Nutrition
Objectives
• Explain the importance of a balance between energy intake and energy requirements.
• List the end products of carbohydrate, protein, and fat metabolism.
• Explain the significance of saturated, unsaturated, and polyunsaturated fats.
• Describe food guidelines and discuss their value in planning meals for good nutrition.
• List the current dietary guidelines for the general population.
• Explain the variance in nutritional requirements throughout growth and development.
• Discuss the major methods of nutritional assessment.
• Identify three major nutritional problems and describe patients at risk.
• Establish a plan of care to meet the nutritional needs of a patient.
• Describe the procedure for initiating and maintaining enteral feedings.
• Describe the methods to avoid complications of enteral feedings.
• Describe the methods for avoiding complications of parenteral nutrition.
• Discuss medical nutrition therapy in relation to three medical conditions.
• Discuss diet counseling and patient teaching in relation to patient expectations.
Key Terms
Amino acid, p. 997
Anabolism, p. 1000
Anorexia, p. 1015
Anorexia nervosa, p. 1003
Anthropometry, p. 1009
Basal metabolic rate (BMR), p. 997
Body mass index (BMI), p. 1009
Bulimia nervosa, p. 1003
Carbohydrates, p. 997
Catabolism, p. 1000
Chyme, p. 1000
Daily values, p. 1001
Dietary reference intakes (DRIs), p. 1001
Dispensable amino acids, p. 997
Dysphagia, p. 1010
Enteral nutrition (EN), p. 1018
Enzymes, p. 998
Fat-soluble vitamins, p. 998
Fatty acids, p. 998
Fiber, p. 997
Food security, p. 996
Gluconeogenesis, p. 1000
Glycogenesis, p. 1000
Glycogenolysis, p. 1000
Hypervitaminosis, p. 998
Ideal body weight (IBW), p. 1009
Indispensable amino acids, p. 997
Intravenous fat emulsions, p. 1021
Ketones, p. 1000
Kilocalorie (kcal), p. 997
Lipids, p. 998
Macrominerals, p. 998
Malabsorption, p. 1024
Malnutrition, p. 1007
Medical nutrition therapy (MNT), p. 1024
Metabolism, p. 1000
Minerals, p. 998
Monounsaturated fatty acids, p. 998
Nitrogen balance, p. 998
Nutrient density, p. 997
Nutrients, p. 997
Parenteral nutrition (PN), p. 1021
Peristalsis, p. 999
Polyunsaturated fatty acids, p. 998
Resting energy expenditure (REE), p. 997
Saccharides, p. 997
Saturated fatty acids, p. 998
Simple carbohydrates, p. 997
Trace elements, p. 998
Triglycerides, p. 998
Unsaturated fatty acids, p. 998
Vegetarianism, p. 1006
Vitamins, p. 998
Water-soluble vitamins, p. 998
![]()
Nutrition is a basic component of health and is essential for normal growth and development, tissue maintenance and repair, cellular metabolism, and organ function. The human body needs an adequate supply of nutrients for essential functions of cells. Food security is critical for all members of a household. This means that all household members have access to sufficient, safe, and nutritious food to maintain a healthy lifestyle; sufficient food is available on a consistent basis; and the household has resources to obtain appropriate food for a nutritious diet. Food also holds symbolic meaning. Giving or taking food is part of ceremonies, social gatherings, holiday traditions, religious events, the celebration of birth, and the mourning of death. The difficulty of the decision to withdraw food in a terminal illness, even in the form of intravenous (IV) nutrients, is a testament to the symbolic power of food and feeding.
Florence Nightingale understood the importance of nutrition, stressing a nurse’s role in the science and art of feeding during the mid-1800s (Dossey, 1999). Since then the nurse’s role in nutrition and diet therapy has changed. Medical nutrition therapy (MNT) uses nutrition therapy and counseling to manage diseases (American Dietetic Association, 2010b). In some illnesses such as type 1 diabetes mellitus (DM) or mild hypertension, diet therapy is often the major treatment for disease control (ADA, 2008; American Heart Association, 2010). Other conditions such as severe inflammatory bowel disease require specialized nutrition support such as enteral nutrition (EN) or parenteral nutrition (PN). Current standards of care promote optimal nutrition in all patients (American Heart Association, 2010; ACS, 2011).
The U.S. Department of Health and Human Services (USDHHS) and the Public Health Service established nutritional goals and objectives for Healthy People 2020 (USDHHS, 2010). Healthy People 2020 is the United States’ contribution to the “Health for All” strategy of the World Health Organization (WHO, 2010). Healthy People 2020 (Box 44-1) continues the objectives initiated in Healthy People 2000 and Healthy People 2010, with overall goals of promoting health and reducing chronic disease. All nutrition-related objectives include baseline data from which progress is measured. The challenge remains to motivate consumers to put these dietary recommendations into practice.
Scientific Knowledge Base
Nutrients: The Biochemical Units of Nutrition
The body requires fuel to provide energy for cellular metabolism and repair, organ function, growth, and body movement. The basal metabolic rate (BMR) is the energy needed to maintain life-sustaining activities (breathing, circulation, heart rate, and temperature) for a specific period of time at rest. Factors such as age, body mass, gender, fever, starvation, menstruation, illness, injury, infection, activity level, or thyroid function affect energy requirements. The resting energy expenditure (REE), or resting metabolic rate, is the amount of energy that an individual needs to consume over a 24-hour period for the body to maintain all of its internal working activities while at rest. Factors that affect metabolism include illness, pregnancy, lactation, and activity level.
In general, when energy requirements are completely met by kilocalorie (kcal) intake in food, weight does not change. When the kilocalories ingested exceed a person’s energy demands, the individual gains weight. If the kilocalories ingested fail to meet a person’s energy requirements, the individual loses weight.
Nutrients are the elements necessary for the normal function of numerous body processes. Energy needs are met from a variety of nutrients: carbohydrates, proteins, fats, water, vitamins, and minerals. Food is sometimes described according to its nutrient density (i.e., the proportion of essential nutrients to the number of kilocalories). High–nutrient dense foods such as fruits and vegetables provide a large number of nutrients in relationship to kilocalories. Low–nutrient dense foods such as alcohol or sugar are high in kilocalories but nutrient poor.
Carbohydrates.
Carbohydrates, composed of carbon, hydrogen, and oxygen, are the main source of energy in the diet. Each gram of carbohydrate produces 4 kcal/g and serves as the main source of fuel (glucose) for the brain, skeletal muscles during exercise, erythrocyte and leukocyte production, and cell function of the renal medulla. People obtain carbohydrates primarily from plant foods, except for lactose (milk sugar). They are classified according to their carbohydrate units, or saccharides.
Monosaccharides such as glucose (dextrose) or fructose cannot be broken down into a more basic carbohydrate unit. Disaccharides such as sucrose, lactose, and maltose are composed of two monosaccharides and water. Both monosaccharides and disaccharides are classified as simple carbohydrates and are found primarily in sugars. Polysaccharides such as glycogen are made up of many carbohydrate units (i.e., complex carbohydrates). They are insoluble in water and digested to varying degrees. Starches are polysaccharides.
The body is unable to digest some polysaccharides because humans do not have enzymes capable of breaking them down. Fiber is a polysaccharide that is the structural part of plants that is not broken down by the human digestive enzymes. Because fiber is not broken down, it does not contribute calories to the diet. Insoluble fibers are not digestible and include cellulose, hemicellulose, and lignin. Soluble fibers dissolve in water and include barley, cereal grains, cornmeal, and oats.
Proteins.
Proteins provide a source of energy (4 kcal/g), and they are essential for synthesis (building) of body tissue in growth, maintenance, and repair. Collagen, hormones, enzymes, immune cells, deoxyribonucleic acid (DNA), and ribonucleic acid (RNA) are all made of protein. In addition, blood clotting, fluid regulation, and acid-base balance require proteins. These proteins transport nutrients and many drugs in the blood. Ingestion of proteins maintains nitrogen balance.
The simplest form of protein is the amino acid, which is made up of hydrogen, oxygen, carbon, and nitrogen. The body does not synthesize indispensable amino acids; thus these need to be provided in the diet. Examples of indispensable amino acids are histidine, lysine, and phenylalanine. The body synthesizes dispensable amino acids. Examples of amino acids synthesized in the body are alanine, asparagine, and glutamic acid. Amino acids can link together. Albumin and insulin are simple proteins because they contain only amino acids or their derivatives. The combination of a simple protein with a nonprotein substance produces a complex protein such as lipoprotein, formed by a combination of a lipid and a simple protein.
A complete protein, also called a high-quality protein, contains all essential amino acids in sufficient quantity to support growth and maintain nitrogen balance. Examples of foods that contain complete proteins are fish, chicken, soybeans, turkey, and cheese. Incomplete proteins are missing one or more of the nine indispensable amino acids and include cereals, legumes (beans, peas), and vegetables. Complementary proteins are pairs of incomplete proteins that, when combined, supply the total amount of protein provided by complete protein sources.
Nitrogen balance is achieved when the intake and output of nitrogen are equal. When the intake of nitrogen is greater than the output, the body is in positive nitrogen balance. Positive nitrogen balance is required for growth, normal pregnancy, maintenance of lean muscle mass and vital organs, and wound healing. The body uses nitrogen to build, repair, and replace body tissues. Negative nitrogen balance occurs when the body loses more nitrogen than it gains (e.g., with infection, burns, fever, starvation, head injury, and trauma). The increased nitrogen loss is the result of body tissue destruction or loss of nitrogen-containing body fluids. Nutrition during this period needs to provide nutrients to put patients into positive balance for healing.
Protein provides energy; however, because of the essential role of protein in growth, maintenance, and repair, a diet needs to provide adequate kilocalories from nonprotein sources. When there is sufficient carbohydrate in the diet to meet the energy needs of the body, protein is spared as an energy source.
Fats.
Fats (lipids) are the most calorie-dense nutrient, providing 9 kcal/g. Fats are composed of triglycerides and fatty acids. Triglycerides circulate in the blood and are composed of three fatty acids attached to a glycerol. Fatty acids are composed of chains of carbon and hydrogen atoms with an acid group on one end of the chain and a methyl group at the other. Fatty acids can be saturated, in which each carbon in the chain has two attached hydrogen atoms; or unsaturated, in which an unequal number of hydrogen atoms are attached and the carbon atoms attach to each other with a double bond. Monounsaturated fatty acids have one double bond, whereas polyunsaturated fatty acids have two or more double carbon bonds. The various types of fatty acids have significance for health and the incidence of disease and are referred to in dietary guidelines.
Fatty acids are also classified as essential or nonessential. Linoleic acid, an unsaturated fatty acid, is the only essential fatty acid in humans. Linolenic acid and arachidonic acid (also unsaturated fatty acids) are important for metabolic processes but are manufactured by the body when linoleic acid is available. Deficiency occurs when fat intake falls below 10% of daily nutrition. Most animal fats have high proportions of saturated fatty acids, whereas vegetable fats have higher amounts of unsaturated and polyunsaturated fatty acids.
Water.
Water is critical because cell function depends on a fluid environment. Water makes up 60% to 70% of total body weight. The percent of total body water is greater for lean people than obese people because muscle contains more water than any other tissue except blood. Infants have the greatest percentage of total body water, and older people have the least. When deprived of water, a person cannot survive for more than a few days.
An individual meets fluid needs by drinking liquids and eating solid foods high in water content such as fresh fruits and vegetables. Water is also produced during digestion when food is oxidized. In a healthy individual fluid intake from all sources equals fluid output through elimination, respiration, and sweating (see Chapters 41 and 45). An ill person has an increased need for fluid (e.g., with fever or gastrointestinal [GI] losses). By contrast, he or she also has a decreased ability to excrete fluid (e.g., with cardiopulmonary or renal disease), which often leads to the need for fluid restriction.
Vitamins.
Vitamins are organic substances present in small amounts in foods that are essential to normal metabolism. They are chemicals that act as catalysts in biochemical reactions. When there is enough of any specific vitamin to meet the body’s catalytic demands, the rest of the vitamin supply acts as a free chemical and is often toxic to the body. Certain vitamins are currently of interest in their role as antioxidants. These vitamins neutralize substances called free radicals, which produce oxidative damage to body cells and tissues. Researchers think that oxidative damage increases a person’s risk for various cancers. These vitamins include betacarotene and vitamins A, C, and E (Nix, 2009).
The body is unable to synthesize vitamins in the required amounts and depends on dietary intake. Vitamin content is usually highest in fresh foods that are used quickly after minimal exposure to heat, air, or water. Vitamins are classified as fat soluble and water soluble.
Fat-Soluble Vitamins.
The fat-soluble vitamins (A, D, E, and K) are stored in the fatty compartments of the body. With the exception of vitamin D, people acquire vitamins through dietary intake. Hypervitaminosis of fat-soluble vitamins results from megadoses (intentional or unintentional) of supplemental vitamins, excessive amounts in fortified food, and large intake of fish oils.
Water-Soluble Vitamins.
The water-soluble vitamins are vitamin C and the B complex (which is eight vitamins). The body does not store water-soluble vitamins; thus they need to be provided in daily food intake. Water-soluble vitamins absorb easily from the GI tract. Although they are not stored, toxicity can still occur.
Minerals.
Minerals are inorganic elements essential to the body as catalysts in biochemical reactions. They are classified as macrominerals when the daily requirement is 100 mg or more and microminerals or trace elements when less than 100 mg is needed daily. Macrominerals help to balance the pH of the body, and specific amounts are necessary in the blood and cells to promote acid-base balance. Interactions occur among trace minerals. For example, excess of one trace mineral sometimes causes deficiency of another. Selenium is a trace element that also has antioxidant properties. Silicon, vanadium, nickel, tin, cadmium, arsenic, aluminum, and boron play an unidentified role in nutrition. Arsenic, aluminum, and cadmium have toxic effects.
Anatomy and Physiology of the Digestive System
Digestion.
Digestion of food is the mechanical breakdown that results from chewing, churning, and mixing with fluid and chemical reactions in which food is reduced to its simplest form. Each part of the GI system has an important digestive or absorptive function (Fig. 44-1). Enzymes are the proteinlike substances that act as catalysts to speed up chemical reactions. They are an essential part of the chemistry of digestion.
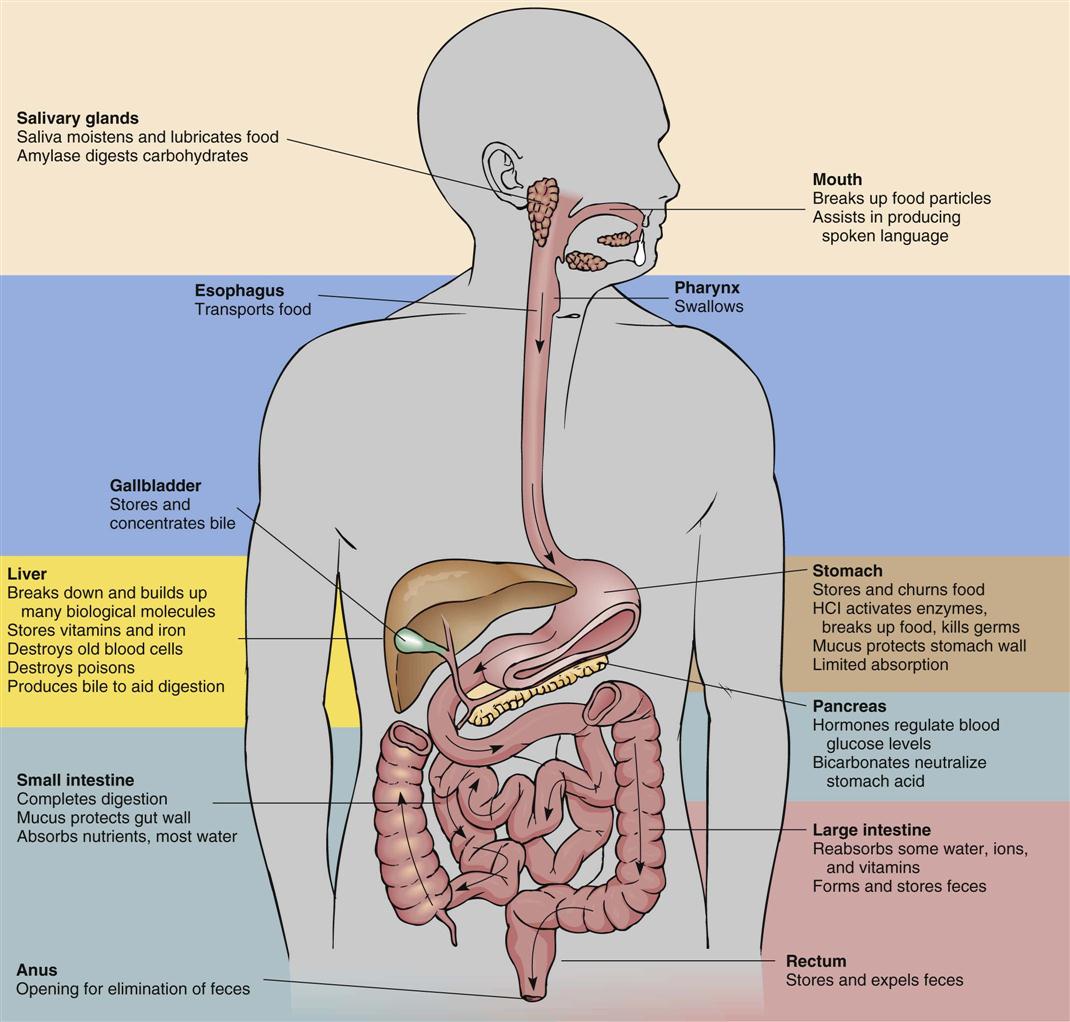
Most enzymes have one specific function. Each enzyme works best at a specific pH. For example, the enzyme amylase in the saliva breaks down starches into sugars. The secretions of the GI tract have very different pH levels. For example, saliva is relatively neutral, gastric juice is highly acidic, and the secretions of the small intestine are alkaline.
The mechanical, chemical, and hormonal activities of digestion are interdependent. Enzyme activity depends on the mechanical breakdown of food to increase its surface area for chemical action. Hormones regulate the flow of digestive secretions needed for enzyme supply. Physical, chemical, and hormonal factors regulate the secretion of digestive juices and the motility of the GI tract. Nerve stimulation from the parasympathetic nervous system (e.g., the vagus nerve) increases GI tract action.
Digestion begins in the mouth, where chewing mechanically breaks down food. The food mixes with saliva, which contains ptyalin (salivary amylase), an enzyme that acts on cooked starch to begin its conversion to maltose. The longer an individual chews food, the more starch digestion occurs in the mouth. Proteins and fats are broken down physically but remain unchanged chemically because enzymes in the mouth do not react with these nutrients. Chewing reduces food particles to a size suitable for swallowing, and saliva provides lubrication to further ease swallowing of the food. The epiglottis is a flap of skin that closes over the trachea as a person swallows to prevent aspiration. Swallowed food enters the esophagus, and wavelike muscular contractions (peristalsis) move the food to the base of the esophagus, above the cardiac sphincter. Pressure from a bolus of food at the cardiac sphincter causes it to relax, allowing the food to enter the fundus, or uppermost portion, of the stomach.
The chief cells in the stomach secrete pepsinogen; and the pyloric glands secrete gastrin, a hormone that triggers parietal cells to secrete hydrochloric acid (HCl). The parietal cells also secrete HCl and intrinsic factor (IF), which is necessary for absorption of vitamin B12 in the ileum. HCl turns pepsinogen into pepsin, a protein-splitting enzyme. The body produces gastric lipase and amylase to begin fat and starch digestion, respectively. A thick layer of mucus protects the lining of the stomach from autodigestion. Alcohol and aspirin are two substances directly absorbed through the lining of the stomach. The stomach acts as a reservoir where food remains for approximately 3 hours, with a range of 1 to 7 hours.
Food leaves the antrum, or distal stomach, through the pyloric sphincter and enters the duodenum. Food is now an acidic, liquefied mass called chyme. Chyme flows into the duodenum and quickly mixes with bile, intestinal juices, and pancreatic secretions. The small intestine secretes the hormones secretin and cholecystokinin (CCK). Secretin activates release of bicarbonate from the pancreas, raising the pH of chyme. CCK inhibits further gastrin secretion and initiates release of additional digestive enzymes from the pancreas and gallbladder.
Bile is manufactured in the liver and concentrated and stored in the gallbladder. It acts as a detergent because it emulsifies fat to permit enzyme action while suspending fatty acids in solution. Pancreatic secretions contain six enzymes: amylase to digest starch; lipase to break down emulsified fats; and trypsin, elastase, chymotrypsin, and carboxypeptidase to break down proteins.
Peristalsis continues in the small intestine, mixing the secretions with chyme. The mixture becomes increasingly alkaline, inhibiting the action of the gastric enzymes and promoting the action of the duodenal secretions. Epithelial cells in the small intestinal villi secrete enzymes (e.g., sucrase, lactase, maltase, lipase, and peptidase) to facilitate digestion. The major portion of digestion occurs in the small intestine, producing glucose, fructose, and galactose from carbohydrates; amino acids and dipeptides from proteins; and fatty acids, glycerides, and glycerol from lipids. Peristalsis usually takes approximately 5 hours to pass food through the small intestine.
Absorption.
The small intestine is the primary absorption site for nutrients. It is lined with fingerlike projections called villi. Villi increase the surface area available for absorption. The body absorbs nutrients by means of passive diffusion, osmosis, active transport, and pinocytosis (Table 44-1).
TABLE 44-1
Mechanisms for Intestinal Absorption of Nutrients
| MECHANISM | DEFINITION |
| Active transport | An energy-dependent process whereby particles move from an area of greater concentration to an area of lesser concentration. A special “carrier” moves the particle across the cell membrane. |
| Passive diffusion | The force by which particles move outward from an area of greater concentration to lesser concentration. The particles do not need a special “carrier” to move outward in all directions. |
| Osmosis | Movement of water through a membrane that separates solutions of different concentrations. Water moves to equalize the concentration pressures on both sides of the membrane. |
| Pinocytosis | Engulfing of large molecules of nutrients by the absorbing cell when the molecule attaches to the absorbing cell membrane. |
Data from Nix S: Williams’ basic nutrition and diet therapy, ed 13, St Louis, 2009, Mosby.
Carbohydrates, protein, minerals, and water-soluble vitamins are absorbed by the small intestine, processed in the liver, and released into the portal vein circulation. Fatty acids are absorbed in the lymphatic circulatory systems through lacteal ducts at the center of each microvilli in the small intestine.
Approximately 85% to 90% of water is absorbed in the small intestine (Huether et al., 2008). Approximately 8.5 L of GI secretions and 1.5 L of oral intake are managed daily within the GI tract. The small intestine resorbs 9.5 L, and the colon absorbs approximately 0.4 L. The remaining 0.1 L is eliminated in feces. In addition, electrolytes and minerals are absorbed in the colon, and bacteria synthesize vitamin K and some B-complex vitamins. Finally, feces are formed for elimination.
Metabolism and Storage of Nutrients.
Metabolism refers to all of the biochemical reactions within the cells of the body. Metabolic processes are anabolic (building) or catabolic (breaking down). Anabolism is the building of more complex biochemical substances by synthesis of nutrients. Anabolism occurs when an individual adds lean muscle through diet and exercise. Amino acids are anabolized into tissues, hormones, and enzymes. Normal metabolism and anabolism are physiologically possible when the body is in positive nitrogen balance. Catabolism is the breakdown of biochemical substances into simpler substances and occurs during physiological states of negative nitrogen balance. Starvation is an example of catabolism when wasting of body tissues occurs.
Nutrients absorbed in the intestines, including water, are transported through the circulatory system to the body tissues. Through the chemical changes of metabolism, the body converts nutrients into a number of required substances. Carbohydrates, protein, and fat are metabolized to produce chemical energy and maintain a balance between anabolism and catabolism. To carry out the work of the body, the chemical energy produced by metabolism converts to other types of energy by different tissues. Muscle contraction involves mechanical energy, nervous system function involves electrical energy, and the mechanisms of heat production involve thermal energy.
Some of the nutrients required by the body are stored in tissues. The major form of body reserve energy is fat, stored as adipose tissue. Protein is stored in muscle mass. When the energy requirements of the body exceed the energy supplied by ingested nutrients, stored energy is used. Monoglycerides from the digested portion of fats are converted to glucose by gluconeogenesis. Amino acids are also converted to fat and stored or catabolized into energy through gluconeogenesis. All body cells except red blood cells and neurons oxidize fatty acids into ketones for energy when dietary carbohydrates (glucose) are not adequate. Glycogen, synthesized from glucose, provides energy during brief periods of fasting (e.g., during sleep). It is stored in small reserves in liver and muscle tissue. Nutrient metabolism consists of three main processes:
Elimination.
Chyme moves by peristaltic action through the ileocecal valve into the large intestine, where it becomes feces (see Chapter 46). Water absorbs in the mucosa as feces move toward the rectum. The longer the material stays in the large intestine, the more water is absorbed, causing the feces to become firmer. Exercise and fiber stimulate peristalsis, and water maintains consistency. Feces contain cellulose and similar indigestible substances, sloughed epithelial cells from the GI tract, digestive secretions, water, and microbes.
Dietary Guidelines
Dietary Reference Intakes.
Dietary reference intakes (DRIs) present evidence-based criteria for an acceptable range of amounts of vitamins and nutrients for each gender and age-group (Institute of Medicine, 2006). There are four components to the DRIs. The estimated average requirement (EAR) is the recommended amount of a nutrient that appears sufficient to maintain a specific body function for 50% of the population based on age and gender. The recommended dietary allowance (RDA) is the average needs of 98% of the population, not the exact needs of the individual. The adequate intake (AI) is the suggested intake for individuals based on observed or experimentally determined estimates of nutrient intakes and is used when there is not enough evidence to set the RDA. The tolerable upper intake level (UL) is the highest level that likely poses no risk of adverse health events. It is not a recommended level of intake (Tolerable upper level intake, 2010).
Food Guidelines.
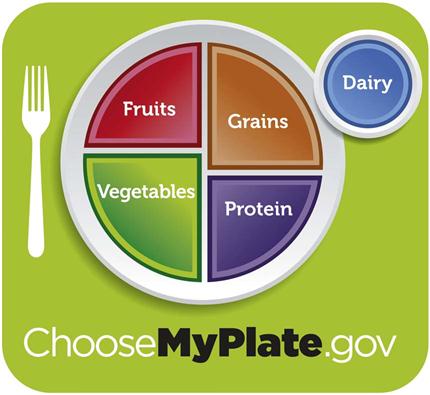
The U.S. Department of Agriculture (USDA) and the U.S. Department of Health and Human Services (USDHHS) published the Dietary Guidelines for Americans 2010 and provide average daily consumption guidelines for the five food groups: grains, vegetables, fruits, dairy products, and meats (Box 44-2). These guidelines are for Americans over the age of 2 years. As a nurse, consider the food preferences of patients from different racial and ethnic groups, vegetarians, and others when planning diets. The ChooseMyPlate program was developed by the U.S. Department of Agriculture to replace the My Food Pyramid program. ChooseMyPlate provides a basic guide for making food choices for a healthy lifestyle (Fig. 44-2). The ChooseMyPlate program includes guidelines for balancing calories; decreasing portion size; increasing healthy foods; increasing water consumption; and decreasing fats, sodium, and sugars (USDA, 2011a).
Daily Values.
The Food and Drug Administration (FDA) created daily values for food labels in response to the 1990 Nutrition Labeling and Education Act (NLEA). The FDA first established two sets of reference values. The referenced daily intakes (RDIs) are the first set, comprising protein, vitamins, and minerals based on the RDA. The daily reference values (DRVs) make up the second set and consist of nutrients such as total fat, saturated fat, cholesterol, carbohydrates, fiber, sodium, and potassium. Combined, both sets make up the daily values used on food labels (USFDA, 2008). Daily values did not replace RDAs but provided a separate, more understandable format for the public. Daily values are based on percentages of a diet consisting of 2000 kcal/day for adults and children 4 years or older.
Nursing Knowledge Base
Sociological, cultural, psychological, and emotional factors are associated with eating and drinking in all societies. Holidays and events are celebrated with food, food is brought to those who are grieving, and food is used for medicinal purposes. It is incorporated into family traditions and rituals and is often associated with eating behaviors. You need to understand patients’ values, beliefs, and attitudes about food and how these values affect food purchase, preparation, and intake to affect eating patterns.
Nutritional requirements depend on many factors. Individual caloric and nutrient requirements vary by stage of development, body composition, activity levels, pregnancy and lactation, and the presence of disease. Registered dietitians (RDs) use predictive equations that take into account some of these factors to estimate patients’ nutritional requirements.
Factors Influencing Nutrition
Environmental Factors.
Environmental factors beyond the control of individuals contribute to the development of obesity. Obesity is an epidemic in the United States. The prevalence of obesity in adults has doubled since 1980, with 33% of adults in the United States overweight, 34% obese, and 6 % extremely obese (body mass index [BMI] ≥40) (Khan et al., 2009). Proposed contributing factors are sedentary lifestyle, work schedules, and poor meal choices often related to the increasing frequency of eating away from home and eating fast food (Kruskall, 2006). The likelihood of healthy eating and participation in exercise or other activities of healthy living is limited by environmental factors. Lack of access to full-service grocery stores, high cost of healthy food, widespread availability of less healthy foods in fast-food restaurants, widespread advertising of less healthy food, and lack of access to safe places to play and exercise are environmental factors that contribute to obesity (Khan et al., 2009).
Developmental Needs
Infants Through School-Age.
Rapid growth and high protein, vitamin, mineral, and energy requirements mark the developmental stage of infancy. The average birth weight of an American baby is 3.2 to 3.4 kg (7 to  pounds). An infant usually doubles birth weight at 4 to 5 months and triples it at 1 year. Infants need an energy intake of approximately 90 to 110 kcal/kg of body weight, with premature infants needing 105 to 130 kcal/kg per day (Nix, 2009). Commercial formulas and human breast milk both provide approximately 20 kcal/oz. A full-term newborn is able to digest and absorb simple carbohydrates, proteins, and a moderate amount of emulsified fat. Infants need about 100 to 120 mL/kg/day of fluid because a large portion of total body weight is water.
pounds). An infant usually doubles birth weight at 4 to 5 months and triples it at 1 year. Infants need an energy intake of approximately 90 to 110 kcal/kg of body weight, with premature infants needing 105 to 130 kcal/kg per day (Nix, 2009). Commercial formulas and human breast milk both provide approximately 20 kcal/oz. A full-term newborn is able to digest and absorb simple carbohydrates, proteins, and a moderate amount of emulsified fat. Infants need about 100 to 120 mL/kg/day of fluid because a large portion of total body weight is water.
Breastfeeding.
The American Dietetic Association strongly supports exclusive breastfeeding for the first 6 months of life and breastfeeding with complementary foods from 6 to 12 months (American Dietetic Association, 2009). Breastfeeding has multiple benefits for both infant and mother, including fewer food allergies and intolerances; fewer infant infections; easier digestion; convenience, availability, and freshness; temperature always correct; economical because it is less expensive than formula; and increased time for mother and infant interaction.
Formula.
Infant formulas contain the approximate nutrient composition of human milk. Protein in the formula is typically whey, soy, cow’s milk base, casein hydrolysate, or elemental amino acids. The American Academy of Pediatrics sets standards for the level of nutrients in infant formulas. Soy protein–based formulas are used for infants allergic or intolerant to cow’s milk (Nix, 2009).
Infants should not have regular cow’s milk during the first year of life. It is too concentrated for an infant’s kidneys to manage, increases the risk of milk product allergies, and is a poor source of iron and vitamins C and E (Nix, 2009). Honey and corn syrup are potential sources of botulism toxin and should not be used in an infant’s diet. This toxin is potentially fatal in children under 1 year of age (Nix, 2009).
Introduction to Solid Food.
Breast milk or formula provides sufficient nutrition for the first 4 to 6 months of life. The development of fine-motor skills of the hand and fingers parallels an infant’s interest in food and self-feeding. Iron-fortified cereals are typically the first semisolid food to be introduced. For infants 4 to 11 months, cereals are the most important nonmilk source of protein (Fox et al., 2006).
The addition of foods to an infant’s diet is governed by an infant’s nutrient needs, physical readiness to handle different forms of foods, and the need to detect and control allergic reactions. Foods such as wheat, egg white, nuts, citrus juice, and chocolate have a high incidence of allergies and should be added late (Nix, 2009). Caregivers should introduce new foods one at a time, approximately 4 to 7 days apart to identify allergies. It is best to introduce new foods before milk or other foods to avoid satiety (Hockenberry and Wilson, 2011).
The growth rate slows during toddler years (1 to 3 years). A toddler needs fewer kilocalories but an increased amount of protein in relation to body weight; consequently appetite often decreases at 18 months of age. Toddlers exhibit strong food preferences and become picky eaters. Small frequent meals consisting of breakfast, lunch, and dinner with three interspersed high nutrient–dense snacks help improve nutritional intake (Hockenberry and Wilson, 2011). Calcium and phosphorus are important for healthy bone growth.
Toddlers who consume more than 24 ounces of milk daily in place of other foods sometimes develop milk anemia because milk is a poor source of iron. Toddlers need to drink whole milk until the age of 2 years to make sure that there is adequate intake of fatty acids necessary for brain and neurological development. Certain foods such as hot dogs, candy, nuts, grapes, raw vegetables, and popcorn have been implicated in choking deaths and need to be avoided. Dietary requirements for preschoolers (3 to 5 years) are similar to those for toddlers. They consume slightly more than toddlers, and nutrient density is more important than quantity.
School-age children, 6 to 12 years old, grow at a slower and steadier rate, with a gradual decline in energy requirements per unit of body weight. Despite better appetites and more varied food intake, you need to assess school-age children’s diets carefully for adequate protein and vitamins A and C. They often fail to eat a proper breakfast and have unsupervised intake at school. High fat, sugar, and salt result from too-liberal intake of snack foods. Physical activity level decreases consistently, and high-calorie, readily available food increases in consumption, leading to an increase in childhood obesity (Budd and Hayman, 2008).
In the last 20 years the prevalence of overweight children has risen. The percent of obesity in children ages 6 to 11 years has doubled to 17%, and the percent of overweight adolescents has more than tripled to 17.6% (Li and Hooker, 2010). A combination of factors contributes to the problem, including a diet rich in high-calorie foods, food advertising targeting children, inactivity, genetic predisposition, use of food as a coping mechanism for stress or boredom or as a reward or celebration, and family and social factors (Budd and Hayman, 2008). Childhood obesity contributes to medical problems related to the cardiovascular system, endocrine system, and mental health (Budd and Hayman, 2008). As a result of the obesity, the incidence of type II diabetes in children is also increasing. Prevention of childhood obesity is critical because of the long-term effects. Family education is an important component in decreasing the prevalence of this problem. Promote healthy food choices and eating in moderation along with increased physical activity.
Adolescents.
During adolescence physiological age is a better guide to nutritional needs than chronological age. Energy needs increase to meet greater metabolic demands of growth. Daily requirement of protein also increases. Calcium is essential for the rapid bone growth of adolescence, and girls need a continuous source of iron to replace menstrual losses. Boys also need adequate iron for muscle development. Iodine supports increased thyroid activity, and use of iodized table salt ensures availability. B-complex vitamins are necessary to support heightened metabolic activity.
Many factors other than nutritional needs influence the adolescent’s diet, including concern about body image and appearance, desire for independence, eating at fast-food restaurants, peer pressure, and fad diets. Nutritional deficiencies often occur in adolescent girls as a result of dieting and use of oral contraceptives. An adolescent boy’s diet is often inadequate in total kilocalories, protein, iron, folic acid, B vitamins, and iodine. Snacks provide approximately 25% of a teenager’s total dietary intake. Fast food, particularly value-size or super-size meals, is common and adds extra salt, fat, and kilocalories (Budd and Hayman, 2008). Skipping meals or eating meals with unhealthy choices of snacks contributes to nutrient deficiency and obesity (Hockenberry and Wilson, 2011).
Fortified foods (nutrients added) are important sources of vitamins and minerals. Snack food from the dairy and fruit and vegetable groups are good choices. To counter obesity, increasing physical activity is often more important than curbing intake. The onset of eating disorders such as anorexia nervosa or bulimia nervosa often occurs during adolescence. Recognition of eating disorders is essential for early intervention (Box 44-3).