Chapter 20
The Pregnant Patient1
It was the best of times, it was the worst of times … .
Charles Dickens (1812–1870)
General Considerations
As of 2008, the average birth rate for the world was 20.2 live births per year per 1000 total population, which for a world population of 6.6 billion amounts to 134 million babies born per year. In 2010, in the United States, the birth rate was 13 per 1000 total population. The lower birth rate in the United States reflects primarily the current smaller proportion of women of childbearing age as baby boomers age and Americans live longer. The fertility rate was 64.1 births per 1000 women aged 15 to 44 years.
The lowest birth rates worldwide, less than 8.5 per 1000, were recorded in Japan, Germany, Singapore, Hong Kong, and Macao. The highest birth rates, 49 or more per 1000, were recorded in Niger, Liberia, Guinea-Bissau, and Democratic Republic of the Congo.
In 2010, 3,999,386 births were reported to United States residents, 3% less than in 2009 (4,130,665). The number of births declined for nearly all race and Hispanic origin groups. The general fertility rate was 64.1 births per 1000 U.S. women aged 15 to 44, down 3% from 2009 (66.2). The total fertility rate (estimated number of births in a woman’s lifetime) was 1931 births per 1000 women in 2010, a 4% decline from 2009 (2002).
Childbearing among teenagers has been on a long-term decline in the United States since the late 1950s, except for a brief, but steep, climb in the late 1980s through 1991. The birth rate for United States teenagers aged 15 to 19 fell 10% in 2010, to 34.2 per 1000, reaching the lowest level reported in the United States in seven decades. The number of live births to 15 to 19 year olds was 367,678. Rates declined for teen subgroups aged 10 to 14, 15 to 17, and 18 to 19 and for all race and Hispanic origin groups.
In 2010, the mean age of mother at first birth increased to 25.4 years from 25.2 in 2009. The mean age rose for nearly all race and Hispanic origin groups. The cesarean delivery rate decreased slightly to 32.8% of all births in 2010, the first decline in this rate since 1996. The cesarean rate rose nearly 60% from 1996 to 2009.
Slightly more than 1 per 10 women smoked during pregnancy in 2010, a decline of 44% since these data were first collected in 1989.
Any woman in the reproductive age group who is sexually active and misses her menstrual period should be considered pregnant until proven otherwise. Even if she presents with symptoms not directly related to the abdomen, she should be evaluated for pregnancy. A sexually active woman in the reproductive age group may have a history of amenorrhea (loss of menstrual periods) but can be pregnant nonetheless. Whatever the previous cause of amenorrhea, it may be different now. “Think pregnancy” should be your motto in the evaluation of such patients. This is extremely important because the diagnosis or treatment of a woman’s medical or surgical problem may affect the developing fetus if she is pregnant. As discussed later in this chapter, many of the symptoms of pregnancy are nonspecific and can be interpreted erroneously if the pregnancy is not recognized. For example, the urinary frequency that is common in early pregnancy might easily be mistaken for cystitis. The patient might then receive an antibacterial agent such as a sulfonamide or a quinolone, which is not the best choice for the developing fetus. When the urinary symptoms fail to respond to the medication, the patient might then be referred for intravenous pyelography, which adds the risk of radiation to an early pregnancy.
Structure and Physiologic Characteristics
The anatomy and the physiologic changes related to the menstrual cycle that occur in the nonpregnant woman have already been discussed. This chapter reviews the physiologic alterations resulting from pregnancy and the functional pelvic anatomy.
Basic Physiologic Characteristics of Reproduction
When semen is deposited in the vagina, sperm travel through the cervix and uterus and into the fallopian tubes, where fertilization may occur if an ovum is present. The majority of sperm deposited in the vagina die within 1 to 2 hours because of the normal acidic environment. The sperm are aided in their travel into the fallopian tubes by uterine and tubal contractions and favorable mucous conditions.
The fertilized ovum, or zygote, remains in the fallopian tube for approximately 3 days. While in the tube, the fertilized ovum divides repeatedly to form a round mass of cells called the morula. If there is an obstruction in the fallopian tube, the fertilized ovum may become trapped in the tube and attach itself to the lining of the tube, giving rise to an ectopic, or tubal, pregnancy. In a normal pregnancy, approximately 6 to 8 days after fertilization, the morula becomes a blastocyst, which migrates through the tube into the uterus, where it attaches itself to the endometrium (implantation), with the inner cell mass adjacent to the endometrial surface. Substances that destroy the surface epithelial cells are released, allowing the blastocyst to burrow into the endometrium. The endometrium then grows over the invading blastocyst.
The primitive chorion, the combination of trophoblast and primitive mesoderm, secretes a luteinizing hormone known as human chorionic gonadotropin (hCG), which controls the corpus luteum and inhibits pituitary gonadotropic activity. Quickly thereafter, as the invasion proceeds, maternal venous blood vessels are tapped to form lakes of blood, and chorionic villi develop. These can be identified as early as the twelfth day after fertilization. These villi develop a leafy appearance and are called the chorion frondosum. By the fifteenth day after fertilization, the maternal arterial vessels are tapped, and by the seventeenth to eighteenth day, a functioning placental circulation is established. At term, the uteroplacental blood flow is estimated to be approximately 550 to 705 mL/minute. Figure 20-1A illustrates the path of sperm, fertilization, and implantation.
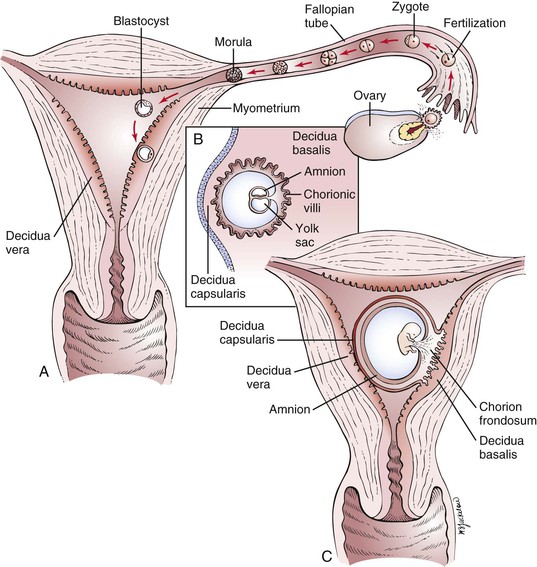
Figure 20–1 A, Fertilization and implantation. B and C, Cross-sectional view through the uterus of a pregnant woman at approximately 8 days and 20 days, respectively.
Decidua is the name given to the endometrium of pregnancy. There are three types, distinguished by location with regard to the growing embryo. The decidua capsularis is the overlying endothelium that covers the conceptus, and the decidua basalis is the decidual tissue lying between the blastocyst and the myometrium. The decidua of the remainder of the endometrial cavity is the decidua vera. A cross section through the uterus of a pregnant woman and the different types of decidua in early pregnancy are illustrated in Figure 20-1B and C.
One of the first placental hormones produced by the developing trophoblastic tissue is hCG. This hormone is present as early as the eighth day after fertilization has taken place. The titers increase to a maximal level by about the sixtieth to seventieth days after fertilization and then decrease. The primary function of hCG is to maintain the corpus luteum during the first 2 months of pregnancy until the placenta can produce enough progesterone by itself. Other hormones, such as human placental lactogen, human chorionic thyrotropin, and adrenocorticotropic hormone, and estrogens are also produced by the placenta. It is beyond the scope of this book to discuss the actions of these hormones; the reader is referred to the online references for this chapter for further information.
Functional Anatomy of Birth
The pelvic cavity is bounded above by the plane of the brim (the inner sacral promontory to the upper and inner borders of the symphysis pubis), below by the plane of the outlet (the lower and inner borders of the symphysis pubis to the end of the sacrum or coccyx), posteriorly by the sacrum, laterally by the sacrosciatic ligaments and ischial bones, and anteriorly by the pubic rami.
The birth canal, through which the infant is delivered, may be thought of as a cylindric passage with walls composed partially of hard parts (the bony pelvis) and partially of soft parts (the muscles of the pelvic floor and the pelvic ligaments). The cross section of the cylinder is oval, rather than circular, to accommodate the oval cross section of the entering fetal part (e.g., the head) as it descends through the pelvis as a result of the expulsive effect of uterine contractions.
This mechanism for delivery and its corresponding anatomy would be easily understood were it not for the fact that the long axis of the schematic oval, which lies transversely at the entrance to the pelvis, comes to lie in the anteroposterior axis in the midpelvis. The entering fetal part must therefore descend in a spiral path as it progresses through the birth canal.
The process of birth varies greatly, depending on the relationships—lie, presentation, attitude, and position—of the fetus to the maternal anatomy. It is important to define these relationships accurately to understand the birth process.
The term lie refers to the relation of the long axis of the fetus to that of the mother. In more than 99% of full-term pregnancies, the lie is in the same plane as or parallel to the long axis of the mother; this is called a longitudinal lie. In rare instances, the long axis of the fetus is perpendicular to the maternal pelvis; this is called a transverse lie.
The term presentation refers to the part of the fetus in the lower pole of the uterus overlying the pelvic brim (e.g., cephalic, vertex, breech) that can be felt through the cervix. Usually the fetus’s head is flexed so that the chin is in contact with the chest. In this case, the occipital fontanelle is the presenting part, and the presentation is referred to as a vertex presentation. The fetus is in the occiput or vertex presentation in approximately 95% of all labors.
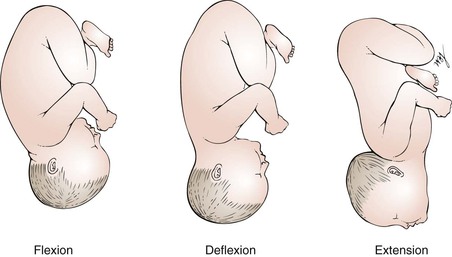
The attitude, or habitus, of the fetus is the posture of the fetus: flexion, deflexion, or extension. Figure 20-2 illustrates these postures. In most cases, the fetus becomes bent over so that the back is convex, the head is sharply flexed on the chest, the thighs are flexed over the abdomen, and the legs are bent at the knees. This is the description of the fetal attitude of flexion.
The position is the relationship of an arbitrarily chosen portion of the presenting part of the fetus to the maternal pelvis. For example, in a vertex presentation, the chosen portion is the fetal occiput; in a breech presentation, it is the sacrum; and in a face presentation, it is the chin, termed the mentum. The maternal pelvis is divided into eight parts for the purpose of further defining position. These divisions are shown in Figure 20-3.
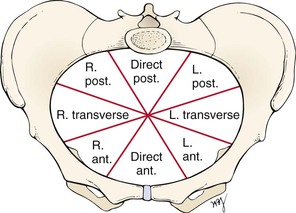
Figure 20–3 Divisions of maternal pelvis as seen from above. ant., Anterior; L., left; post., posterior; R., right.
Because the arbitrarily chosen portion of the presenting part may be either left or right, the portion can be described as left occiput (LO), right occiput (RO), left sacral (LS), right sacral (RS), left mental (LM), or right mental (RM). This part is also directed anteriorly (A), posteriorly (P), or transversely (T). For each of the three presentations (vertex, breech, and face), there are therefore six varieties of position. For example, in a vertex presentation, if the occiput is in the left anterior segment of the maternal pelvis, the position is described as left occiput anterior (LOA), which is the most common of all vertex presentations. The common clinical vertex positions are illustrated in Figure 20-4. Left and right always denote the side of the mother. Likewise, anterior, posterior, and transverse refer to the mother’s pelvis.
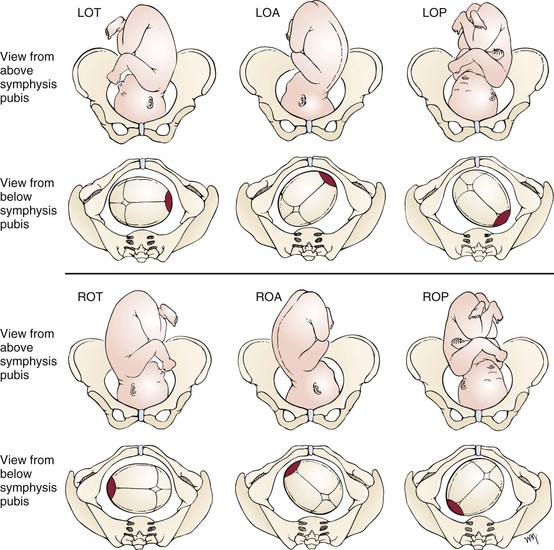
Figure 20–4 Common clinical vertex positions. For each position shown, the top diagram is the view from above the symphysis pubis; the bottom is the view from below the symphysis pubis. Right and left refer to the mother’s side. Anterior, posterior, and transverse refer to the maternal pelvis. Red area is the fetal occiput. LOA, Left occiput anterior; LOP, left occiput posterior; LOT, left occiput transverse; ROA, right occiput anterior; ROP, right occiput posterior; ROT, right occiput transverse.
The term station characterizes the level of descent of the presenting part of the fetus; “0 station” signifies that the fetal occiput has reached the level of the maternal ischial spines and that the widest transverse part of the infant’s head (biparietal diameter) is at the level of the pelvic brim. This is also known as engagement. If the vertex is at “−1 station,” it means that the fetal occiput is at a plane 1 cm above the level of the maternal ischial spines (and that the biparietal diameter is therefore 1 cm above the pelvic brim), and the infant’s head is therefore not engaged.
The cardinal movements of labor are engagement, descent, flexion, internal rotation, extension, external rotation, and expulsion.
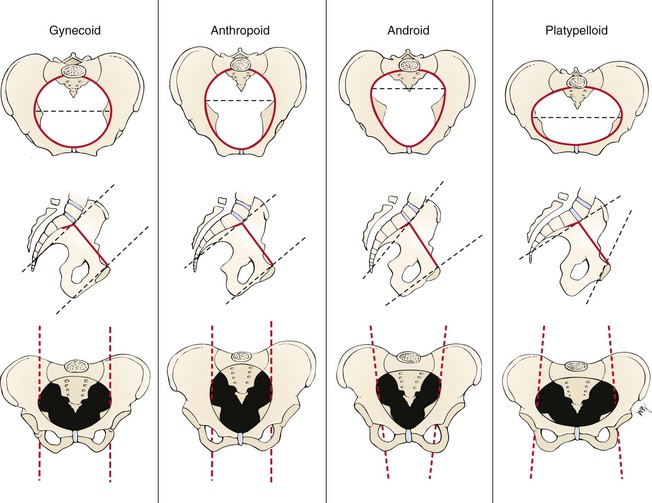
There are four basic pelvic configurations: gynecoid, anthropoid, android, and platypelloid. These are based on the shape of the brim, midpelvis, and outlet. Any pelvis is likely to combine features of more than one configuration. Figure 20-5 illustrates these basic types and summarizes the differences in pelvic anatomy.
Review of Specific Symptoms
The most common symptoms of pregnancy are the following:
Amenorrhea
Amenorrhea results from the high levels of estrogen, progesterone, and hCG, which increase and alter (decidualize) the uterine endometrium and do not allow the endometrium to slough as in menstrual bleeding.
Nausea
Nausea, with or without vomiting, is the so-called morning sickness of pregnancy. As the name implies, the symptom is usually worse during the early part of the day and usually passes in a few hours, although it may last longer. More than 50% of all pregnant women in their first trimester have gastrointestinal symptoms. Although the cause is unknown, high levels of estrogen and hCG have been implicated in its development. Pregnant women are also hypersensitive to odors, and they may experience alterations in taste. Morning sickness usually improves after 12 to 16 weeks, when the hCG levels fall. Severe vomiting may occur, resulting in dehydration and ketosis, but this is uncommon, occurring in fewer than 2% of pregnancies.
Breast Changes
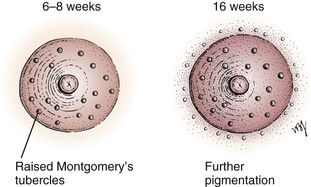
Several changes in the breast occur with pregnancy. One of the earliest symptoms is an increase in the vascularity of the breast, associated with a sensation of heaviness, almost pain. This occurs at approximately the sixth week. By the eighth week, the nipple and areola have become more pigmented, and the nipple becomes more erectile. The Montgomery tubercles become prominent as raised pinkish-red nodules on the areola. By the sixteenth week, a clear fluid called colostrum is secreted and may be expressed from the nipple. By the twentieth week, further pigmentation and mottling of the areola have developed. Figure 20-6 illustrates the changes in the nipple and areola.
Heartburn
Heartburn in pregnancy occurs because progesterone causes relaxation of the gastroesophageal sphincter. Another cause of heartburn in the third trimester is the pushing upward of the enlarged uterus. This upward displacement exerts pressure on the stomach. There is a decrease in gastric motility, as well as a decrease in gastric acid secretion, which delays digestion.
Backache
As a result of secretion of estrogen and progesterone, the pelvic joints relax, and the increased uterine weight accentuates lordosis. The abdominal muscles stretch and lose tone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree