Chapter 12
The Peripheral Vascular System
Veins which by the thickening of their tunicles in the old restrict the passage of blood, and by this lack of nourishment destroy their life without any fever, the old coming to fail little by little in slow death.
Leonardo da Vinci (1452–1519)
General Considerations
Diseases of the peripheral vascular system are common and may involve the arteries, veins, or lymphatic vessels. The arterial conditions include cerebrovascular, aortoiliac, femoropopliteal, renal, aortic occlusive, and aneurysmal diseases. The two most important diseases of the peripheral arteries are atherosclerosis of the larger arteries and microvascular disease. Peripheral vascular disease (PVD) is a nearly pandemic condition that has the potential to cause loss of limb or even loss of life.
The most common cause of peripheral arterial occlusive disease is atherosclerosis affecting the medium-sized and large vessels of the extremities. Narrowing of the vessel causes a decreased blood supply, resulting in ischemia. PVD is a common disorder that usually affects men older than age 50. People are at higher risk if they have a history of:
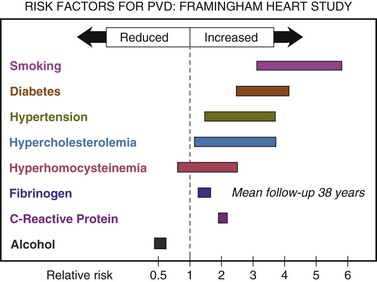
Figure 12-1 summarizes the risk factors for PVD according to the Framingham Heart Study.1
The classic symptoms of PVD are pain, heaviness, fatigue, burning, or discomfort in the muscles of your feet, calves, or thighs. These symptoms usually appear during walking or exercise and go away after several minutes of rest. At first, these symptoms may appear only when the patient walks uphill, walks faster, or walks for longer distances. Slowly, these symptoms come on more quickly and with less exercise. The legs or feet may feel numb while at rest. The legs also may feel cool to the touch, and the skin may look pale. When peripheral artery disease becomes severe, the patient may experience:
Atherosclerosis may become manifest by aneurysmal dilatation. The abdominal aorta is commonly affected. The aneurysm is commonly below the renal arteries and may extend as far as the external iliac arteries. Often, this aneurysm produces few, if any, symptoms. The examiner may discover a pulsatile mass as an incidental finding. Frequently, the first manifestation is the catastrophic rupture of the aneurysm. An abdominal aortic aneurysm (AAA) larger than 5 cm in diameter carries a 20% risk of rupturing within the first year of discovery and a 50% risk of rupturing within 5 years.
Vesalius described the first AAA in the sixteenth century. Before the development of a surgical intervention for the process, attempts at medical management failed. The initial surgical attempts at control entailed ligation of the aorta with poor results. In 1923, Rudolph Matas performed the first successful aortic ligation on a patient. Attempts were made to induce thrombosis by inserting intraluminal wires. In 1948, C. E. Rea wrapped reactive cellophane around the aneurysm to induce fibrosis and limit expansion. This technique was used on Albert Einstein in 1949, and he survived 6 years before dying of rupture. However, not until 1951 was an abdominal aneurysm surgically treated by resection and grafting. In that year, C. Dubost performed the first AAA repair with a homograft. Since then, great strides have been made in understanding the natural history of vascular disease, as well as in developing new technology to help diagnose and treat it.
In autopsy studies, the frequency rate of AAA ranges from 0.5% to 3.2%. In a large U.S. Veterans Administration screening study, the prevalence rate was 1.4%. The frequency of rupture is 4.4 cases per 100,000 persons. AAA is 5 times more common in men than in women and is 3.5 times more common in white men than in African-American men. The likelihood of development varies from 3 to 117 cases per 100,000 person-years.
Microvascular arterial disease occurs in patients with diabetes. Changes develop in the small arterioles that impair circulation to the skin or nerves, especially of the lower extremities, producing symptoms of ischemia. Peripheral neuropathy is a common sequela of microvascular disease. This neuropathy may be manifested as a defect in the sensory, motor, or autonomic system. Microvascular disease affects more than 15 million individuals in the United States. In diabetic patients, there is the tragic “Rule of 15,” which states that:
Also, in diabetic patients, the “Rule of 50” states that:
Peripheral venous disease often progresses to venous stasis and thrombotic disorders. One of the dreaded complications of thrombotic disease is pulmonary embolism. In the United States, more than 175,000 deaths per year are attributed to acute pulmonary embolism.
Structure and Physiology
Diseases of the peripheral arterial system cause ischemia of the extremities. When the body is at rest, collateral blood vessels may be able to provide adequate circulation. During exercise, when oxygen demand increases, this circulation may not be sufficient for the actively contracting muscles, and ischemia may result.
The venous system consists of a series of low-pressure capacitance vessels. Nearly 70% of the blood volume is contained in this system. Although offering little resistance, the veins are controlled by a variety of neural and humoral stimuli that enhance venous return to the right side of the heart. In addition, valves aid in the return of blood.
When an individual is in the upright posture, the venous pressure in the lower extremity is the highest. Over many years, the veins dilate as a result of weakening of their walls. As the walls dilate, the veins are unable to close adequately, and reflux of blood occurs. In addition, the venous pump becomes less efficient in returning blood to the heart. Both of these factors are responsible for the venous stasis seen in patients with chronic venous insufficiency. Complications from venous stasis include pigmentation, dermatitis, cellulitis, ulceration, and thrombus formation.
The lymphatic system is an extensive vascular network and is responsible for returning tissue fluid (lymph) back to the venous system. The extremities are richly supplied with lymphatic tissue. Lymph nodes, many of which are located between major proximal joints, aid in filtering the lymphatic fluid before it enters the blood. The most important clinical symptoms of lymphatic obstruction are lymphedema and lymphangitis.
Review of Specific Symptoms
Many patients with PVD are asymptomatic. When patients are symptomatic, vascular disease causes the following:
Pain
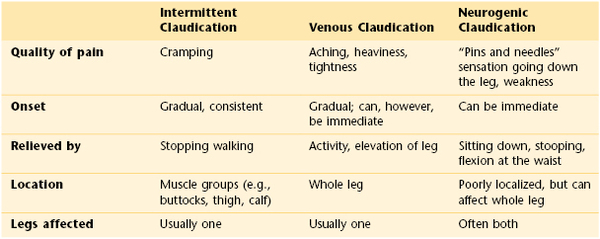
Pain is the principal symptom of atherosclerosis. Whenever a patient complains of pain in the calf, arch of the foot, thighs, hips, or buttocks while walking, PVD of the arteries must be considered. The symptom of pain in the lower extremity during exercise and relieved by rest is called intermittent claudication. The site of the pain is always distal to the occlusive disease. Supply does not equal demand. As the disease progresses, pain at rest occurs. This is often severe and is aggravated by cool temperatures and elevation, especially during sleep in bed. Pain may also occur with deep vein thrombosis, a condition known as venous claudication. It is the combination of venous valvular incompetence, outflow obstruction, and calf muscle pump function derangement that generates the hemodynamic setting most often associated with the development of venous claudication. A unique feature of venous claudication is that motionless standing is often more difficult than walking. This is because contraction of the muscles in our legs while walking pumps the blood through the veins and back to the heart. Neurogenic claudication is a common symptom of lumbar spinal stenosis, or inflammation of the nerves emanating from the spinal cord. The pain is often related to posture. The combination of the stenosis with certain back postures such as arching puts pressure on lumbosacral nerve roots and the cauda equina. Table 12-1 describes the differences between intermittent claudication, venous claudication, and neurogenic claudication.
If a male patient complains of pain in the buttocks, hips, or thighs while walking, the examiner should inquire about erectile dysfunction. The patient may also experience leg numbness or weakness. Leriche’s syndrome is chronic aortoiliac obstruction; the patient presents with intermittent claudication and erectile dysfunction. In this condition, the terminal aorta and iliac arteries are involved by severe atherosclerosis at the aortic bifurcation.
Patients occasionally complain of bilateral leg pain or numbness that occurs while walking, as well as while resting. This is called pseudoclaudication and is a symptom of musculoskeletal disease in the lumbar area.
Skin Changes
Skin color changes are common with vascular disease. In chronic arterial insufficiency, the affected extremity is cool and pale. In chronic venous insufficiency, the extremity is warmer than normal. The leg becomes erythematous, and erosions produced by excoriation result. With chronic insufficiency, stasis changes produce increased pigmentation, swelling, and an “aching” or “heaviness” in the legs. These changes characteristically occur in the lower third of the extremity and are more prominent medially. When venous insufficiency occurs, edema of dependent areas results.
Patients with acute deep vein thrombosis have secondary inflammation of the tissue surrounding the vein. This produces signs of inflammation: warmth, redness, and fever. Swelling is the most reliable symptom and sign associated with venous obstruction. This finding is indicative of severe deep vein obstruction because the superficial veins of the lower extremity carry only 20% of the total drainage and are not associated with swelling. The extremities should be compared, and a difference in circumference of 2 cm at the ankle or midcalf should be considered significant.
Edema
Lymphedema results from either a primary abnormality in the development of the lymphatic system or an acquired obstruction to flow. Whether the congenital or the acquired form is involved, the net result is stasis of lymph fluid in the tissues, producing a firm, nonpitting edema. Over several years, the skin takes on a rough consistency similar to that of pigskin. Because lymphedema is usually painless, the only symptom is “heaviness” of the extremity.
Ulceration
Persistent ischemia of a limb is associated with ischemic ulceration and gangrene. Ulceration is almost inevitable once skin has thickened and the circulation is compromised. Ulceration related to arterial insufficiency occurs as a result of trauma to the toes and heel. These ulcers are painful, have discrete edges that produce a “punched-out” appearance, and are often covered with crust. When infected, the tissue is erythematous.
In contrast to arterial insufficiency ulceration, venous insufficiency leads to stasis ulceration, which is painless and occurs in the ankle area or lower leg just above the medial malleolus. The classic manifestation is a diffusely reddened, thickened area over the medial malleolus. The skin has a cobblestone appearance resulting from fibrosis and venous stasis. Ulceration occurs with the slightest trauma. Rapidly developing ulcers are commonly caused by arterial insufficiency, whereas slowly developing ulceration is usually the result of venous insufficiency. Figures 12-2 and 12-3 show stasis dermatitis and ulcerations over the medial malleoli. Patients with leg ulcers should be asked the following:
“What did the ulcer look like when it first appeared?”
“What do you think started the ulcer?”
“What kind of medications have you been taking?”
“Is there a history of any generalized diseases, such as anemia? Rheumatoid arthritis?”
Emboli
A history of emboli is important. Thrombus formation results from stasis and hypercoagulability. It appears, however, that venous stasis is the most important cause of thrombus formation. Bed rest, congestive heart failure, obesity, pregnancy, recent extended travel on airplanes, and oral contraceptives have been linked to thrombus formation and emboli.
Symptoms secondary to emboli can include shortness of breath from pulmonary emboli; abdominal pain from splenic, intestinal, or renal artery emboli; neurologic symptoms from carotid or vertebrobasilar artery emboli; and pain and paresthesias from peripheral artery emboli.
Neurologic Symptoms
Cerebrovascular occlusive disease causes many neurologic symptoms, including strokes,2 dizziness, and changes in consciousness. Occlusion of the internal carotid artery produces a syndrome of contralateral hemiplegia, contralateral sensory deficits, and dysphasia. Vertebrobasilar disease is associated with diplopia, cerebellar dysfunction, changes in consciousness, and facial paresis.
Effect of Vascular Disease on the Patient
A patient with chronic arterial insufficiency has worsening pain while walking. As the condition progresses, ulceration of the toes, feet, and areas susceptible to trauma, such as the shins, develops. Pain may become excruciating. Gangrene of a toe may develop, and amputation of the toe is frequently followed by amputation of the foot and leg. In addition, the patient becomes increasingly depressed as a result of ongoing mutilation of the body.
Physical Examination
The equipment necessary for the examination of the peripheral vascular system consists of a stethoscope, a tourniquet, and a tape measure.
The physical examination of the peripheral vascular system consists of inspection, palpation of the arterial pulses, and some additional tests if disease is thought to be present. All these techniques are usually integrated with the rest of the physical examination.
The patient lies supine, with the examiner standing to the right of the bed. The evaluation of the peripheral vascular system includes the following:
Inspection
Inspect for Symmetry of the Extremities
The extremities should be compared for asymmetries in size, color, temperature, and venous patterns. Figure 12-4 depicts massive lymphedema of the right upper extremity secondary to a right total mastectomy 18 years earlier.
Inspect the Lower Extremities
The lower extremities should be inspected for pigmentary abnormalities, ulcers, edema, and venous patterns. Is cyanosis present? Is edema present? If edema is present, does it pit? Bilateral color changes and swelling of the legs of the patient are pictured in Figure 12-5. The patient had chronic venous insufficiency. She died of a massive pulmonary embolus 1 day after this photograph was taken.
Assess the Skin Temperature
Evaluate the temperature by using the back of your hand. Compare similar areas of each extremity. Coolness of an extremity is common with arterial insufficiency.
Inspect for Varicosities
Ask the patient to stand, and inspect the lower extremities for varicosities. Look at the area of the proximal femoral ring, as well as in the distal portion of the legs. Varicose veins in these locations may not have been visible when the patient was lying down.
The patient in Figure 12-6 was a 37-year-old woman with severe right-sided heart failure. Notice the marked dilated and tortuous veins in the popliteal fossa. Also notice the increased pigmentation of the skin over the lower legs. Figure 12-7 shows another patient, 65 years of age, with marked bilateral lower extremity varicosities extending from the groin down the entire legs. Despite their appearance, she suffered no other symptoms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree