Documentation and Informatics
Objectives
• Describe methods for interdisciplinary communication within the health care team.
• Identify purposes of a health care record.
• Discuss legal guidelines for documentation.
• Identify ways to maintain confidentiality of electronic and written records.
• Describe five quality guidelines for documentation and reporting.
• Discuss the relationship between documentation and financial reimbursement for health care.
• Describe the different methods used in record keeping.
• Discuss the advantages of standardized documentation forms.
• Identify elements to include when documenting a patient’s discharge plan.
• Identify the important aspects of home care and long-term care documentation.
• Describe the purpose and content of a hand-off report.
• Explain when to take and how to verify telephone orders.
• Discuss the relationship between informatics and quality health care.
• Describe the advantages of a nursing information system.
Key Terms
Accreditation, p. 349
Acuity records, p. 356
Case management, p. 355
Charting by exception (CBE), p. 354
Clinical decision support system (CDSS), p. 360
Computerized provider order entry (CPOE), p. 361
Consultations, p. 349
Critical pathways, p. 355
DAR, p. 354
Diagnosis-related group (DRG), p. 350
Documentation, p. 348
Electronic health record (EHR), p. 353
Electronic medical record (EMR), p. 353
Firewall, p. 361
Flow sheets, p. 356
Focus charting, p. 354
Hand-off reports, p. 357
Health informatics, p. 359
Incident (occurrence) report, p. 358
Information technology (IT), p. 359
Kardex, p. 356
Nursing informatics, p. 359
PIE, p. 354
Problem-oriented medical record (POMR), p. 353
Referrals, p. 349
SOAP, p. 354
SOAPIE, p. 354
Source record, p. 354
Standardized care plans, p. 356
Variances, p. 355
![]()
Documentation is anything written or printed on which you rely as record or proof of patient actions and activities. Documentation in a patient’s medical record is a vital aspect of nursing practice. Nursing documentation must be accurate, comprehensive, and flexible enough to retrieve clinical data, maintain continuity of care, track patient outcomes, and reflect current standards of nursing practice. Information in the patient record provides a detailed account of the level of quality of care delivered to patients. Effective documentation ensures continuity of care, saves time, and minimizes the risk of errors.
There are several documentation systems for recording patient data. Regardless whether documentation is entered electronically or on paper, as a member of the health care team you communicate information about patients in an accurate, timely, and effective manner. The quality of patient care depends on your ability to communicate with other members of the health care team. All health care providers require the same information about patients to develop an organized, comprehensive plan of care. When a plan is not communicated to all members of the health care team, care becomes fragmented, tasks are repeated, and often delays or omissions in therapy occur.
The health care environment creates many challenges for accurately documenting and reporting the care delivered to patients. The quality of care, the standards of regulatory agencies and nursing practice, the reimbursement structure in the health care system, and legal guidelines make documentation and reporting an extremely important responsibility of a nurse. Whether the transfer of patient information occurs through verbal reports, written documents, or electronically, you need to follow basic principles to maintain confidentiality of information.
Confidentiality
Nurses are legally and ethically obligated to keep information about patients confidential. They may not discuss a patient’s examination, observation, conversation, diagnosis, or treatment with other patients or staff not involved in the patient’s care. Only staff directly involved in a patient’s care have legitimate access to the records. Patients frequently request copies of their medical records, and they have the right to read them. Each institution has policies to control the manner for sharing records. In most situations patients are required to give written permission for release of medical information.
Legislation to protect patient privacy for health information, the Health Insurance Portability and Accountability Act (HIPAA), governs all areas of patient information and management of that information. To eliminate barriers that could delay access to care, providers are required to notify patients of their privacy policy and make a reasonable effort to obtain written acknowledgment of this notification. HIPAA requires that disclosure or requests regarding health information are limited to the minimum necessary. This includes only the specific information required for a particular purpose. For example, if you need a patient’s home telephone number to reschedule an appointment, access to the medical records is limited solely to telephone information.
Sometimes nurses use health care records for data gathering, research, or continuing education. As long as a nurse uses a record as specified and permission is granted, this is permitted. When you are a student in a clinical setting, confidentiality and compliance with HIPAA are part of professional practice. You can review your patients’ medical records only for information needed to provide safe and effective patient care. For example, when you are assigned to care for a patient, you need to review the patient’s medical record and plan of care. You do not share this information with classmates (except for clinical conferences) and do not access the medical records of other patients on the unit. Access to electronic health records is traceable through user log-in information. Not only is it unethical to view medical records of other patients, but breaches of confidentiality can lead to disciplinary action by employers and dismissal from work or nursing school. To protect patient confidentiality, ensure that written or electronic materials used in your student clinical practice do not include patient identifiers (e.g., room number, date of birth, demographic information) and never print material from an electronic health record for personal use.
Standards
Within a health care organization there are standards that govern the type of information you document and for which you are accountable. Institutional standards or policies often dictate the frequency of documentation such as how often you record a nursing assessment or a patient’s level of pain. Know the standards of your health care organization to ensure complete and accurate documentation. Nurses are expected to meet the standard of care for every nursing task they perform. Patient records can be used as evidence in a court of law if standards are not met (ANA, 2005).
In addition, your documentation needs to conform to the standards of the National Committee for Quality Assurance (NCQA) and accrediting bodies such as The Joint Commission (TJC) to maintain institutional accreditation and minimize liability. Usually an organization incorporates accreditation standards into its policies and revises documentation forms to suit these standards. Current documentation standards require that all patients admitted to a health care facility have an assessment of physical, psychosocial, environmental, self-care, knowledge level, and discharge planning needs. TJC standards require that your documentation be within the context of the nursing process, including evidence of patient and family teaching and discharge planning (TJC, 2011). Other standards such as HIPAA include those directed by state and federal regulatory agencies and are enforced through the Department of Justice and the Centers for Medicare and Medicaid Services (ANA, 2005).
Interdisciplinary Communication within the Health Care Team
Patient care requires effective communication among members of the health care team. Effective communication takes place along two approaches. A patient’s record or chart is a confidential, permanent legal documentation of information relevant to his or her health care. The record is a continuing account of the patient’s health care status and is available to all members of the health care team. All records contain the following information:
• Patient identification and demographic data
• Informed consent for treatment and procedures
• Nursing diagnoses or problems and nursing or interdisciplinary care plan
• Record of nursing care treatment and evaluation
• Medical and health discipline progress notes
• Physical assessment findings
• Summary of operative procedures
Reports are oral, written, or audiotaped exchanges of information among caregivers. Common reports given by nurses include change-of-shift reports, telephone reports, hand-off reports, and incident reports. A health care provider calls a nursing unit to receive a verbal report on a patient’s condition. The laboratory submits a written report providing the results of diagnostic tests and often notifies the nurse by telephone if results are critical.
Team members communicate information through discussions or conferences. For example, a discharge planning conference involves members of all disciplines (e.g., nursing, social work, dietary, medicine, and physical therapy) who meet to discuss the patient’s progress toward established discharge goals. Consultations are another form of discussion in which one professional caregiver gives formal advice about the care of a patient to another caregiver. For example, a nurse caring for a patient with a chronic wound consults with a wound care specialist. Nurses document referrals (an arrangement for services by another care provider), consultations, and conferences in a patient’s permanent record to allow all caregivers to plan care accordingly.
Purposes of Records
The patient record is a valuable source of data for all members of the health care team. Its purposes include communication, legal documentation, financial billing, education, research, and auditing/monitoring.
Communication
The patient’s record is one way that health care team members communicate patient needs and progress, individual therapies, content of consultations, patient education, and discharge planning. The plan of care needs to be clear to anyone reading the chart (see Unit 3). The record is the most current and accurate continuous source of information about a patient’s health care status. Information communicated in the patient’s record allows health care providers to know a patient thoroughly, facilitating safe, effective, and timely patient-centered decisions. To enhance communication and promote safe patient care, you base communication on assessment findings and document patient information as you provide care (e.g., immediately after providing a nursing intervention or completing a patient assessment).
Legal Documentation
Accurate documentation is one of the best defenses for legal claims associated with nursing care (see Chapter 23). To limit nursing liability nursing documentation must indicate clearly that a patient received individualized, goal-directed nursing care based on the nursing assessment. The record must describe exactly what happened to a patient and follow agency standards. This is best achieved when you chart immediately after providing care. Even though nursing care may have been excellent, in a court of law “care not documented is care not provided.”
Common charting mistakes that result in malpractice include: (1) failing to record pertinent health or drug information, (2) failing to record nursing actions, (3) failing to record that medications have been given, (4) failing to record drug reactions or changes in patients’ conditions, (5) writing illegible or incomplete records, and (6) failing to document discontinued medications. Table 26-1 provides guidelines for legally sound documentation.
TABLE 26-1
Legal Guidelines for Recording
| GUIDELINES | RATIONALE | CORRECT ACTION |
| Do not erase, apply correction fluid, or scratch out errors made while recording. | Charting becomes illegible: it appears as if you were attempting to hide information or deface a written record. | Draw single line through error, write word error above it, and sign your name or initials and date it. Then record note correctly. |
| Do not document retaliatory or critical comments about patient or care by other health care professionals. Do not enter personal opinions. | Statements can be used as evidence for nonprofessional behavior or poor quality of care. | Enter only objective and factual observations of patient’s behavior; quote all patient comments. |
| Correct all errors promptly. | Errors in recording can lead to errors in treatment or may imply an attempt to mislead or hide evidence. | Avoid rushing to complete charting; be sure that information is accurate and complete. |
| Record all facts. | Record must be accurate, factual, and objective. | Be certain entry is factual and thorough. A person reading the documentation should be able to determine that patient had adequate care. |
| Do not leave blank spaces in nurses’ notes. | Another person can add incorrect information in space. | Chart consecutively, line by line; if space is left, draw line horizontally through it and sign your name at end. |
| Record all written entries legibly and in black ink. Do not use felt-tip pens or erasable ink. | Illegible entries can be misinterpreted, causing errors and lawsuits; ink from felt-tip pen smudges or runs when wet and may destroy documentation; erasures are not permitted in patient charting; black ink is more legible when records are photocopied or scanned. | Never erase entries or use correction fluid and never use pencil. |
| If an order is questioned, record that clarification was sought. | If you perform order known to be incorrect, you are just as liable for prosecution as the health care provider. | Do not record “physician made error.” Instead, chart that “Dr. Smith was called to clarify order for analgesic.” Include the date and time of phone call, with whom you spoke, and the outcome. |
| Chart only for yourself. | You are accountable for information that you enter into a patient’s record. | Never chart for someone else (exception: if caregiver has left unit for day and calls with information that needs to be documented; include date and time of entry and reference specific date and time to which you are referring and name of source of information in entry; include that information was provided via telephone). |
| Avoid using generalized, empty phrases such as “status unchanged” or “had good day.” | This type of documentation is subjective and does not reflect patient assessment. | Use complete, concise descriptions of care so documentation is objective and factual. |
| Begin each entry with date and time and end with your signature and title. | This guideline ensures that correct sequence of events is recorded; signature documents who is accountable for care delivered. | Do not wait until end of shift to record important changes that occurred several hours earlier; be sure to sign each entry (e.g., Mary Marcus, RN). |
| For computer documentation keep your password to yourself. | This maintains security and confidentiality. | Once logged into computer, do not leave computer screen unattended. Log out when you leave the computer. Make sure that computer screen is not accessible for public viewing. |
Reimbursement
Diagnosis-related groups (DRGs) are the basis for establishing reimbursement for patient care. A DRG is a classification based on patients’ medical diagnoses. Hospitals are reimbursed a predetermined dollar amount by Medicare for each DRG. Detailed recording establishes diagnoses for determining a DRG. Your documentation clarifies the type of treatment a patient receives and supports reimbursement to the health care agency.
A medical record audit reviews financial charges used in the patient’s care. Private insurance carriers and auditors from federal agencies review records to determine the reimbursement that a patient or a health care agency receives. Accurate documentation of supplies and equipment used assists in accurate and timely reimbursement.
Education
A patient’s record contains a variety of information, including diagnoses, signs and symptoms of disease, successful and unsuccessful therapies, diagnostic findings, and patient behaviors. One way to learn the nature of an illness and the individual patient’s response to it is to read the patient care record. No two patients have identical records, but you can identify patterns of information in records of patients who have similar health problems. With this information you learn to anticipate the type of care required for a patient.
Research
After obtaining appropriate agency approvals, nurse researchers often use patients’ records for research studies to gather statistical data on the frequency of clinical disorders, complications, use of specific medical and nursing therapies, recovery from illness, and deaths. Researchers also use this information to investigate nursing interventions or health problems. For example, a nurse wants to compare a new method of pain control with a standard pain protocol using two groups of patients. The records provide data on the two types of interventions: the new method and the standard pain control. The nurse researcher collects data from the records that describe the type and dose of analgesic medications used, objective assessment data, and patients’ subjective reports of pain relief. The researcher then compares the findings to determine if the new method was more effective than the standard pain control protocol. Analysis of the data contributes to evidence-based nursing practice and quality health care (see Chapter 5).
Auditing and Monitoring
Hospitals establish quality improvement programs for conducting objective, ongoing reviews of patient care. Quality improvement programs keep nurses informed of standards of nursing practice to maintain excellence in nursing care. Accrediting agencies such as TJC (2011) require quality improvement programs and set standards for the information located in a patient’s record, including indications that a plan of care is developed with the patient as a participant and that discharge planning and patient education have occurred. Institutions and accrediting groups establish standards for quality care. Nurses audit records throughout the year to determine the degree to which standards of care are met and identify areas needing improvement and staff development (see Chapter 5). Nurses share deficiencies identified during monitoring with all members of the nursing staff to make changes in policy or practice.
Guidelines for Quality Documentation and Reporting
High-quality documentation and reporting are necessary to enhance efficient, individualized patient care. Quality documentation and reporting have five important characteristics: they are factual, accurate, complete, current, and organized.
Factual
A factual record contains descriptive, objective information about what a nurse sees, hears, feels, and smells. An objective description is the result of direct observation and measurement. For example, “B/P 80/50, patient diaphoretic, heart rate 102 and regular.” Avoid vague terms such as appears, seems, or apparently because these words suggest that you are stating an opinion, do not accurately communicate facts, and do not inform another caregiver of the details regarding the behaviors exhibited by a patient. Objective documentation includes observations of a patient’s behaviors. For example, instead of documenting “the patient seems anxious,” provide objective signs of anxiety and document “the patient’s pulse rate is elevated at 110 beats/min, respiratory rate is slightly labored at 22 breaths/min, and the patient reports increased restlessness.”
The only subjective data included in the record are what the patient says. When recording subjective data, document the patient’s exact words within quotation marks whenever possible. For example, when he or she exhibits anxiety, you record, “Patient states, ‘I feel very nervous.’ ” Include objective data to support subjective data so your charting is as descriptive as possible.
Accurate
The use of exact measurements establishes accuracy. For example, a description such as “Intake, 360 mL of water” is more accurate than “Patient drank an adequate amount of fluid.” Charting that an abdominal wound is “5 cm in length without redness, drainage, or edema” is more descriptive than “large wound healing well.” Accurate measurements help you determine if a patient’s condition has changed.
Documentation of concise data is clear and easy to understand. It is essential to avoid the use of unnecessary words and irrelevant detail. For example, the fact that the patient is watching television is only necessary when this activity is significant to the patient’s status and plan of care.
To ensure patient safety use abbreviations carefully to avoid misinterpretation. TJC’s “do not use” list of abbreviations (see Chapter 31) is used by all health care providers to promote patient safety. In addition, TJC (2011) requires that health care institutions develop a list of standard abbreviations, symbols, and acronyms to be used by all members of the health care team when documenting or communicating patient care and treatment. To minimize errors spell out abbreviations in their entirety when they become confusing.
Correct spelling demonstrates a level of competency and attention to detail. Many terms can easily be misinterpreted (e.g., dysphagia or dysphasia and dram or gram). Some spelling errors result in serious treatment errors (e.g., the names of certain medications such as Lamictal and Lamisil or morphine and Numorphan are similar). Transcribe such terms carefully to ensure that the patient receives the correct medication.
All entries in medical records must be dated, and there must be a method to identify the authors of all entries (TJC, 2011). Each entry in a patient’s record ends with the caregiver’s full name or initials and status such as “Jane Woods, RN.” When initials are used, the full name and status of the individual are found in the medical record to allow others to readily identify the individual. As a nursing student, enter your full name and nursing student (NS) abbreviation, such as “David Jones, NS. The abbreviation for nursing student varies between NS for nursing student or SN for student nurse. Include your educational institution when required by agency policy.
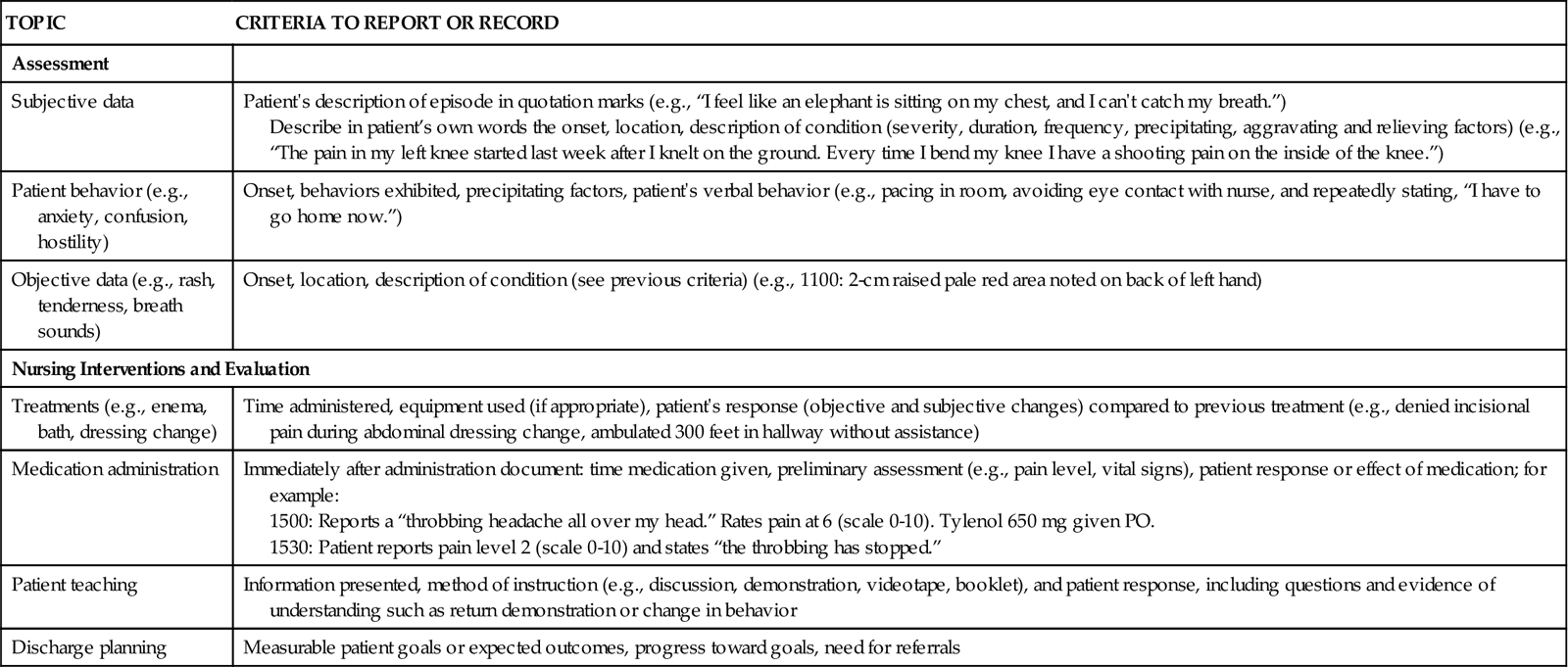
Complete
The information within a recorded entry or a report must be complete, containing appropriate and essential information. Criteria for thorough communication exist for certain health problems or nursing activities (Table 26-2). Your written entries in a patient’s medical record describe the nursing care you administer and the patient’s response. An example of a thorough nurse’s note follows:
TABLE 26-2
Examples of Criteria for Reporting and Recording
| TOPIC | CRITERIA TO REPORT OR RECORD |
| Assessment | |
| Subjective data | Patient’s description of episode in quotation marks (e.g., “I feel like an elephant is sitting on my chest, and I can’t catch my breath.”) Describe in patient’s own words the onset, location, description of condition (severity, duration, frequency, precipitating, aggravating and relieving factors) (e.g., “The pain in my left knee started last week after I knelt on the ground. Every time I bend my knee I have a shooting pain on the inside of the knee.”) |
| Patient behavior (e.g., anxiety, confusion, hostility) | Onset, behaviors exhibited, precipitating factors, patient’s verbal behavior (e.g., pacing in room, avoiding eye contact with nurse, and repeatedly stating, “I have to go home now.”) |
| Objective data (e.g., rash, tenderness, breath sounds) | Onset, location, description of condition (see previous criteria) (e.g., 1100: 2-cm raised pale red area noted on back of left hand) |
| Nursing Interventions and Evaluation | |
| Treatments (e.g., enema, bath, dressing change) | Time administered, equipment used (if appropriate), patient’s response (objective and subjective changes) compared to previous treatment (e.g., denied incisional pain during abdominal dressing change, ambulated 300 feet in hallway without assistance) |
| Medication administration | Immediately after administration document: time medication given, preliminary assessment (e.g., pain level, vital signs), patient response or effect of medication; for example: 1500: Reports a “throbbing headache all over my head.” Rates pain at 6 (scale 0-10). Tylenol 650 mg given PO. 1530: Patient reports pain level 2 (scale 0-10) and states “the throbbing has stopped.” |
| Patient teaching | Information presented, method of instruction (e.g., discussion, demonstration, videotape, booklet), and patient response, including questions and evidence of understanding such as return demonstration or change in behavior |
| Discharge planning | Measurable patient goals or expected outcomes, progress toward goals, need for referrals |
1915 Verbalizes sharp, throbbing pain localized along lateral side of right ankle, beginning approximately 15 minutes ago after twisting his foot on the stairs. Rates pain as 8 on a scale of 0-10. Pain increased with movement, slightly relieved with elevation. Pedal pulses equal bilaterally. Right ankle circumference 1 cm larger than left. Bilateral lower extremities warm, pale pink, skin intact, responds to tactile stimulation and capillary refill less than 3 seconds. Ice applied to right ankle. Percocet 2 tabs (PO) given for pain. States pain somewhat relieved with ice, rates pain as 6 on a scale of 0-10. Dr. M. Smith notified. Lee Turno, RN
1945 Rates pain as a 3 on a scale of 0-10. States, “The pain medication really helped.” Lee Turno, RN
You frequently use flow sheets or graphic records when documenting routine activities such as daily hygiene care, vital signs, and pain assessments. Describe these data in greater detail when they are relevant such as when a change in functional ability or status occurs. For example, if your patient’s blood pressure, pulse, and respirations are elevated above expected values following a walk down the hall, document additional description about the patient’s status and response to the walk in the appropriate place in the medical record (e.g., nurse’s notes).
Current
Timely entries are essential in a patient’s ongoing care. Delays in documentation lead to unsafe patient care. To increase accuracy and decrease unnecessary duplication, many health care agencies keep records or computers near a patient’s bedside to facilitate immediate documentation of information as it is collected from a patient. Document the following activities or findings at the time of occurrence:
• Administration of medications and treatments
• Preparation for diagnostic tests or surgery, including preoperative checklist
• Change in patient’s status and who was notified (e.g., physician, manager, patient’s family)
• Admission, transfer, discharge, or death of a patient
• Treatment for sudden change in patient’s status
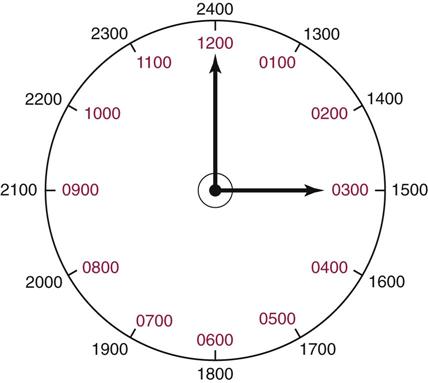
Most health care agencies use military time, a 24-hour system that avoids misinterpretation of AM and PM times (Fig. 26-1). Instead of two 12-hour cycles in standard time, the military clock is one 24-hour time cycle. The military clock ends with midnight at 2400 and begins at 1 minute after midnight as 0001. For example, 10:22 AM is 1022 military time; 1:00 PM is 1300 military time.
Organized
Communicate information in a logical order. It is also more effective when notes are concise, clear, and to the point. To document notes about complex situations in an organized fashion think about the situation and make a list of what you need to include before beginning to enter data in the medical record. Applying critical thinking skills and the nursing process gives logic and order to nursing documentation. For example, an organized entry describes the patient’s pain, your assessment and interventions, and the patient’s response. Use the nursing process to give logic and organization to your documentation.
Methods of Documentation
There are several documentation systems for recording patient data. Regardless whether documentation is entered electronically or on paper, each health care agency selects a documentation system that reflects its philosophy of nursing. The same system is used throughout a specific agency and may be used throughout a health care system as well.
Paper and Electronic Health Records
Traditionally health care professionals documented on paper medical records. Paper records are episode oriented, with a separate record for each patient visit to a health care agency (Hebda et al., 2009). Key information such as patient allergies, current medications, and complications from treatment may be lost from one episode of care (e.g., hospitalization or clinic visit) to the next, jeopardizing a patient’s safety.
To enhance communication among health care providers and thus patient safety, the American Recovery and Reinvestment Act of 2009 set a goal that all medical records will be kept electronically as of 2014. Many professional organizations and accrediting body initiatives also support initiation of the electronic health record (EHR). The EHR is an electronic record of patient health information generated whenever a patient accesses medical care in any health care delivery setting (HIMSS, 2003). Although the electronic medical record (EMR) contains patient data gathered in a health care setting at a specific time and place and is a part of the EHR, the two terms are frequently used interchangeably (Garets and Davis, 2005; Hebda et al., 2009).
The EHR provides access to a patient’s health record information at the time and place that clinicians need it. A unique feature of an EHR is its ability to integrate all pertinent patient information into one record, regardless of the number of times a patient enters a health care system. An EHR also includes results of diagnostic studies that may include images and sound and decision support software programs. Because an unlimited number of patient records potentially can be stored within an EHR system, health care providers can access clinical data to identify quality issues, link interventions with positive outcomes, and make evidence-based decisions.
The EHR improves continuity of health care from one episode of illness to another. A clinician accesses relevant and timely information about a patient and focuses on the priority problems of care to make timely, well-informed clinical decisions. An EHR is a powerful tool because of the decision support resources it contains. For example, in a hospital setting an EHR gathers data and performs checks to support regulatory and accreditation requirements. An EHR includes tools to guide and critique medication administration (see Chapter 31) and basic decision support tools such as physician order sets and interdisciplinary treatment plans.
The ultimate development of an EHR for all patients will affect the entire health care community. Currently the American Medical Association, American Nurses Association, the HIMSS, and the American Medical Informatics Association are just some of the organizations gathering information from health care professionals to support the adoption of EHR standards (Hebda et al., 2009). All disciplines and health care organizations will benefit from the implementation of an EHR. The key advantages of an EHR for nursing include providing a means to compare ongoing clinical data about a patient with original baseline information and maintaining an ongoing record of a patient’s health education. In addition, the EHR offers easier access to quality data for research and automates evidence-based guidelines.
Narrative Documentation
Narrative documentation is the traditional method for recording nursing care. It is simply the use of a story-like format to document information specific to patient conditions and nursing care. However, narrative charting has many disadvantages, including the tendency to be repetitious and time consuming and to require the reader to sort through much information to locate desired data (Box 26-1).