Theoretical Foundations of Nursing Practice
Objectives
• Explain the influence of nursing theory on a nurse’s approach to practice.
• Describe types of nursing theories.
• Describe the relationship between nursing theory, the nursing process, and patient needs.
• Discuss selected theories from other disciplines.
• Discuss selected nursing theories.
Key Terms
Assumptions, p. 42
Concepts, p. 41
Content, p. 43
Descriptive theory, p. 42
Domain, p. 40
Environment/situation, p. 41
Feedback, p. 43
Grand theories, p. 42
Health, p. 41
Input, p. 43
Interdisciplinary theory, p. 43
Middle-range theories, p. 42
Nursing, p. 41
Nursing paradigm, p. 40
Nursing theory, p. 41
Output, p. 43
Paradigm, p. 40
Person, p. 40
Phenomenon, p. 41
Prescriptive theories, p. 42
Theory, p. 41
![]()
Providing patient-centered nursing care is an expectation for all nurses. As you progress through your curriculum, you will learn to apply knowledge from nursing science, social sciences, physical sciences, biobehavioral sciences, ethics, and health policy. To address individual and family responses to health problems, theory-based nursing practice is important for designing and implementing nursing interventions. Initially you might find nursing theory difficult to understand or appreciate. However, as you increase your knowledge about theories, you will find that they help to describe, explain, predict, and/or prescribe nursing care measures. For example, a theory about caring gives you a way to communicate with your patients and their families and individualize care to meet their needs (Watson, 2010; Sumner, 2010). The scientific work used in developing theories expands the scientific knowledge of the profession. Theories offer well-grounded rationales for how and why nurses perform specific interventions and for predicting patient behaviors and outcomes.
Expertise in nursing is a result of knowledge and clinical experience. The expertise required to interpret clinical situations and make clinical judgments is the essence of nursing care and the basis for advancing nursing practice and nursing science (Benner et al., 2010). As you progress through your courses, reflect and learn from your experiences to grow professionally and use well-developed theories as a basis for your approach to patient care.
The Domain of Nursing
The domain is the perspective of a profession. It provides the subject, central concepts, values and beliefs, phenomena of interest, and central problems of a discipline. The domain of nursing provides both a practical and theoretical aspect of the discipline. It is the knowledge of nursing practice as well as the knowledge of nursing history, nursing theory, education, and research. The domain of nursing gives nurses a comprehensive perspective that allows you to identify and treat patients’ health care needs at all levels and in all health care settings.
A paradigm is a pattern of thought that is useful in describing the domain of a discipline. A paradigm links the knowledge of science, philosophy, and theories accepted and applied by the discipline. The paradigm of nursing includes four links: the person, health, environment/situation, and nursing. The elements of the nursing paradigm direct the activity of the nursing profession, including knowledge development, philosophy, theory, educational experience, research, and practice (Alligood and Tomey, 2010).
Person is the recipient of nursing care, including individual patients, groups, families, and communities. The person is central to the nursing care you provide. Because each person’s needs are often complex, it is important to provide individualized patient-centered care.
Health has different meanings for each patient, the clinical setting, and the health care profession (see Chapter 6). It is dynamic and continuously changing. Your challenge as a nurse is to provide the best possible care based on the patient’s level of health and health care needs at the time of care delivery.
Environment/situation includes all possible conditions affecting patients and the settings in which their health care needs occur. There is a continuous interaction between a patient and the environment. This interaction has positive and negative effects on the person’s level of health and health care needs. Factors in the home, school, workplace, or community all influence a patient’s level of health and health care needs. For example, an adolescent girl with type 1 diabetes needs to adapt her treatment plan to adjust for physical activities of school, the demands of a part-time job, and the timing of social events such as her prom.
Nursing is the “… diagnosis and treatment of human responses to actual or potential health problems …” (American Nurses Association, 2010). The scope of nursing is broad. For example, a nurse does not medically diagnose a patient’s health condition as heart failure. However, a nurse will assess a patient’s response to the decrease in activity tolerance as a result of the disease and develop nursing diagnoses of fatigue, activity intolerance, and ineffective coping. From these nursing diagnoses the nurse creates a patient-centered plan of care for each of the patient’s health problems (see Unit 3). Use critical thinking skills to integrate knowledge, experience, attitudes, and standards into the individualized plan of care for each of your patients (see Chapter 15).
Theory
Theories are designed to explain a phenomenon such as self-care or caring. For example, the nurse using Orem’s self-care deficit theory helps to explain how patients meet their own therapeutic self-care demands. In this theory, nurses assist patients by acting for them or guiding necessary physical and/or psychological support (Alligood, 2010). Orem’s theory contains a detailed framework of self-care concepts that are linked in such a way as to explain, describe, or predict the type of nursing care that helps patients achieve a better level of health (McEwen and Willis, 2011). A theory is a way of seeing through a “set of relatively concrete and specific concepts and the propositions that describe or link the concepts” (Fawcett, 2005).
A nursing theory is a conceptualization of some aspect of nursing that describes, explains, predicts, or prescribes nursing care (Meleis, 2011). For example, Orem’s self-care deficit theory (2001) explains the factors within a patient’s living situation that support or interfere with his or her self-care ability. As a result, a nurse who practices using this theory can anticipate such factors when designing an education plan for the patient. This theory has value in helping nursing design interventions to promote the patient’s self-care in managing an illness such as asthma, heart failure, diabetes, or arthritis.
Theories constitute much of the knowledge of a discipline. Theory and scientific inquiry are vital links to one another, providing guidelines for decision making, problem solving, and nursing interventions (Selanders, 2010). Theories give us a perspective for assessing our patients’ situations and organizing data and methods for analyzing and interpreting information. For example, if you use Orem’s theory in practice, you assess and interpret data to determine patients’ self-care needs, self-care deficits, and self-care abilities in the management of their disease. The theory then guides the design of patient-centered nursing interventions. Application of nursing theory in practice depends on the knowledge of nursing and other theoretical models, how they relate to one another, and their use in designing nursing interventions.
Nursing is a science and an art. Nurses need a theoretical base to demonstrate knowledge about the science and art of the profession when they promote health and wellness for their patients, whether the patient is an individual, a family, or a community (Porter, 2010). A nursing theory helps to identify the focus, means, and goals of practice. Common theories enhance communication and increase autonomy and accountability for care to our patients (Meleis, 2011).
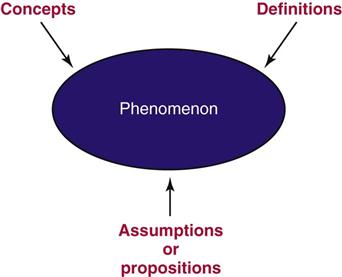
Components of a Theory
A theory contains a set of concepts, definitions, and assumptions or propositions that explain a phenomenon. The theory explains how these elements are uniquely related in the phenomenon (Fig. 4-1). For example, Kristin Swanson developed her theory about the phenomenon of caring by conducting extensive interviews with patients and their professional caregivers (Swanson, 1991). Swanson’s theory of caring defines five components of caring: knowing, being with, doing for, enabling, and maintaining belief (see Chapter 7). These components provide a foundation of knowledge for nurses to direct and deliver caring nursing practices. Researchers test theories, and as a result they get a clearer perspective of all parts of a phenomenon. Swanson’s theory of caring is one that provides a basis for identifying and testing nurse caring behaviors to determine if caring improves patient health outcomes (Watson, 2010).
Phenomenon
Nursing theories focus on the phenomena of nursing and nursing care. A phenomenon is the term, description, or label given to describe an idea or responses about an event, a situation, a process, a group of events, or a group of situations (Meleis, 2011). This phenomenon may be temporary or permanent. Examples of phenomena of nursing include caring, self-care, and patient responses to stress. For example, in Neuman’s systems model (2011), phenomena focus on stressors perceived by the patient or caregiver. The theoretical model is an open systems model that views nursing as being primarily concerned with nursing actions in stress-related situations. These stressors may include, but are not limited to, patient responses, internal and external environmental factors, and nursing actions.
Concepts
A theory also consists of interrelated concepts. These concepts can be simple or complex and relate to an object or event that comes from individual perceptual experiences (Alligood and Tomey, 2010). Think of concepts as ideas and mental images. They help describe or label phenomena. Again, using Neuman’s systems model (2011) as an example, there are concepts that affect the patient system. The patient system can be an individual, a group, a family, or a community. This system is an open structure that includes internal and external environmental factors. These concepts are physiological, psychological, sociocultural, developmental, and spiritual and may relate to health and wellness, illness prevention, stressors, and defense mechanisms (Meleis, 2011).
Definitions
The definitions within a theory communicate the general meaning of the concepts. These definitions describe the activity necessary to measure the concepts within a theory (Alligood and Tomey, 2010). For example, Neuman’s model uses an open systems approach to describe how patient systems deal with stressors in their environments. A stressor is any stimuli that can produce tension and cause instability within the system. The environment includes internal and external factors that have the potential to affect the patient system. Internal factors exist within the patient system (e.g., the physiological and behavioral responses to illnesses). External factors are outside the patient system (e.g., changes in health care policy or an increase in the crime rate). It is important that nurses using Neuman’s theory in practice focus their care on the system’s responses to the stressors (Meleis, 2011). For example, when patients receive a new diagnosis and perceive the diagnosis to be stressful, they may react by withdrawing or eating an improper diet. In this situation the nurse focuses on both the illness process and the patient’s response to the stressors and designs appropriate interventions.
Assumptions
Assumptions are the “taken-for-granted” statements that explain the nature of the concepts, definitions, purpose, relationships, and structure of a theory (Meleis, 2011). For example, in Neuman’s systems model the assumptions include the following: patients are dynamic; the relationships between the concepts of a theory influence a patient’s protective mechanisms and determine a patient’s response; patients have a normal range of responses; stressors attack flexible lines of defense followed by the normal lines of defense; and the nurse’s actions focus on primary, secondary, and tertiary prevention (Neuman, 2011).
Types of Theory
The general purpose of a theory is important because it specifies the context and situation in which the theory applies (Chinn and Kramer, 2011). For example, theories about pain focus on pain: its cause, effects, and alleviation measures. Theories have different purposes and are sometimes classified by levels of abstraction (grand theories versus middle-range theories) or the goals of the theory (descriptive or prescriptive). For example, a descriptive theory describes a phenomenon such as grief or caring. A predictive theory identifies conditions or factors that predict a phenomenon. A prescriptive theory details nursing interventions for a specific phenomenon and the expected outcome of the care. Box 4-1 summarizes goals of theoretical nursing models.
Grand theories are systematic and broad in scope, complex, and therefore require further specification through research. A grand theory does not provide guidance for specific nursing interventions; but it provides the structural framework for broad, abstract ideas about nursing. For example, Neuman’s systems model is a grand theory that provides a comprehensive foundation for scientific nursing practice, education, and research (Walker and Avant, 2009).
Middle-range theories are more limited in scope and less abstract. They address a specific phenomenon and reflect practice (administration, clinical, or teaching). A middle-range theory tends to focus on a specific field of nursing, such as uncertainty, incontinence, social support, quality of life, and caring, rather than reflect on a wide variety of nursing care situations (Meleis, 2011). For example, Mishel’s theory of uncertainty in illness (1990; 1997) focuses on patients’ experiences with cancer while living with continual uncertainty. The theory provides a basis to help nurses understand how patients cope with uncertainty and the illness response.
Descriptive theories are the first level of theory development. They describe phenomena, speculate on why they occur, and describe their consequences. These theories explain, relate, and in some situations predict nursing phenomena (Meleis, 2011). For example, theories of growth and development describe the maturation processes of an individual at various ages (see Chapter 11). Descriptive theories do not direct specific nursing activities but help to explain patient assessments.
Prescriptive theories address nursing interventions for a phenomenon, describe the conditions under which the prescription (i.e., nursing interventions) occurs, and predict the consequences (Meleis, 2011). Prescriptive theories are action oriented and test the validity and predictability of a nursing intervention. These theories guide nursing research to develop and test specific nursing interventions (George, 2011). For example, Mishel’s theory of uncertainty predicts that increasing the coping skills of patients with gynecological cancer assists their ability to deal with the uncertainty of the cancer diagnosis and treatment (Mishel, 1997). Thus the theory provides a framework to design interventions that support and strengthen patients’ coping resources.
Theory-Based Nursing Practice
Nursing is a practice-oriented discipline. Nursing knowledge is derived from basic and nursing sciences, experience, aesthetics, nurses’ attitudes, and standards of practice. As nursing continues to grow as a profession, knowledge is needed to prescribe specific interventions to improve patient outcomes. Nursing theories and related concepts continue to evolve. Florence Nightingale spoke with firm conviction about the “nature of nursing as a profession that requires knowledge distinct from medical knowledge” (Nightingale, 1860; Selanders, 2010). The overall goal of nursing knowledge is to explain the practice of nursing as different and distinct from the practice of medicine, psychology, and other health care disciplines. Theory generates nursing knowledge for use in practice, thus supporting evidence-based practice. The integration of theory into practice is the basis for professional nursing (McEwen and Wills, 2011).
The nursing process is used in clinical settings to determine individual patient needs (see Unit 3). Although the nursing process is central to nursing, it is not a theory. It provides a systematic process for the delivery of nursing care, not the knowledge component of the discipline. However, a theory can direct how a nurse uses the nursing process. For example, the theory of caring influences what to assess, how to determine patient needs, how to plan care, how to select individualized nursing interventions, and how to evaluate patient outcomes.
Interdisciplinary Theories
To practice in today’s health care systems, nurses need a strong scientific knowledge base from nursing and other disciplines such as the physical, social, and behavioral sciences. Knowledge from these other disciplines includes relevant theories that explain phenomena. An interdisciplinary theory explains a systematic view of a phenomenon specific to the discipline of inquiry. For example, Piaget’s theory of cognitive development helps to explain how children think, reason, and perceive the world (see Chapter 11). Knowledge and use of this theory helps pediatric nurses design appropriate therapeutic play interventions for ill toddlers or school-age children.
Systems Theory
A system is composed of separate components. The components are interrelated and share a common purpose to form a whole. There are two types of systems, open and closed. An open system such as a human organism or a process such as the nursing process interacts with the environment, exchanging information between the system and the environment. Factors that change the environment also affect an open system. Neuman’s systems theory (2011) defines a total-person model of wholism and an open-systems approach. A closed system such as a chemical reaction within a test tube does not interact with the environment.
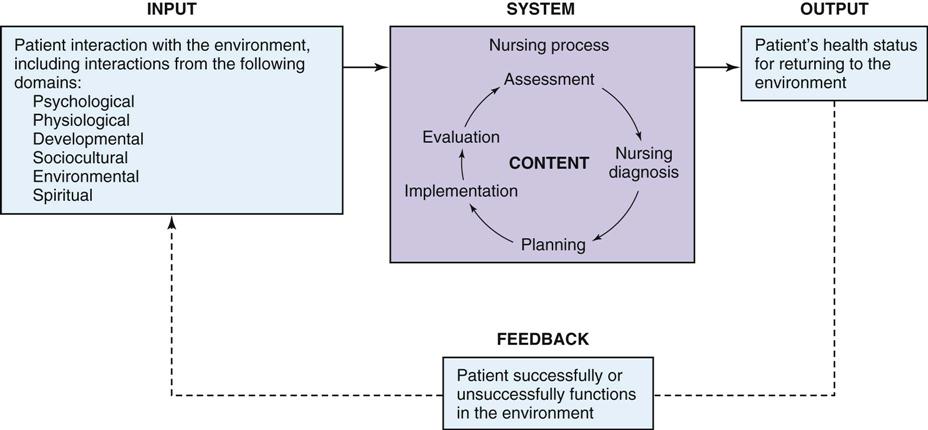
Like all systems, the nursing process has a specific purpose or goal (see Unit 3). The goal of the nursing process is to organize and deliver patient-centered care. As a system the nursing process has the following components: input, output, feedback, and content (Fig. 4-2). Input for the nursing process is the data or information that comes from a patient’s assessment (e.g., how the patient interacts with the environment and the patient’s physiological function). Output is the end product of a system; and in the case of the nursing process it is whether the patient’s health status improves, declines, or remains stable as a result of nursing care.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


