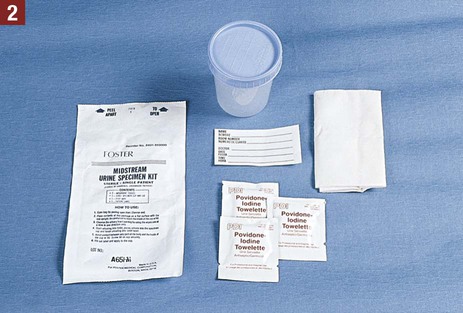
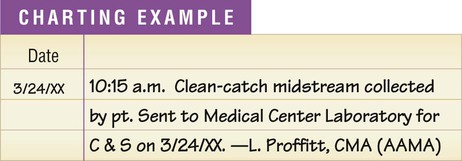
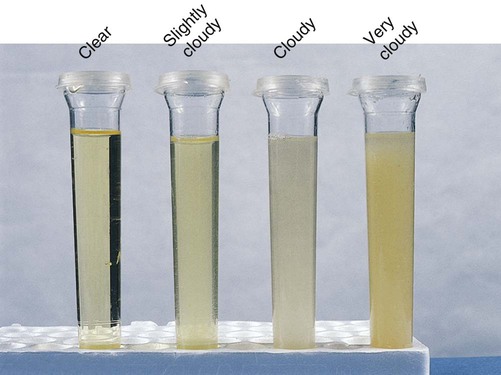
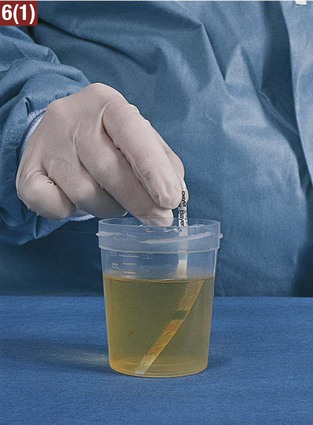
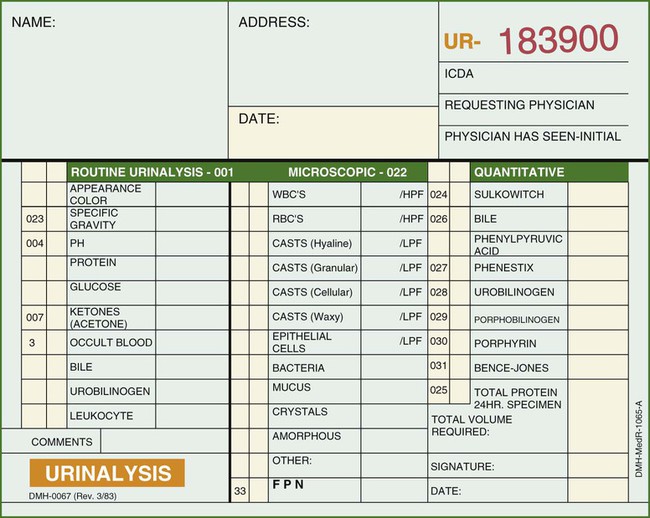
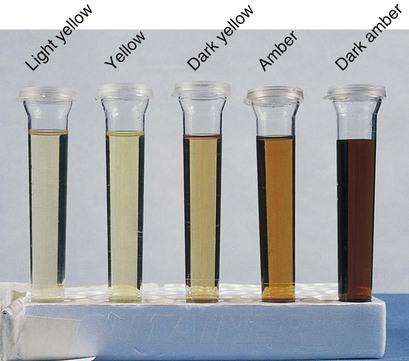
3. Explain why a first-voided morning specimen is often preferred for urinalysis. 4. Explain the purpose of collecting a clean-catch midstream specimen. 5. Explain the purpose of a 24-hour urine collection. 6. List changes that may occur if urine is allowed to remain standing for longer than 1 hour. Anuria Failure of the kidneys to produce urine Diuresis Secretion and passage of large amounts of urine Dysuria Difficult or painful urination Frequency The condition of having to urinate often Hematuria Blood present in the urine Nocturia Excessive (voluntary) urination during the night Nocturnal enuresis Inability of an individual to control urination at night during sleep (bedwetting) Oliguria Decreased output of urine Polyuria Increased output of urine Pyuria Pus present in the urine Retention The inability to empty the bladder. The urine is being produced normally but is not being voided Urgency The immediate need to urinate The guidelines listed should be followed in collection of a urine specimen: 1. The medical assistant must obtain an adequate volume of urine as necessary for the type of test (usually 30 to 50 mL of urine). 2. Each specimen must be labeled properly with the patient’s name and date of birth, the date and time of collection, and the type of specimen (i.e., urine) to avoid any mix-ups in specimens. 3. Any medication the patient is taking should be recorded on the laboratory requisition and in the patient’s chart, because some medications may interfere with the accuracy of the test results. 4. If possible, the collection of a urine specimen should be avoided in women during menstruation and for several days thereafter because the specimen may become contaminated with blood. This results in a false-positive test result for blood in the urine. 5. The medical assistant should take into consideration that voiding may be difficult for patients under stress and anxiety. In these instances, understanding and patience should be conveyed to the patient. 6. A urine specimen may be difficult to obtain from a child, even with the assistance of a parent. In this case, the physician should be informed because another collection method may be used, such as a urine collection bag, suprapubic aspiration, or catheterization of the patient. Guidelines that should be followed when collecting a clean-catch midstream specimen are listed: 1. A clean-catch midstream specimen is collected by the patient at the medical office. The medical assistant must provide complete instructions for collection of this specimen. Failure to instruct the patient adequately may necessitate a return to the medical office for the collection of another specimen because of bacterial contamination. Patient instructions for obtaining a clean-catch midstream specimen are presented in Procedure 30-1. 2. The medical assistant must label the container with the patient’s name and date of birth, the date, the time of collection, and the type of specimen (clean-catch midstream specimen). 3. For reliable test results, the specimen should be tested immediately and should not be allowed to stand. If this is not possible, the specimen should be refrigerated, or a preservative should be added. 4. If the specimen is to be tested at an outside laboratory, completion of a laboratory requisition to accompany it is necessary. A urinalysis laboratory request form is shown in Figure 30-1. 5. The procedure is completed by sanitizing the hands and recording the procedure in the patient’s chart. The information to be charted for specimens tested at the medical office includes the date and time, the type of specimen collected, and the laboratory test results. If the specimen is being transported to an outside laboratory for testing, record the date and time, the type of specimen collected, and the date the specimen was transported to the laboratory. 1. Bacteria in the environment that get into the urine specimen work on the urea present in the urine, converting it to ammonia. Because ammonia is alkaline, an acid urine becomes alkaline, increasing the pH. In addition, an alkaline pH may result in a false-positive result on the protein test. 2. Bacteria multiply rapidly in the urine, resulting in a cloudy specimen and an increase in the nitrite. 3. If glucose is present in the specimen, it decreases in amount because microorganisms use the glucose as a source of food. 4. If any red or white blood cells are present, they may break down. The color of the urine is the result of the presence of a yellow pigment known as urochrome, produced by the breakdown of hemoglobin. It is common for the color of urine to vary among different shades of yellow within the course of a day. Classifications that can be used to describe the color of urine include light yellow, yellow, dark yellow, light amber, amber, and dark amber (Figure 30-2). In the medical office, specific gravity is most commonly measured using a reagent strip. This involves a color comparison determination with a reagent strip that contains a reagent area for specific gravity. The reagent strip is dipped into the urine specimen, and the results are compared with a color chart (see Procedure 30-2).
Urinalysis
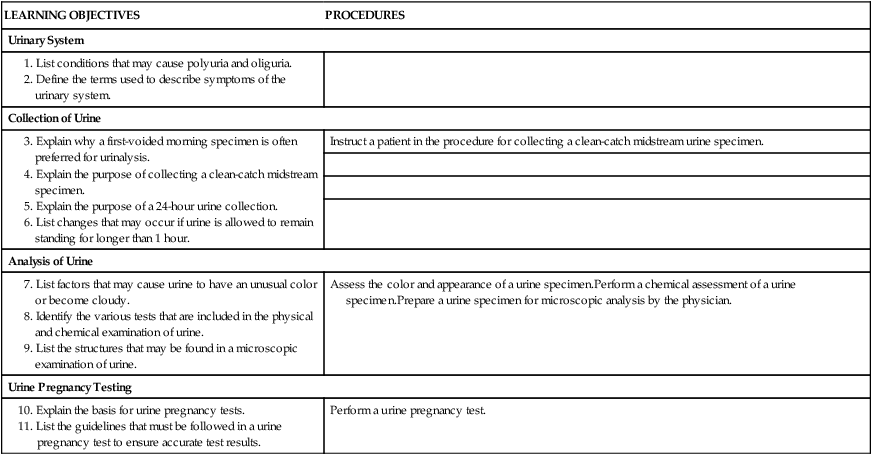
LEARNING OBJECTIVES
PROCEDURES
Urinary System
Collection of Urine
Instruct a patient in the procedure for collecting a clean-catch midstream urine specimen.
Analysis of Urine
Assess the color and appearance of a urine specimen.Perform a chemical assessment of a urine specimen.Prepare a urine specimen for microscopic analysis by the physician.
Urine Pregnancy Testing
Perform a urine pregnancy test.
Composition of Urine
Terms Related to the Urinary System
Collection of Urine
Guidelines for Urine Collection
Urine Specimen Collection Methods
Clean-Catch Midstream Specimen
Guidelines
Analysis of Urine
Physical Examination of Urine
Color
Specific Gravity

Urinalysis
Get Clinical Tree app for offline access