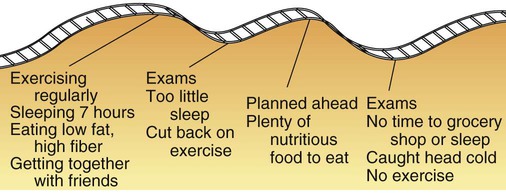
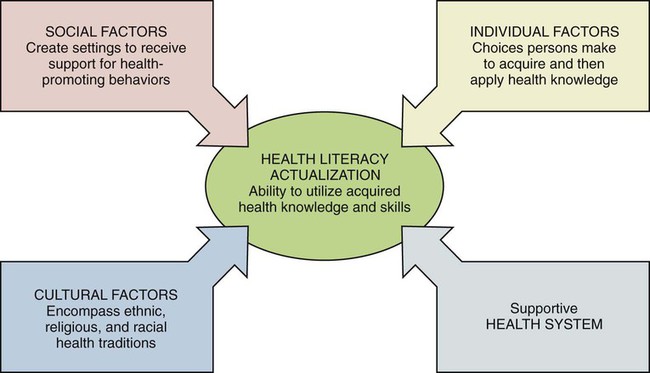
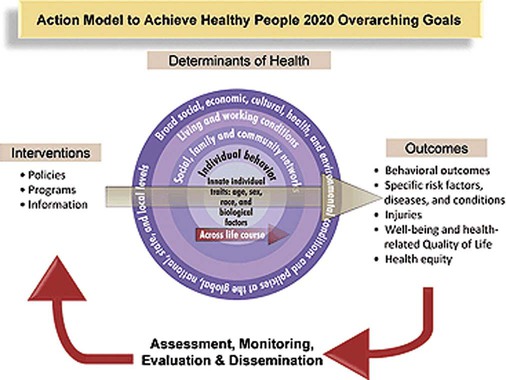
Nutrition is a hot topic that generates interest easily; everyone seems to have opinions about what to eat and concerns about their own eating styles. The public is flooded with information and techniques related to health promotion through nutrition. Health literacy is the ability to acquire and comprehend basic health concepts, such as nutrition, and apply them to one’s own health decisions.1 Health literacy allows for education to be most effective, resulting in behavior changes. Nurses, through formal, nonformal, and informal educational interactions, can introduce knowledge and strategies for personal lifestyle choices that consider the health context of patients’ lives.2 Health context takes into account the influence of cultural, social, and individual factors on the acquisition of health literacy. Cultural factors may encompass ethnic, religious, and racial traditions surrounding health issues. Social factors create the settings for which members of a community receive support or lack support for health-promoting behaviors. Individual factors reflect on the choices people make regarding willingness to acquire and then apply health knowledge. Health literacy actualization means being able to use acquired health knowledge and skills. The extent to which this occurs within health care settings is influenced by the level to which health care providers are supportive of literate health populations seeking greater involvement in their health care (Figure 1-1). One of the first expanded definitions of health was provided by the World Health Organization (WHO): “Health is a state of complete physical, mental, and social well-being and not merely the absence of disease and infirmity.”3 Although this definition addresses the concern that health is more than just the absence of disease, health is presented as a static concept that individuals achieve. A more expanded definition of health was presented by Rene Dubos, biologist and philosopher, who wrote, “Health is a quality of life involving social, emotional, mental, spiritual, and biologic fitness on the part of the individual, which results from adaptations to the environment.”4 This view leads to our present understanding of health as a complex concept best represented by physical and psychologic dimensions, as follows: • Physical health: The efficiency of the body to function appropriately, to maintain immunity to disease, and to meet daily energy requirements • Intellectual health: The use of intellectual abilities to learn and to adapt to changes in one’s environment • Emotional health: The capacity to easily express or suppress emotions appropriately • Social health: The ability to interact with people in an acceptable manner and sustain relationships with family members, friends, and colleagues • Spiritual health: The cultural beliefs that give purpose to human existence, found through faith in the teachings of organized religions, in an understanding of nature or science, or in an acceptance of the humanistic view of life Health promotion consists of strategies used to increase the level of the health of individuals, families, groups, and communities. In community and occupational health settings, health promotion strategies implemented by nurses often focus on lifestyle changes that will lead to new, positive health behaviors. Development of positive behaviors may depend on knowledge, techniques, and community supports, as follows (see the Teaching Tool box Literacy and Health): • Knowledge: Learning new information about the benefits or risks of health-related behaviors • Techniques: Applying new knowledge to everyday activities; developing ways to modify current lifestyles • Community supports: Availability of environmental or regulatory measures to support new health-promoting behaviors within a social context For more than 30 years, national health targets have been set. In 1979 the first initiative, the Surgeon General’s report titled Healthy People, laid out life-stage targets that continue to be tracked today. Since then, health targets have been updated every 10 years through collaboration among the government, voluntary and professional health associations, businesses, and individuals under the direction of the secretary of the Department of Health and Human Services. The objectives focus on the decisions and policies that affect prevention efforts and create a standard from which to later assess the performance of meeting these goals. In addition, the interrelatedness of the health of communities and individuals is emphasized. The health status of an individual is dependent on the health supports accessible within the community. (This theme is also discussed in Chapter 2 under the heading “Community Nutrition.”) HP2020 is guided by a framework based on the vision of “a society in which all people live long, healthy lives.”5 The mission is “to improve health through strengthening policy and practice.”5 Four overarching goals present pathways to achieve the vision and mission. Details of the HP2020 framework are listed in Box 1-1. The Action Model to Achieve Healthy People 2020 Overarching Goals (Figure 1-2) suggests priorities for change based on determinants of health such as living and working conditions, as well as individual behaviors as affected by the traits of individuals such as age, sex, race, and biological factors. The implementations of strategies are assessed by their outcomes. The outcomes are then evaluated, distributed, and used to create additional interventions.5 These actions will bring us as a nation closer to achieving the goals by 2020. Hectic contemporary schedules may seem to interfere with efforts to achieve wellness. The aim is to strive for wellness even if the path may seem more like a roller coaster than a smooth uphill climb (Figure 1-3). At times, clients may falter in their efforts, but the key is to renew positive behaviors as soon as possible.
Wellness Nutrition
![]() http://evolve.elsevier.com/Grodner/foundations/
http://evolve.elsevier.com/Grodner/foundations/ ![]() Nutrition Concepts Online
Nutrition Concepts Online
Role in Wellness
Definition of Health
Health Promotion
Role of Nutrition
Definition of Wellness
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree