Chapter 21
The Pediatric Patient1
Children are not like men or women; they are almost as different creatures, in many respects, as if they never were to be the one or the other; they are as unlike as buds are unlike flowers, and almost as blossoms are unlike fruits.
Walter Savage Landor (1775–1864)
General Considerations
Since the late 1920s, awareness of the importance of child health care has increased. Along with better control of infectious disease and great strides in nutrition and technology has come the recognition of the importance of the behavioral and social aspects of a child’s health. Despite the many advances and the marked reduction in infant mortality rates, the neonatal period remains a time of very high risk.2
In 2004, a total of 27,936 deaths occurred in the United States in children younger than 1 year, an infant mortality rate of 6.8 per 1000 live births; 70% of these deaths occurred in the first month after birth, almost all of those in the first week.3 Although the infant mortality rate reached a record low level of 6.14 infant deaths per 1000 live births in 2010,4 the United States still ranks poorly in this regard when compared with other industrialized countries.5
Unintentional injury and sudden infant death syndrome (SIDS) are the leading causes of infant mortality after the first month of life. SIDS is the leading cause of death among infants aged 1 to 12 months and is the third leading cause overall of infant mortality in the United States. Although the overall rate of SIDS in the United States has declined by more than 50% since 1990, thanks to the “Back to Sleep” campaign, rates have declined less among non-Hispanic African-American, and American Indian/Alaska Native infants. SIDS is defined as the sudden death of a healthy infant younger than 1 year that cannot be explained after a thorough investigation is conducted, including a complete autopsy, examination of the death scene, and review of the clinical history. Preventing SIDS remains an important public health priority. Several risk factors have been associated with SIDS, including prone sleeping, sleeping on soft surfaces, loose bedding, overheating as a result of overdressing, smoking in the home, maternal smoking during pregnancy, bed sharing, and prematurity or low birth weight. In some cases, SIDS seems to be caused by a mutation in a gene that leads to a cardiac channelopathy, resulting in prolonged QT interval and other arrhythmogenic states.
Unintentional injury remains the top killer of children aged 1 to 14 years6 ahead of cancer and birth defects. More than 5300 children in the United States died in 2004 from unintentional injuries—an average of 15 children each day. Motor vehicle occupant injury is the leading cause of injury-related death among all children after infancy. Death from airway obstruction is the leading cause of injury death for children younger than 1 year, and drowning follows motor vehicle injuries for children aged 1 to 14 years. Poverty is the primary predictor of fatal injury; male sex and race are additional factors. Native American and African-American children are the groups at highest risk; they are approximately twice as susceptible to fatal injury as are white children.
Previous chapters discussed the history and physical examination as they relate to adult patients. This chapter discusses the differences related to physical diagnosis in the pediatric age group. The field of pediatrics is broad and encompasses birth through adolescence, often defined as up to age 22. During this period, there are enormous changes in children’s emotional, social, cognitive, and physical development, all of which must be discussed thoroughly.
This chapter is organized somewhat differently from the previous chapters. The first section is devoted to the pediatric history, which is similar in most pediatric age groups but differs in important ways from the adult history. The sections that follow are devoted to the physical examinations of the following age groups:
• Neonatal period (birth to 1 month of age)
• Infancy (1 month to 1 year of age)
• Toddler and early childhood (1 to 5 years of age)
• Late childhood (6 to 12 years of age)
Most of this chapter is devoted to the first three groups because the order and techniques of examining children 6 to 22 years of age are similar to those for adults. You will note, however, that the order of the physical examination does differ from that of the adult in the younger age groups.
The reader is advised to watch the video presentation on Student Consult to review the physical examinations of the newborn and the toddler, as well as specific pointers about the neurologic assessment at these ages. The internet version also contains a demonstration of an adolescent history with a standardized patient.
The Pediatric History
The pediatric history, like the adult history, is obtained before the examination is performed. During this period, the child can get accustomed to the clinician. Unlike the adult history, however, much of the pediatric history is taken from the parent or guardian. But it can be helpful to include the child in the process. If the child is old enough, interview him or her as well.
Effective communication with the child is the key to a successful workup, just as with an adult. An infant communicates by crying and, in so doing, indicates the existence of an unmet need. Although older children can communicate through language, they also often use crying as a response to pain or to express emotional unrest. This mode of communication merits attention. Newborns can also communicate by cooing and babbling, which indicates contentment.
In infancy, children use sounds to mimic words, as well as using gestures to communicate. At approximately 10 to 12 months of age, children usually speak their first word, usually “dada” or “mama.” By 15 months of age, children are expected to say between 3 and 10 words, and by 2 years of age, their vocabulary may contain more than 200 words; it is at this age that we expect children to be able to put 2 or more words together in a phrase, such as “Juice gone” or “Up me!” By 3 years of age, children are able to put together sentences of 5 or 6 words from a 1500-word vocabulary, and should be 50% intelligible to an adult who does not know the child. By the time they are 6 years of age, they are able to communicate in longer sentences, with a vocabulary of several thousand words, and use most of the grammar of their native language. Three-year-olds can give the clinician a good idea of what hurts, where, and how it feels. The 6-year-old can give some idea of how and when the complaint started. The examiner must pay attention to everything the child says because the words used may give insight into the child’s physical, emotional, and developmental state, as well as his or her home situation and other factors in his or her environment.
An effective relationship with a child begins by engaging with him or her. Start by admiring the child’s shoes or toy; possessions are more neutral topics for the child to talk about at first than his or her own body or behavior. One of the best ways to make a child feel comfortable is through praise. When talking to a child, it is useful to say, “Thank you for holding still. That makes the examination easier.” The use of “You’re a good boy” or “You are such a sweet girl” may produce embarrassment. Therefore praise should be given for a child’s behavior or actions and not for his or her personality. Sharing a book with the child (e.g., as part of the “Reach Out and Read” program7) is another useful way to engage the toddler or preschooler. Particularly for this age group, some examiners may choose not to wear a white coat to alleviate some of the child’s fears.
It is important not to talk down to children. The examiner must assess the developmental level of the child and choose words that are appropriate to that child’s level of understanding. This is especially important in dealing with a preadolescent; in fact, when interviewing such a child, the interviewer may gain more cooperation from the child by treating him or her as a bit older than his or her actual age, rather than younger.
Although most of the history is obtained from the parent or guardian, some questions are asked of the child. There are two simple rules in asking questions of children:
Interviewers are often amazed by how well a child can respond to questions phrased according to these rules. School-aged children can respond to structured, open-ended questions. Asking “How do you like school?” may elicit only a shrug. Asking “What do you like best about school?” is likely to get the child talking. It is useful to spend time observing the child at play while interviewing a parent. It is also rewarding to allow a toddler to play with a stethoscope, tongue blade, or penlight to “make friends” with the equipment that will be used later in the physical examination.
The pediatric history consists of the following:
The chief complaint and the history of the present illness are obtained in the same manner as with the adult patient. The history should identify the informant, and the interviewer should try to establish whether and where the child has a regular source of medical care. The history of the present illness should always include information about the effect of an acute illness on the child’s oral intake, activity level, hydration status, and ability to sleep. For a chronic problem, the examiner should look for effects on the child’s growth and development.
Birth History
The past medical history section begins with the birth history. An opening with the mother such as “How was your pregnancy?” may be all that is needed to start this part of the medical history. Determine any maternal problems, medications taken, illnesses, bleeding, whether x-ray films were taken during the pregnancy, and whether the child was born “on time.” Ask the following questions:
“How old were you at the time of your child’s delivery? How old was the baby’s father?”
“How many times have you been pregnant? Have you had any miscarriages or children who died in infancy?” If yes, “Do you know the cause? Were any of your children born too early?” (Box 21-1 contains an explanation of the shorthand notation for this information.)
“How much weight did you gain during your pregnancy?”
Although testing for human immunodeficiency virus infection is not automatic, most women also accept it because therapy with antiretroviral drugs in the last trimester can reduce rates of congenital infection from 25% to less than 2%.
“How long was your labor? Were there any unusual problems with it?”
“What type of delivery did you have, vaginal or cesarean?” If cesarean, ask for the reason. Was it because of a previous cesarean birth or a problem related to this pregnancy?8
“Did the baby come out head first or feet first?”
“Were you told of any abnormalities at birth?”
“Were you told the Apgar9 scores?” If the parents don’t know, ask, “Did he cry right away? Or did the doctors need to do something to help him start breathing?”
“Did the child experience any problems in the newborn nursery, such as breathing difficulties? Jaundice? Feeding problems?”
“Did the child receive oxygen in the nursery? Antibiotics? Phototherapy?”
“After delivery, how long did the baby remain in the hospital?”
“Did the child go home with you?” If not, ask what the reason was.
“Were you told that problems were found on the newborn screening tests?”10 If yes, “What were they? Was follow-up testing performed?”
Note the order of these questions: they begin with the prenatal course, then focus on the actual birth, and then turn to the postnatal course. See the sample write-up of a newborn’s history at the end of this chapter. The amount of detail needed in the birth history depends on the age of the child and the clinical situation. Most of this information is pertinent for an infant; for a teenager, it is probably enough to know whether the child was born full term and whether there were any problems in the neonatal period.
In recent years, many babies are being born following methods of conception and delivery that were unavailable in the past. Babies might be adopted; they can be conceived via in vitro fertilization; conception may have occurred by artificial insemination using sperm provided by the rearing father or by a donor; a donor egg might have been used; the pregnancy might have been carried in the womb of the rearing mother or of a maternal surrogate. Gathering this information is important for different reasons: psychologically and emotionally, it is important to support the parents who are raising the child, regardless of whether they are the biological parents. However, genetically, it is important to obtain information about the biological parents to assess the child’s susceptibility to inherited disease. Interviews to explore inherited disorders need to be conducted with considerable tact. The parents may not want to discuss this family history in front of the child, and each parent should be offered a private interview.
Past Medical History
As with the adult, the past medical history should include details of any hospitalizations, injuries, and surgeries, as well as any medications taken on a regular basis. Ask, “Does your child have any chronic health problems?” Common chronic health problems in children include asthma, seizure disorders, eczema, recurrent ear infections or urinary tract infections, sickle cell disease, cystic fibrosis, diabetes, gastroesophageal reflux disease, and cerebral palsy. If the child was born before term, ask about late effects of preterm birth, such as chronic lung disease, nutritional problems, developmental and motor difficulties, and sensory deficits.
It is important to identify allergies to medication (including penicillin), foods, or other substances. The most common problem associated with medications is the development of a rash. Rashes, however, are common in children and may have occurred coincidentally at the time a medication was prescribed. Therefore try to determine whether the medication was the cause of the rash. Certain viral states “sensitize” a patient to a medication. The medication may be given at other times without any problems. Whenever a parent describes a “medication allergy,” ask the following questions:
“How do you know the child is allergic to …?”
“What was the rash like?” A hivelike or urticarial rash is likely to be a true allergy.
“Did the child have any problems other than the rash?”
“How long after the child started the medication11 did the rash appear?”
“After the medication was stopped, how long did the rash last?”
“Has the child ever taken the medication again with recurrence of the rash?”
Nutrition
Nutrition is central to the child’s well-being. Obesity in childhood is considered by some to be an epidemic in this country. In 2009–2010, 16.9% of U.S. children and adolescents or 12.5 million children and adolescents were obese.12
Parents need to be proactive in preventing their children from becoming obese by feeding them healthy foods and teaching them how to make healthy food choices for later on as older children and adults. Getting a complete nutritional history not only helps you monitor the child’s nutritional health, but may also help you make the diagnosis of an acute problem. Ask the following questions:
For infants:
“How many ounces of formula13 is the baby given a day? What kind of formula do you feed? How do you prepare it?”
“When did you introduce solid foods, such as cereals?”
“Has the child ever had a problem with vomiting? Diarrhea? Constipation? Colic?”
For infants, differentiate diarrhea from normal liquid stools. If the child is breast-fed, the stools are usually a yellow or mustard-colored liquid and may follow each feeding. If the child is formula-fed, the stools are more likely to be yellowish-tan and firmer. Infants frequently have green, brown, or grayish stools, and normal stools may be loose or liquid in consistency. With diarrhea, the stools are more frequent and all liquid, and watery rings stain the infant’s diaper. Minor changes in the stool are common. Normal infants may have several bowel movements a day but may go 1 or more days without a bowel movement. Small, hard, pebble-like stools indicate constipation.
Until an infant is 1 year of age, breast milk or infant formula should be his or her main food. Cow’s milk may be fine for older children, but it may irritate the infant’s digestive system, which is not fully developed. There are some major differences between cow’s milk and breast milk or formula: Cow’s milk has too much protein and sodium and too little iron, vitamin C, copper, and zinc for a developing infant. For a toddler or older child, determine how many ounces of milk and juice the child drinks. Inquire about the daily consumption of vegetables, fruit, protein, and especially “junk foods.” Does the child take a vitamin supplement? It is also valuable to ask about the meal pattern: Does he or she eat breakfast, lunch, dinner, and healthy snacks? Where does he or she eat? With whom? Do you eat any meals together as a family? Older children and adolescents eat many meals away from home; such patients are your best source of information about their eating patterns.
Growth and Development
Ask about the child’s pattern of growth. As is discussed later, the height, weight, and head circumference of children should be plotted on appropriate growth curves. Has the child’s growth been consistent, or has he or she crossed percentile lines on the growth chart? Is the mother concerned about her child’s growth?
Ask, “How has the child been growing? Are you concerned about his or her weight gain or about his or her linear growth?” Asking about how quickly the child outgrows shoes and clothes may give you an indication of his or her growth rate.
The child’s characteristics or temperament during infancy may be predictive of early developmental progress and of how he or she will respond to new experiences in years to come.
Ask, “Would you describe your child as active, average, or quiet?” If this is not the mother’s first child, it is appropriate to ask how this infant compares with the family’s other children: Is this child slower, faster, or about the same in development?
“When did the child first sleep through the night?”
“Do you have any concerns about the child’s development?” If yes, “What are they?”
“Has the child ever failed to make progress or ever lost any ability he or she once had?”
“Does the child have difficulty keeping up with other children?”
After asking general questions about the child’s development, you need to get information about specific developmental milestones that reflect the child’s ability in at least four areas: gross motor, language, fine motor, and personal and social development. The following questions should be asked:
The Denver Developmental Screening Test, shown in Figure 21-1, was developed to detect developmental delays in the first 6 years of a child’s life, with special emphasis on the first 2 years. It is standardized on the basis of findings from a large group of children in the Denver, Colorado, area and tests the four main areas of development indicated previously. A line is drawn from top to bottom of the sheet according to the age of the child. Each of the milestones crossed by this line is tested. Each milestone has a bar that indicates the percentage of the “standard” population that should be able to perform this task. Failure to perform an item passed by 90% of children is significant. Two failures in any of the four main areas indicate a developmental delay. This test is a screening device for developmental delays; it is not an intelligence test.
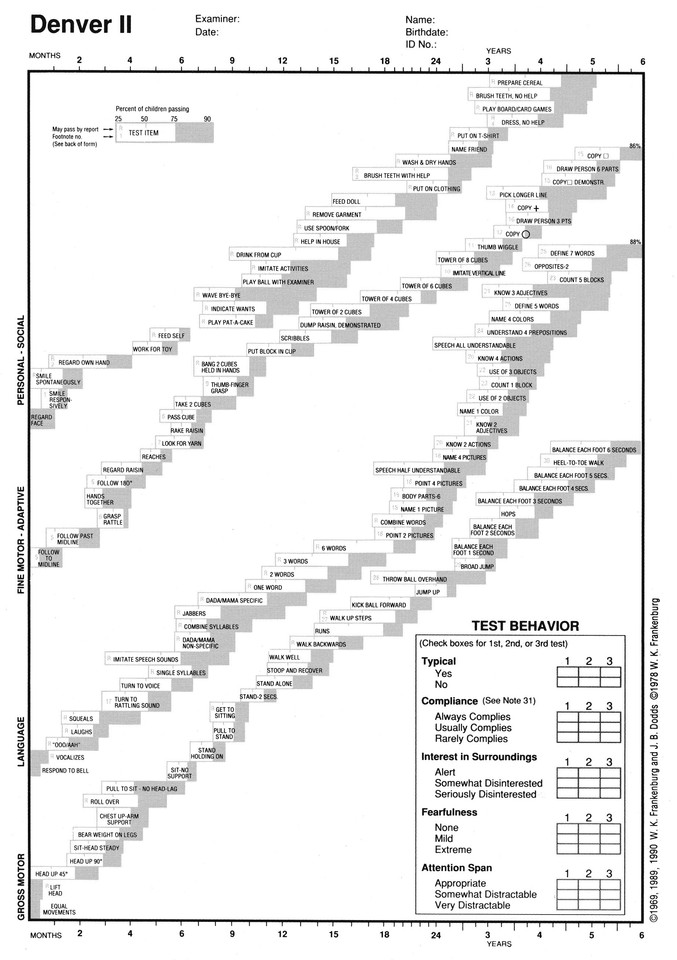
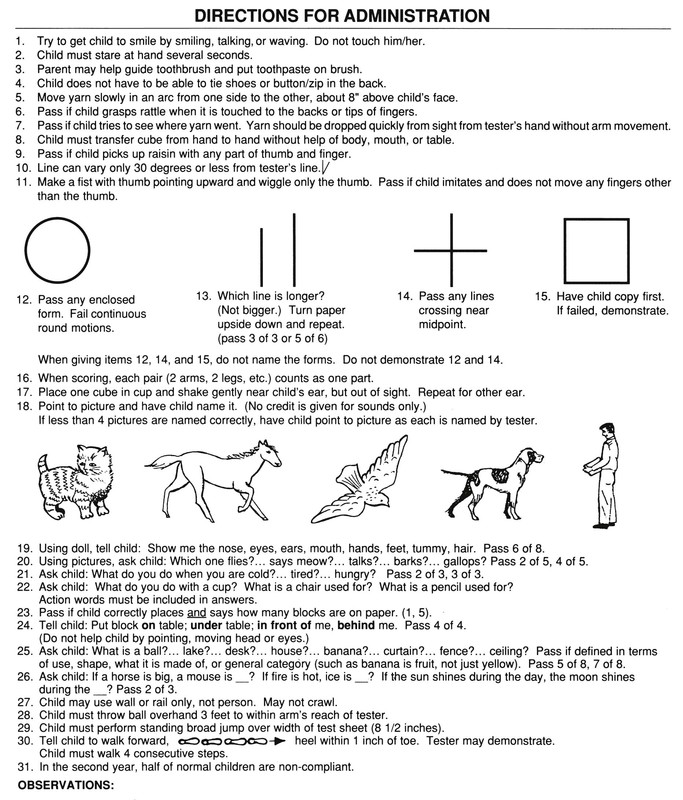
Figure 21–1 Denver Developmental Screening Test. (Reprinted with permission from William K. Frankenburg, MD, Denver Developmental Materials, Inc. Denver, Colo.)
Another screening test, the Ages and Stages Questionnaires,14 is a series of 19 age-specific questionnaires that use parents’ responses to specific questions to assess progress in communication, gross and fine motor, problem solving and personal adaptive skills. The questionnaires, which provide a pass/fail score, are useful in children from 4 to 60 months, takes 10 to 15 minutes to administer, and were normed on more than 12,000 children from diverse ethnic and socioeconomic backgrounds, including Spanish speakers.
For the school-aged child, the child’s social, motor, and language development, as well as emotional maturation, are reflected in current behavior. A nice way to broach this topic is to ask, “How would you describe your child as a person?” Follow up with some or all of these questions:
“What do you enjoy the most about your child? The least?”
“Does your child usually complete what he or she starts?”
“How does your child get along with other children his or her age?”
“How many hours of sleep does your child get each night?”
“Does the child have any recurrent nightmares?”
“What type of responsibility can he or she be given?”
“How old was your child when he or she started school?”
“In what grade is he or she now?”
“How is he or she doing in school?”
“Has he or she ever been left back?”
“What is your child’s grade level for reading? Math?”
“What does your child enjoy doing during his or her free time?”
“What kinds of things scare him or her?”
“How does the child get along with his or her brothers and sisters?”
“How much time does your child spend watching TV? Playing video games? On the computer?”
It is useful to ask whether the child has any disturbing habits. This question allows the parent or guardian to vent any previously unexpressed concerns. This may be asked as follows:
In 2007, because of a striking increase in the prevalence of autism and autistic spectrum disorders, the American Academy of Pediatrics recommended screening all children for the following behaviors:
Because it is clear that early intervention can significantly improve the outcome for children with autism and autistic spectrum disorders, the Academy recommends that this screening be performed at least twice during the first 2 years of life.
Immunization History
The pediatric history contains detailed information about immunizations. The current immunization schedule for persons aged 0 to 18 years of age in the United States,15 as of February 1, 2013, is shown in Appendix F.
Vaccines are one of the major successes of twentieth-century medicine; clinicians are unlikely to ever see many of the vaccine-preventable diseases such as polio, rubella, or diphtheria, and if an immunized child does have one of these diseases, that child may have an immune deficiency. However, if the child is missing one or more vaccines, you should consider the possibility the child is suffering from a vaccine-preventable illness. Note that the immunization schedule offers instructions for providing “catch-up” vaccinations for children who have fallen behind.
As the schedule of vaccines has become rather complex, many parents are unsure about the exact vaccines given to the child. Ask to see the immunization record, which many parents carry with them. Also, many localities have centralized vaccine registries where health care providers can access the record of a particular child.
You can partially reconstruct the child’s vaccine history, if necessary, with the following questions:
For the child 11 or older, ask, “Has she gotten any vaccines recently? How many?” Recent additions to the vaccine schedule provide adolescents with protection against pertussis; meningococcal disease; hepatitis A; and, for both boys and girls, human papillomavirus, the leading cause of cervical cancer. Also ask, “Did your child have a reaction to any of the shots?”
For an older child, ask “Has he or she ever had chickenpox?” See “Clinicopathologic Correlations” at the end of this chapter for a detailed description of this disease.
Social and Environmental History
The social and environmental history should include the parents’ ages and occupations, as well as the current living conditions. Ask these questions:
“How many rooms do you live in?”
“Is the child cared for in any other house?”
“Who supervises the child during the day?”
“How does the family have fun together?”
“Do both the child’s parents share in family life?”
“What is the condition of the paint and plaster in your home?”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



