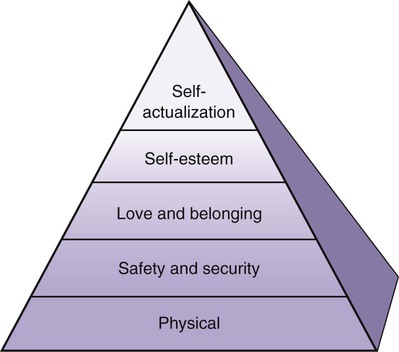
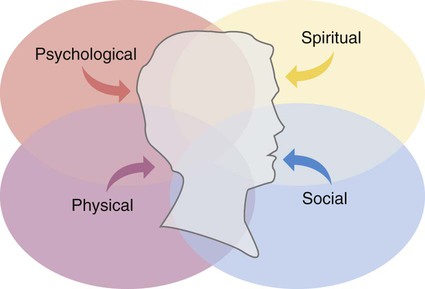
• Define the key terms listed in this chapter. • Identify the parts that make up the whole person. • Explain how to properly address the person. • Explain Abraham Maslow’s theory of basic needs. • Explain how culture and religion influence health and illness. • Explain how to deal with behavior issues. • Identify the elements needed for good communication. • Describe how to use verbal and nonverbal communication. • Explain the methods and barriers to good communication. • Explain how to communicate with persons who have behavioral problems. • Explain why family and visitors are important to the person. • Identify courtesies given to the person, family, and friends. • Explain how to promote PRIDE in the person, the family, and yourself. Holism means whole. Holism is a concept that considers the whole person. The whole person has physical, social, psychological, and spiritual parts. These parts are woven together and cannot be separated (Fig. 6-1). A need is something necessary or desired for maintaining life and mental well-being. According to psychologist Abraham Maslow, basic needs must be met for a person to survive and function. These needs are arranged in order of importance (Fig. 6-2). Lower-level needs must be met before the higher-level needs. Basic needs, from the lowest level to the highest level, are: • Physical needs. Oxygen, food, water, elimination, rest, and shelter are needed for life and to survive. A person dies within minutes without oxygen. Without food or water, a person feels weak and ill within a few hours. The kidneys and intestines must function. Otherwise, poisonous wastes build up in the blood and can cause death. Without enough rest and sleep, a person becomes very tired. Without shelter, the person is exposed to extremes of heat and cold. • Safety and security needs. The person needs to feel safe from harm, danger, and fear. Health care agencies are strange places with strange routines and equipment. Some care causes pain or discomfort. People feel safe and more secure if they know what will happen. For every task, the person should know: • Love and belonging needs. These needs relate to love, closeness, affection, and meaningful relationships with others. Some people become weaker or die from the lack of love and belonging. This is seen in older persons who have out-lived family and friends. • Self-esteem needs. Self-esteem means to think well of oneself and to see oneself as useful and having value. People often lack self-esteem when ill, injured, older, or disabled. • The need for self-actualization. Self-actualization means experiencing one’s potential. It involves learning, understanding, and creating to the limit of a person’s capacity. This is the highest need. Rarely, if ever, is it totally met. Most people constantly try to learn and understand more. This need can be postponed and life will continue. People come from many cultures, races, and nationalities. Their family practices and food choices may differ from yours. So might their hygiene habits and clothing styles. Some speak a foreign language. Some cultures have beliefs about what causes and cures illness. (See Caring About Culture: Health Care Beliefs.) They may perform rituals to rid the body of disease. (See Caring About Culture: Sick Care Practices.) Many cultures have health beliefs and rituals about dying and death (Chapter 32). Culture also is a factor in communication. See Focus on Communication: Culture and Religion. • Anger. Anger is a common emotion. Causes include fear, pain, and dying and death. Loss of function and loss of control over health and life are causes. Anger is a symptom of some diseases that affect thinking and behavior. Some people are generally angry. Anger is communicated verbally and nonverbally. Verbal outbursts, shouting, raised voices, and rapid speech are common. Some people are silent. Others are not cooperative. They may refuse to answer questions. Nonverbal signs include rapid movements, pacing, clenched fists, and a red face. Glaring and getting close to you when speaking are other signs. Violent behaviors can occur. • Demanding behavior. Nothing seems to please the person. The person is critical of others. He or she wants care given at a certain time and in a certain way. Loss of independence, loss of health, and loss of control of life are causes. So are unmet needs. • Self-centered behavior. The person cares only about his or her own needs. The needs of others are ignored. The person demands the time and attention of others. The person becomes impatient if needs are not met. • Aggressive behavior. The person may swear, bite, hit, pinch, scratch, or kick. Fear, anger, pain, and dementia (Chapter 30) are causes. Protect the person, others, and yourself from harm (Chapter 9). • Withdrawal. The person has little or no contact with family, friends, and staff. He or she spends time alone and does not take part in social or group activities. This may signal physical illness or depression. Some people are not social. They prefer to be alone. • Inappropriate sexual behavior. Some people make inappropriate sexual remarks. Or they touch others in the wrong way. Some disrobe or masturbate in public. These behaviors may be on purpose. Or they are caused by disease, confusion, dementia, or drug side effects. Some behaviors are not pleasant. You cannot avoid the person or lose control. Good communication is needed. Behaviors are addressed in the care plan. The care plan may include some of the guidelines in Box 6-1, p. 62. See Focus on Communication: Behavior Issues, p. 62. • Follow the rules of communication (Chapter 5). • Use words that have the same meaning for you and the person. • Avoid medical terms and words not familiar to the person. • Communicate in a logical and orderly manner. Do not wander in thought. • Understand and respect the patient or resident as a person. • View the person as a physical, psychological, social, and spiritual human being. • Appreciate the person’s problems and frustrations. • Respect the person’s rights, religion, and culture. • Give the person time to understand the information that you give. • Repeat information as often as needed. Repeat what you said. Use the exact same words. Do not give the person a new message to process. If the person does not seem to understand after repeating, try re-phrasing the message. This is very important for persons with hearing problems. • Ask questions to see if the person understood you. • Be patient. People with memory problems may ask the same question many times. Do not say that you are repeating information. • Include the person in conversations when others are present. This includes when a co-worker is assisting with care. See Focus on Older Persons: Communicating With the Person.
Understanding the Person
Caring for the Person
Basic Needs
Culture and Religion
Behavior Issues
Communicating With the Person
Understanding the Person
Get Clinical Tree app for offline access