Safety
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Describe accident risk factors.
• Explain why you identify a person before giving care.
• Explain how to correctly identify a person.
• Describe the safety measures to prevent burns, poisoning, and suffocation.
• Identify the signs and causes of choking.
• Explain how to prevent equipment accidents.
• Explain how to handle hazardous substances.
• Describe safety measures for fire prevention and oxygen use.
• Explain what to do during a fire.
• Give examples of natural and human-made disasters.
• Explain how to report accidents and errors.
• Explain how to protect yourself from workplace violence.
• Describe your role in risk management.
• Perform the procedures described in this chapter.
Key terms
dementia The loss of cognitive and social function caused by changes in the brain
disaster A sudden catastrophic event in which people are injured and killed and property is destroyed
electrical shock When electrical current passes through the body
ground That which carries leaking electricity to the earth and away from an electrical item
hazard Any thing in the person’s setting that may cause injury or illness
hazardous substance Any chemical in the workplace that can cause harm
hemiplegia Paralysis on one side of the body
incident Any event that has harmed or could harm a resident, visitor, or staff member
paralysis Loss of muscle function, loss of sensation, or loss of both muscle function and sensation
paraplegia Paralysis in the legs and lower trunk
quadriplegia Paralysis in the arms, legs, and trunk; tetraplegia
suffocation When breathing stops from the lack of oxygen
tetraplegia See “quadriplegia”
workplace violence Violent acts (including assault and threat of assault) directed toward persons at work or while on duty
KEY ABBREVIATIONS
| AED | Automated external defibrillator |
| C | Centigrade |
| CMS | Centers for Medicare & Medicaid Services |
| CPR | Cardiopulmonary resuscitation |
| EMS | Emergency Medical Services |
| F | Fahrenheit |
| FBAO | Foreign-body airway obstruction |
| ID | Identification |
| MSDS | Material safety data sheet |
| OBRA | Omnibus Budget Reconciliation Act of 1987 |
| OSHA | Occupational Safety and Health Administration |
| PASS | Pull the safety pin, aim low, squeeze the lever, sweep back and forth |
Safety is a basic need. Residents are at great risk for accidents and falls. (See Chapter 13 for falls.) Some accidents and injuries cause death.
The health team must provide for safety. This includes you. Ordinary and sometimes extraordinary measures are needed to prevent accidents and keep residents safe. The goal is to decrease the person’s risk of accidents and injuries without limiting mobility and independence.
![]() The Omnibus Budget Reconciliation Act of 1987 (OBRA) requires that nursing centers follow safety policies and procedures. So do accrediting agency standards. The intent is to keep residents, visitors, and staff safe. Measures to protect residents must not interfere with their rights (Chapter 2).
The Omnibus Budget Reconciliation Act of 1987 (OBRA) requires that nursing centers follow safety policies and procedures. So do accrediting agency standards. The intent is to keep residents, visitors, and staff safe. Measures to protect residents must not interfere with their rights (Chapter 2).
Common sense and simple safety measures can prevent most accidents. You must protect residents, visitors, yourself, and co-workers. The safety measures in this chapter apply to nursing and everyday life. The care plan lists other safety measures for the person.
A safe setting
In a safe setting, a person has little risk of illness or injury. The person’s setting is free of hazards to the extent possible. A hazard is any thing in the person’s setting that may cause injury or illness.
The person feels safe and secure physically and mentally. The risk of infection, falls, burns, poisoning, and other injuries is low. Temperature and noise levels are comfortable. Smells are pleasant. There is enough room and light to move about safely. The person and the person’s property are safe from fire and intruders. The person is not afraid. He or she has few worries and concerns.
The person must receive the right care and treatment. The person is protected from falls, burns, poisoning, suffocation, and infection. To protect the person from harm, follow the person’s care plan. Also practice the safety measures in this chapter.
See Teamwork and Time Management: A Safe Setting.
Accident risk factors
Some people cannot protect themselves. They present dangers to themselves and others. They rely on others for safety. Know the factors that increase a person’s risk of accidents and injuries. Follow the person’s care plan to provide for safety.
• Age. Changes from aging increase the risk for falls and other injuries. Older persons have decreased strength and move slowly. Some are unsteady. Often balance is affected. These changes prevent quick and sudden movements to avoid dangers and prevent falls. Older persons also are less sensitive to heat and cold. They have poor vision, hearing problems, and a dulled sense of smell. Confusion, poor judgment, memory problems, and disorientation may occur (Chapter 44).
• Awareness of surroundings. People need to know their surroundings to protect themselves from injury. Coma is a state of being unaware of one’s surroundings and being unable to react or respond to people, places, or things. A coma can occur from illness or injury. The person in a coma relies on others for protection. Confused and disoriented persons may not understand what is happening to and around them.
See Residents With Dementia: Accident Risk Factors (Awareness of Surroundings).
Identifying the person
You will care for many people. Each has different treatments, therapies, and activity limits. You must give the right care to the right person. Life and health are threatened if the wrong care is given.
The person may receive an identification (ID) bracelet when admitted to the center (Fig. 12-1). The bracelet has the person’s name, room and bed number, birth date, age, doctor, and center name. Other identifying information may include the person’s ID number given by the center. Some centers include the person’s religion.

You use the bracelet to identify the person before giving care. The assignment sheet states what care to give. To identify the person:
• Compare identifying information on the assignment sheet with that on the ID bracelet (Fig. 12-2). Carefully check the information. Some people have the same first and last names. For example, John Smith is a very common name.

Alert and oriented residents may choose not to wear ID bracelets. This is noted on the person’s care plan. Follow center policy and the care plan to identify the person.
Some nursing centers have photo ID systems (Fig. 12-3). The person’s photo is taken on admission. Then it is placed in the person’s medical record. If your center uses such a system, learn to use it safely.
See Promoting Safety and Comfort: Identifying the Person.
Preventing burns
Burns are a leading cause of death among children and older persons. Smoking, spilled hot liquids, electrical items, and very hot water (hand sinks, tubs, showers) are some causes in nursing centers. Risk factors for burns in older persons are decreased skin thickness, decreased sensitivity to heat, reduced reaction time, decreased mobility, communication problems, confusion, and dementia.
Burn severity depends on water temperature and length of exposure (Table 12-1). The person’s condition also is a factor.
Table 12-1
Water Temperature and Length of Exposure for a Third Degree Burn
| Fahrenheit (F) | Centigrade (C) | Time Required for a Third Degree Burn to Occur |
| 155° F | 68° C | 1 second |
| 148° F | 64° C | 2 seconds |
| 140° F | 60° C | 5 seconds |
| 133° F | 56° C | 15 seconds |
| 127° F | 52° C | 1 minute |
| 124° F | 51° C | 3 minutes |
| 120° F | 48° C | 5 minutes |
| 100° F | 37° C | Usually a safe temperature for bathing |
Modified from Centers for Medicare & Medicaid Services: State operations manual, Baltimore, Md, April 10, 2009, U.S. Department of Health and Human Services.
The safety measures in Box 12-1 can prevent burns.
Preventing poisoning
Poisoning also is a health hazard and a major cause of death. Older persons are at risk. Drugs and household products are common poisons. Poisoning in adults may be from carelessness, confusion, or poor vision when reading labels. As a result, a person may take too much of a drug. Sometimes poisoning is a suicide attempt.
The measures in Box 12-2 can prevent poisoning.
Preventing suffocation
Suffocation is when breathing stops from the lack of oxygen. Death occurs if the person does not start breathing. Common causes include choking, drowning, inhaling gas or smoke, strangulation, and electrical shock (p. 141).
Carbon monoxide poisoning is another cause. Carbon monoxide is a colorless, odorless, and tasteless gas. It is produced by burning fuel. For example, motor vehicles, furnaces, gas water heaters, gas stoves, and gas dryers use fuel. These devices must be in good working order and used correctly. Otherwise, dangerous levels of carbon monoxide may result. Instead of breathing in oxygen, the person breathes in air filled with carbon monoxide. Headache, nausea, and dizziness are common. So are confusion, breathing problems, sleepiness, and cherry-pink skin. Death can occur.
Measures to prevent suffocation are listed in Box 12-3. Clear the airway if the person is choking.
Choking
Foreign bodies can obstruct the airway. This is called choking or foreign-body airway obstruction (FBAO). Air cannot pass through the air passages to the lungs. The body does not get enough oxygen. It can lead to cardiac arrest. Cardiac arrest is when the heart stops suddenly and without warning (Chapter 47).
Choking often occurs during eating. A large, poorly chewed piece of meat is the most common cause. Weakness, dentures that fit poorly, dysphagia (difficulty swallowing), and chronic illness are also causes.So are laughing and talking while eating and excessive alcohol intake.
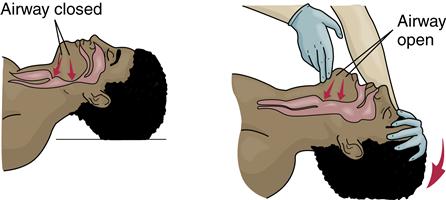
Unconscious persons can choke. Common causes are aspiration of vomitus and the tongue falling back into the airway. These also occur during cardiac arrest.
Foreign bodies can cause mild or severe airway obstruction. With mild airway obstruction, some air moves in and out of the lungs. The person is conscious and usually can speak. Often forceful coughing can remove the object. Breathing may sound like wheezing between coughs. For mild airway obstruction:
Difficulty breathing occurs with severe airway obstruction. Air does not move in and out of the lungs. The person may not be able to breathe, speak, or cough. If able to cough, the cough is of poor quality. When the person tries to inhale, there is no noise or a high-pitched noise. The person may appear pale and cyanotic (bluish color).
The conscious person clutches at the throat (Fig. 12-4). Clutching at the throat is often called the “universal sign of choking.” The conscious person is very frightened. If the obstruction is not removed, the person will die. Severe airway obstruction is an emergency.

 Relieving choking
Relieving choking
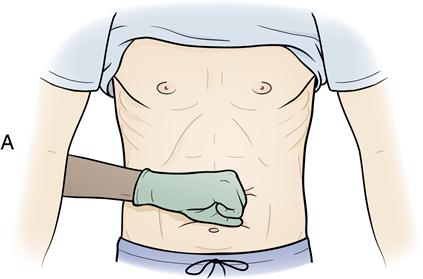
Abdominal thrusts are used to relieve severe airway obstruction. Abdominal thrusts are quick, upward thrusts to the abdomen. They force air out of the lungs and create an artificial cough. They are done to try to expel the foreign body from the airway.
Abdominal thrusts are not used for very obese persons or pregnant women. Chest thrusts are used (p. 140).
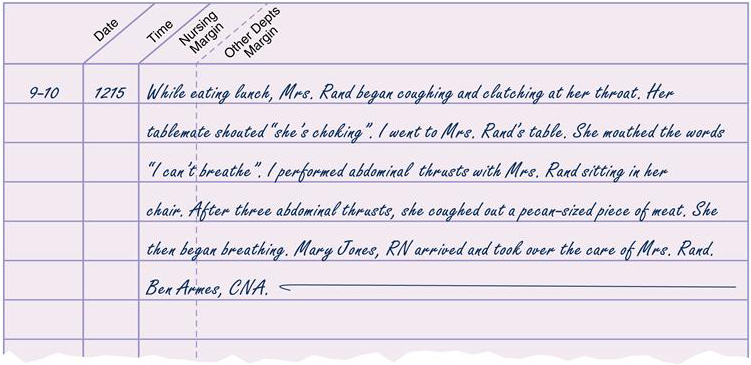
You may observe a person choking. And you may perform emergency measures to relieve choking. Report and record what happened, what you did, and the person’s response (Fig. 12-5).
Relief of choking occurs when the foreign body is removed. Or it occurs when you feel air move and see the chest rise and fall when giving rescue breaths. The person may still be unresponsive.
Self-administered abdominal thrusts.
You may choke when by yourself. Perform abdominal thrusts to relieve the obstructed airway.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree