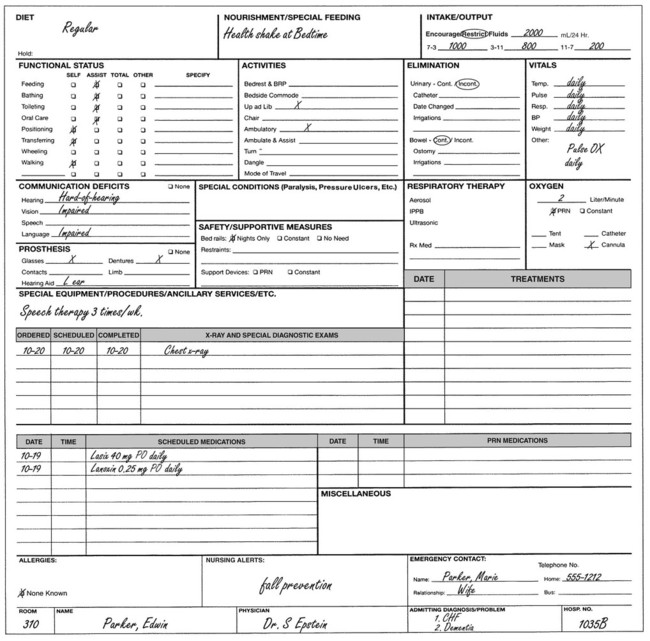
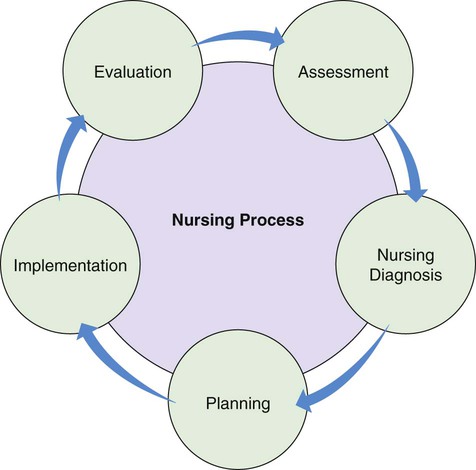
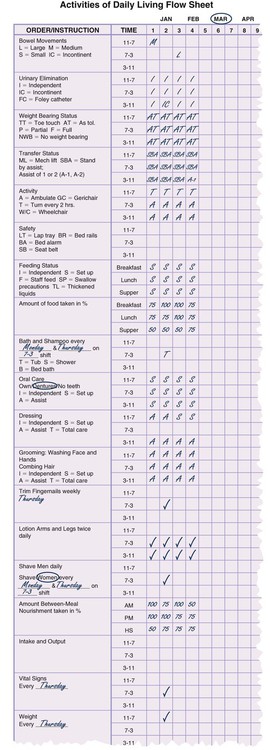
Chapter 5 ADL Activities of daily living EPHI; ePHI Electronic protected health information OBRA Omnibus Budget Reconciliation Act of 1987 • Define the key terms and key abbreviations listed in this chapter. • Describe the rules for good communication. • Describe the legal and ethical aspects of medical records. • Identify common parts of the medical record. • Explain your role in the nursing process. • List the information you need to report to the nurse. • List the rules for recording. • Use the 24-hour clock, medical terminology, and medical abbreviations. • Explain how computers and other electronic devices are used in health care. • Explain how to protect the right to privacy when using computers and other electronic devices. • Describe how to answer phones. • Explain how to problem solve and deal with conflict. • Explain how to promote PRIDE in the person, the family, and yourself. A report that the nurse gives at the end of the shift to the on-coming shift; change-of-shift report • Use words that mean the same thing to you and the message receiver. Avoid words with more than 1 meaning. What does “far” mean—50 feet or 100 feet? • Use familiar words. Avoid terms that the person and family do not understand. • Be brief and concise. Do not add unrelated or unnecessary information. Stay on the subject. Do not wander in thought or get wordy. • Give information in a logical and orderly way. Organize your thoughts. Present them step-by-step. • Give facts and be specific. You report a pulse rate of 110. It is more specific and factual than saying the “pulse is fast.” Agencies have policies about medical records and who can access them. Policies address: Common parts of the record include: • Admission information—is gathered when the person is admitted to the agency. It includes the person’s identifying information. • Health history—is completed by the nurse. The nurse asks about current and past illnesses, signs and symptoms, allergies, and drugs. • Flow sheets and graphic sheets—are used to record care measures, observations, and measurements made daily, every shift, or 3 to 4 times a day (Fig. 5-1). Information includes vital signs (blood pressure, temperature, pulse, respirations), weight, intake and output (Chapter 20), bowel movements, doctor visits, and everyday activities. • Progress notes and nurses’ notes—are used to describe observations, the care given, and the person’s response and progress. They are used to record information about treatments, some drugs, and procedures. In long-term care, summaries of care describe the person’s progress toward meeting goals and response to care. The Kardex or care summary provides a quick, easy reference to the person’s drugs, treatments, diagnoses, care measures, equipment, and special needs. The Kardex is a type of card file (Fig. 5-2). With computer systems, the person’s information is organized in a care summary. The summary can be printed for reference when providing care. The nursing process is the method nurses use to plan and deliver nursing care. It has 5 steps. The nursing process is on-going. New information is gathered and the person’s needs may change. However, the steps are the same. You will see how the nursing process is continuous as each step is explained (Fig. 5-3). You have a key role in the nursing process. Your observations are used for the assessment step. You may help develop the care plan. In the implementation step, you perform tasks in the care plan. Your assignment sheet (p. 51) tells you what to do. Your observations are used for the evaluation step. Observation is using the senses of sight, hearing, touch, and smell to collect information. • You see how the person lies, sits, or walks. You see flushed or pale skin. You see red and swollen body areas. • You listen to the person breathe, talk, and cough. You use a stethoscope to measure blood pressure. • Through touch, you feel if the skin is hot or cold, or moist or dry. You use touch to take the person’s pulse. • Smell is used to detect body, wound, and breath odors. You also smell odors from urine and bowel movements. Box 5-1 lists the observations to report at once. Box 5-2, p. 48 lists the observations you need to make and report to the nurse. Make notes of your observations. Use them to report and record observations. Carry a note pad and pen in your pocket. Note your observations as you make them. The Omnibus Budget Reconciliation Act of 1987 (OBRA) requires the Minimum Data Set (MDS) for nursing center residents (Appendix D). It provides extensive information about the person. Examples include memory, communication, hearing and vision, physical function, and activities. The RN uses assessment information to make a nursing diagnosis. A nursing diagnosis describes a health problem that can be treated by nursing measures (Box 5-3, p. 49). It is different from a medical diagnosis—the identification of a disease or condition by a doctor. Cancer, stroke, heart attack, and diabetes are examples of medical diagnoses.
Communicating With the Health Team
Key Abbreviations
Communication
The Medical Record
The Kardex or Care Summary
The Nursing Process
Assessment
The Minimum Data Set.
Nursing Diagnosis