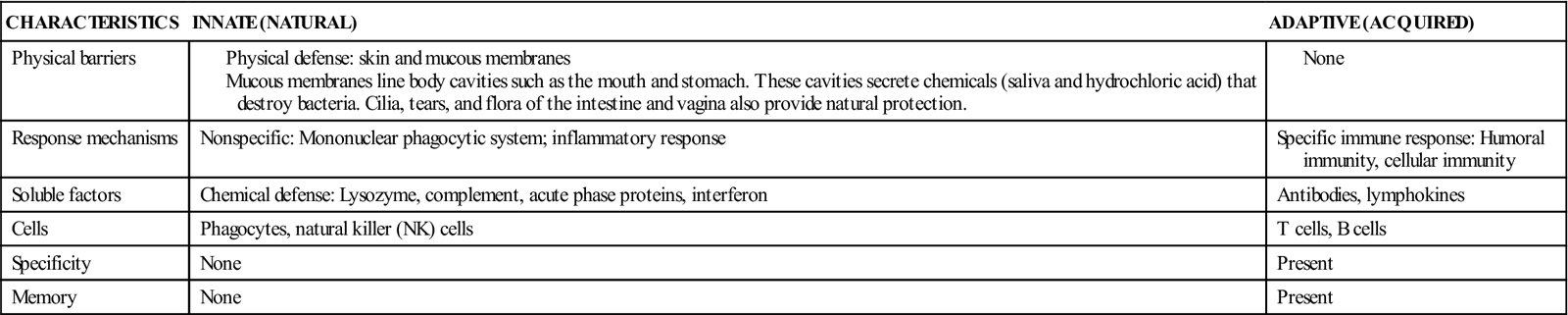
The body’s first line of defense, innate immunity, provides physical and chemical barriers to invading pathogens and protects against the external environment. The innate system is composed of the skin and mucous membranes, cilia, stomach acid, tears, saliva, sebaceous glands, and secretions and flora of the intestine and vagina. These organs, tissues, and secretions provide biochemical and physical barriers to disease. The first line of defense provides nonspecific immunity to the individual (Table 15-1).
Table 15-1
Innate (Natural) and Adaptive (Acquired) Immunity
Adaptive, or acquired, immunity
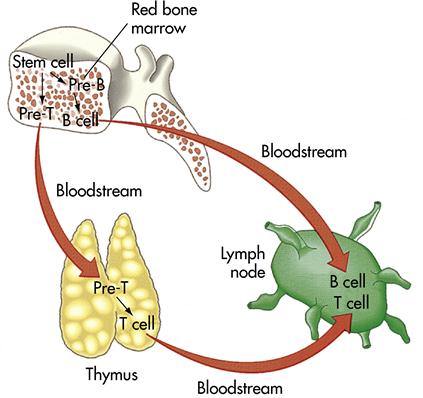
If the components of innate or natural immunity fail to prevent invasion or to destroy a foreign pathogen, the adaptive, or acquired, immune response assists in the battle. This is the body’s second line of defense against disease. Adaptive immunity provides a specific reaction to each invading antigen and has the unique ability to remember the antigen that caused the attack. The adaptive immune system is composed of highly specialized cells and tissues, including the thymus, the spleen, bone marrow, blood, and lymph (Figure 15-2). Adaptive immunity includes both humoral and cell-mediated immunity. The adaptive immune system’s specificity (i.e., being specific) results from the production of antibodies in the cells. Antibodies develop naturally after infection or artificially after vaccinations.
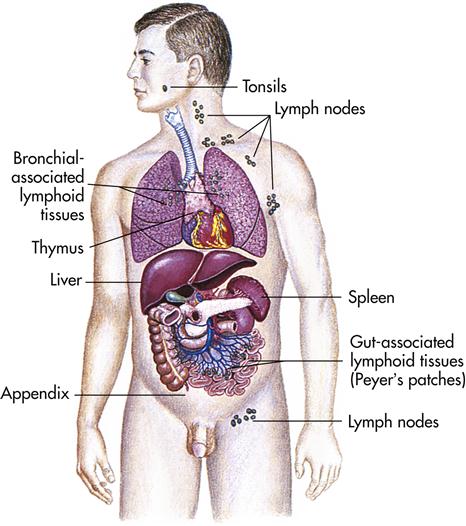
The cells of the immune system are the macrophages (any phagocytic cell involved in defense against infection) and the lymphocytes. When organisms pass the epithelial barriers, phagocytes become activated. Phagocytes also migrate through the bloodstream to the tissues for the body’s second line of defense against disease. Phagocytes engulf and destroy microorganisms that pass the skin and mucous membrane barriers. These cells also assist in the immune response by carrying antigens to the lymphocytes.
Lymphocytes include the T and B cells (Figure 15-3) and the large, granular lymphocytes also known as natural killer, or NK, cells. Approximately 70% to 80% of the lymphocytes are T-cell lymphocytes. When activated, T cells release a substance called lymphokine. Lymphokine attracts macrophages to the site of infection or inflammation and prepares them for attack. T cells cooperate with the B cells to produce antibodies but do not produce antibodies themselves. T cells are responsible for cell-mediated immunity and protect the body against viruses, fungi, and parasites. T cells also provide protection in allografts (transfer of tissue between two genetically dissimilar individuals of the same species) and against malignant cells.
B cells make up approximately 20% to 30% of the lymphocyte population. B cells trigger the production of antibodies and proliferate (increase in number) in response to a particular antigen (a substance recognized by the body as foreign that can trigger an immune response). An antigen is usually a protein that causes the formation of an antibody and reacts specifically with that antibody. B cells migrate to the peripheral circulation and tissues and eventually are filtered from the lymph and stored in the lymphoid tissue of the body.
The initial formation of B cells does not require antigen stimulation or any other environmental stimulus. However, B-cell proliferation (reproduction or multiplication of similar forms) depends on antigen stimulation. B cells are responsible for humoral immunity. B cells produce antibodies and protect against bacteria, viruses, and soluble antigens.
Humoral immunity
Humoral immunity (one of the two forms of immunity that respond to antigens, such as bacteria and foreign tissue) is mediated by the B cells. B cells produce antibodies in response to antigen challenge. On first exposure to a given antigen, a primary humoral response is initiated. This response is generally slow compared with subsequent antigen exposures. When a second exposure occurs, memory B cells cause a quick response, regardless of whether the first exposure was to an antigen or to immunization. Immunization is a process by which resistance to an infectious disease is induced or increased.
Antigen is presented to the T-helper cell population by the macrophages. T lymphocytes can be categorized into T-helper (CD4) and T-suppressor (CD8) cells. An antigen is taken to the B cells and, assisted by T-helper cells, the B cells initiate production of antibodies. T-suppressor cells maintain the humoral response at a level appropriate for the stimulus.
Antibodies produced by one’s own body are said to provide active immunity. An example of active immunity is a person who has been vaccinated against rubeola (red measles). In contrast, temporary, or passive, immunity is provided by antibodies that are formed by one person in response to a specific antigen and administered to another person. An example of passive immunity is hepatitis B immune globulin administered after exposure to hepatitis B virus in a nonimmune person.
Even though humoral immunity is mediated by the B-cell population, T-helper cells and T-suppressor cells are vital to the immunocompetent person. Immunocompetence is the ability of an immune system to mobilize and deploy its antibodies and other responses to stimulation by an antigen. Both the number and functions of the helper and T-suppressor cells help determine the strength and persistence of an immune response. The normal ratio of T-helper cells to T-suppressor cells in the body is 2:1. When this ratio is disrupted, autoimmune and immunodeficient diseases occur. Factors that may weaken immunocompetence include the aging process, viruses, radiation, and chemotherapeutic drugs (Mosby’s Dictionary of medicine, nursing, and health professions, 2009).
Exposure to antigen and response with antibody may activate either (1) the humoral complement (one of the 25 complex enzyme serum proteins) system, which results in breakdown of the bacteria and release of lysosomes to destroy bacteria; or (2) the antigen-antibody reaction, which results in mast cells releasing histamine, which produces the symptoms of allergy. When symptoms of allergy occur, antigen is referred to as allergen (a substance that can produce a hypersensitive reaction in the body but may not be inherently harmful). When immunity results, antigen is referred to as immunogen (any agent or substance capable of provoking an immune response or producing immunity).
Cellular immunity
Cellular immunity, also called cell-mediated immunity (the mechanism of acquired immunity characterized by the dominant role of small T cells), results when T cells are activated by an antigen. Whole cells become sensitized in a process similar to that which stimulates the B cells to form antibodies. Once these T cells have been sensitized, they are released into the blood and body tissues, where they remain indefinitely. On contact with the antigen to which they are sensitized, they attach to the organism and destroy it. Cellular immunity is involved in resistance to infectious diseases caused by viruses and some bacteria.
Cellular immunity is of primary importance in (1) immunity against pathogens that survive inside cells, including viruses and some bacteria (e.g., Mycobacterium organisms); (2) fungal infections; (3) rejection of transplanted tissues; (4) contact hypersensitivity reactions; (5) tumor immunity; and (6) certain autoimmune diseases (Box 15-1).
Hypersensitivity reactions are cell-mediated responses of the body (Box 15-2).
Complement system
The word complement became part of the terminology of immunology at the turn of the nineteenth century, when researchers recognized that blood plasma contained a substance necessary to complete the destruction of bacteria. The complement system includes approximately 25 serum enzymatic proteins that interact with one another and with other components of the innate (natural) and adaptive (acquired) immune systems. Normally, complement enzymes are inactive in plasma and body fluids. When an antigen and antibody interact, the complement system is activated. Complement functions in a “step-by-step” series much like the clotting mechanism, but with a different purpose. The complement system can destroy the cell membrane of many bacterial species, and this action attracts phagocytes to the area.
Genetic control of immunity
More is being discovered about the genetic role in immunity. A genetic link exists to both well-developed immune systems and poorly developed or compromised immune systems.
The immune system develops at different rates and at different times in fetal and early life. Bone marrow serves as an important mechanism of producing stem cells and all the other cells involved in the immune response.
Effects of normal aging on the immune system
With advancing age, there is a decline in the immune system. The primary clinical evidence for this immunosenescence is the high incidence of tumors in older adults. Older adults are also more susceptible to infections (such as influenza and pneumonia) from pathogens that they were relatively immunocompetent against earlier in life.
Aging does not affect all aspects of the immune system. The bone marrow is relatively unaffected by increasing age. However, aging has a pronounced effect on the thymus, which decreases in size and activity. These changes in the thymus are probably a primary cause of immunosenescence. Both T and B cells show deficiencies in activation, transit time through the cell cycle, and subsequent differentiation. However, the most significant alterations seem to involve T cells. As thymic output of T cells diminishes, the differentiation of T cells in peripheral lymphoid structures increases. Consequently, there is an accumulation of memory cells rather than new precursor cells responsive to previously unencountered antigens.
Delayed hypersensitivity response, as determined by skin testing with injected antigens, is frequently decreased or absent in older adults. The clinical consequences of a decline in cell-mediated immunity are evident. Older adults have an increased risk of death from cancer (see Life Span Considerations box).
 L-
L- r-j
r-j n,
n,  N-to-j
N-to-j n,
n,  w-t
w-t –
– -M
-M N,
N,  -M
-M -n
-n -t
-t ,
,  m-
m- -n
-n -j
-j n,
n,  M-f
M-f -k
-k n,
n,