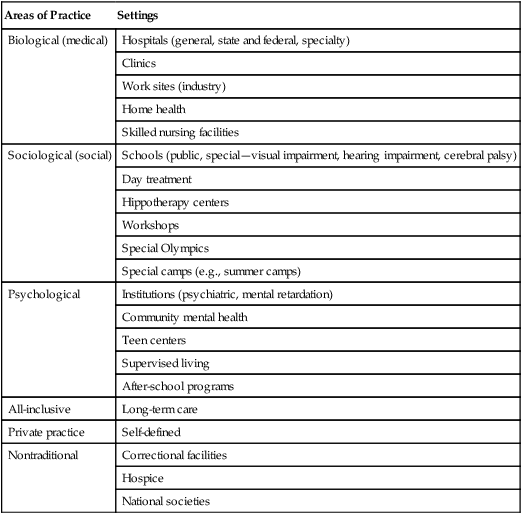
After reading this chapter, the reader will be able to do the following: • Characterize settings in which OT practitioners are employed by types of administration, levels of care, and areas of practice • Identify the primary health problems addressed in different settings • Describe how treatment setting influences the focus of OT intervention LINDA S. FAZIO, PhD, OTR/L, FAOTA Professor of Clinical Occupational Therapy Assistant Chair and Coordinator of the Professional Program Department of Occupational Science and Occupational Therapy University of Southern California Public agencies are operated by federal, state, or county governments. Federal agencies include the Veterans Administration Hospitals and Clinics, Public Health Services Hospitals and Clinics, and Indian Health Services. State-run agencies may include correctional facilities, mental health centers, and medical school hospitals, and their clinics. The county may operate county hospitals, clinics, and rehabilitation facilities that deliver services to clients in the same way as federal and state facilities. However, county administration must follow different rules and regulations than federal and state administrations, which may affect employment or method of reimbursement. Private not-for-profit agencies receive special tax exemptions and typically charge a fee for services and maintain a balanced budget to provide services. These agencies include hospitals and clinics with religious affiliations, private teaching hospitals, and organizations such as the Easter Seal Society and United Cerebral Palsy. Private for-profit agencies are owned and operated by individuals or a group of investors. These agencies are in business to make a profit. Large for-profit corporations may form multi-facility systems. These corporations may focus on one specific level of care (e.g., all hospitals or all skilled nursing facilities) or own multiple facilities across the continuum of care (e.g., a hospital, a skilled nursing facility, and an outpatient facility). A multi-facility system is able to buy supplies and equipment in bulk at a lower volume rate. Because these systems provide a wider range of services, they have an advantage when it comes to developing contracts with third-party payers to provide health care services. Another way of characterizing health care settings is by the level of care required by the client. Health care is provided to the consumer along a continuum, as the client’s needs dictate, referred to as the continuum of care. Acute care is the first level on the continuum. A client at this level has a sudden and short-term need for services and is typically seen in a hospital. Services provided in the hospital are expensive because of the high cost of technology and the number of services provided. The Prospective Payment System, introduced under Public Law 98-21 and passed in 1983, changed the way in which hospitals were paid through Medicare. Under this system, a nationwide schedule defines how much Medicare reimburses hospitals. Depending on the client’s diagnosis, hospitals are paid a predetermined, fixed fee, based on diagnosis-related groups (DRGs), regardless of the services provided. The system provides an incentive for hospitals and physicians to reduce costs and to discharge clients from the hospital as soon as possible. As a result of the 1983 Prospective Payment System, the average length of a hospital stay has decreased.8 The move to short hospital stays and the implementation of cost-cutting measures have resulted in a decrease in the number of OT practitioners working in hospital-based settings.7–9 See Table 11-1. Table 11-1 Note: The categories do not indicate specialization. There are overlapping services in all areas; the classification highlights the setting’s primary concern. Adapted from Reed K, Sanderson SR: Concepts in Occupational Therapy, ed 3, Baltimore, 1992, Lippincott Williams & Wilkins. Shorter hospital stays also created a need for an interim level of care, referred to as subacute care. At this level, the client still needs care but does not require an intensive level or specialized service, thereby reducing hospital costs. Typically these clients require 1 to 4 weeks more of rehabilitation. Hospitals with excess acute care beds have converted beds to less expensive subacute care beds, whereas skilled nursing facilities have upgraded some beds to the subacute level.6 Freestanding subacute care facilities have been established to address client needs. The client typically served by a subacute care facility may be a person who has sustained a stroke or hip fracture, or one who has a cardiac condition or cancer. Rehabilitation services, including occupational therapy services, are a major component of subacute care. Long-term care serves clients who are medically stable but who have a chronic condition requiring services over time, potentially throughout life. Persons who have developmental disabilities, history of mental illness, age-related disabilities, or injury resulting in a severe disability may require this level of care. Services provided at this level may take place in an institution, skilled nursing or extended care facility, residential care facility, client’s home, outpatient clinic, or community-based program. Health care practice areas may be grouped into (1) biological (medical), (2) psychological, and (3) sociological (social). Health problems occurring in any of the areas affect a person’s ability to engage in occupations. OT practitioners help clients make adjustments and find new ways to function by planning and guiding improvement of function in any or all of the three areas of practice. See Table 11-1.
Treatment Settings and Areas of Practice

Characteristic of Settings
Administration of Setting
Levels of Care
Areas of Practice
Settings
Biological (medical)
Hospitals (general, state and federal, specialty)
Clinics
Work sites (industry)
Home health
Skilled nursing facilities
Sociological (social)
Schools (public, special—visual impairment, hearing impairment, cerebral palsy)
Day treatment
Hippotherapy centers
Workshops
Special Olympics
Special camps (e.g., summer camps)
Psychological
Institutions (psychiatric, mental retardation)
Community mental health
Teen centers
Supervised living
After-school programs
All-inclusive
Long-term care
Private practice
Self-defined
Nontraditional
Correctional facilities
Hospice
National societies
Areas of Practice
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Treatment Settings and Areas of Practice
Get Clinical Tree app for offline access
