Reader activities
Having read this scenario, consider the following:
- For what reasons might the consultant have requested IAP measurements? Consider how a valid measurement might be obtained.
- Consider the rationale for an emergency laparotomy in this scenario.
- Why was it necessary to intubate and ventilate Mr Borkowski?
- What concerns might you have regarding the renal function of Mr Borkowski?
Pathophysiology related to increased intra-abdominal pressure
Normal IAP is 05 mmHg (Brush 2007b). Abdominal compartment syndrome (ACS) is a condition caused by an increase in abdominal pressure, referred to as intra-abdominal hypertension (IAH) (Walker and Criddle 2003). Physiological compromise starts when the pressure rises above 12 mmHg (Brush 2007b). Once pressures reach 20 mmHg, irreversible tissue ischemia occurs and organ function is compromised (World Society of Abdominal Compartment Syndrome (WSACS) 2009). As Mr Borkowski’s IAP is already 18 mmHg, he is at significant risk. At this point the abdomen often looks distended, and can feel rigid and tense on palpation (see Figure 8.1).
Figure 8.1 Rigid abdomen. (Photo courtesy of Dr Manu Malbrain, adapted from Deeren DH, Zachée P, Malbrain MLNG (2005) Granulocyte colony-stimulating factor-induced capillary leak syndrome confirmed by extravascular lung water measurements. Annals of Hematology 84(2), 89–94.)

The main cause of IAH is reduced gut perfusion, causing capillary endothelial damage and cellular ischemia, leading to further secondary damage (Walker and Criddle 2003). Large amounts of interstitial fluid can accumulate, due to loss of integrity of the capillary membrane causing the abdominal wall to expand. As compliance reduces, the pressure within the abdominal cavity rises, causing occlusion of capillary blood flow and compromise of venous return and arterial flow (Wolfe 2009). This worsens the ischemia, triggering a vicious cycle leading to further increases in IAH.
Any patient with a severe inflammatory response can develop IAH. Patients who have suffered direct peritoneal or retroperitoneal injury from trauma, surgery or inflammation are also at risk (Wolfe 2009). Pancreatitis, the diagnosis for Mr Borkowski, is a recognised cause, as is bowel obstruction (Tiwari et al. 2006). Sepsis is also often associated with IAH due to uncontrolled inflammation. Obese patients with a body mass index >45 kg/m2 are also at high risk, particularly when placed in the supine position (Brush 2007a).
A high IAP compromises the function of a number of other organs. The kidneys are affected by direct renal artery compression, and because of central venous compression. Once the IAP exceeds central venous pressure (CVP), preload is reduced, lowering cardiac output and arterial blood pressure, thus reducing perfusion to the kidneys (Wolfe 2009). The effects of this can be seen in Mr Borkowski’s haemodynamic and renal data. This would also partly explain the metabolic acidaemia as being related to the development of acute tubular necrosis (Brush 2007a). The production of lactic acid related to cellular hypoxia would be another contributing factor explaining this metabolic picture.
The pulmonary effects of IAH are largely mechanical. As the pressure under the diaphragm increases, there is an increased work of breathing resulting in rapid shallow breathing, as seen in the data presented for Mr Borkowski. This reduction in alveolar ventilation causes atelectasis and a resultant V/Q mismatch, and this has demonstrated itself in the blood gas analysis results revealing hypoxaemia, hypercarbia and a respiratory acidaemia (Brush 2007a). This might necessitate the use of ventilatory support for Mr Borkowski. The high peak inspiratory pressures required to maintain adequate tidal volumes, however, increases the risk of barotrauma, volutrauma, biotrauma and acute lung injury (Wolfe 2009). IAH can also contribute to a rise in the intracranial pressure of susceptible patients as cerebral venous return becomes obstructed (Walker and Criddle 2003; Brush 2007a; Wolfe 2009).
Tests and investigations
Intra-abdominal pressure monitoring
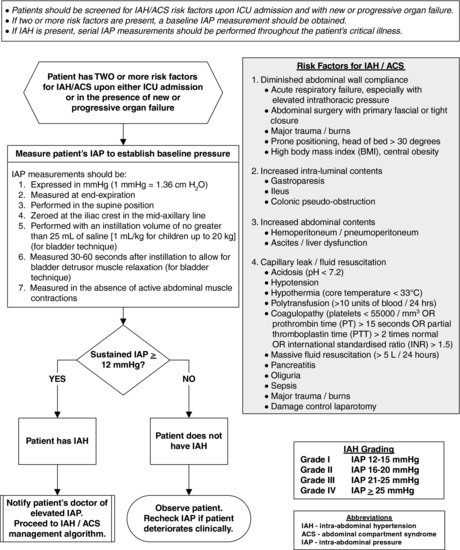
Normal IAP is 0–5 mmHg, although in critically ill patients a value of up to 7 mmHg is acceptable (WSACS 2009). Mr Borkowski should be assessed for signs of IAH. The WSACS (2009) recommends that all critically ill patients should be screened for signs of IAH, and that a baseline IAP recorded when two or more of the risk factors for ACS are present. In the presence of IAH, the WSACS (2009) recommend that serial measurements should be taken throughout the period of critical illness (see Figure 8.2).
Figure 8.2 Intra-abdominal hypertension (IAH) assessment algorithm. (Algorithm courtesy of the World Society of the Abdominal Compartment Syndrome (WSACS).)
Recognising higher levels of IAP is vital to prevent the above sequelae from developing. Traditionally, this was done by clinical observation of the abdomen, monitoring for signs of tautness, often combined with girth measurements if concern was apparent. These subjective assessments have, however, more recently been shown to be unreliable determinants of IAP (Kirkpatrick et al. 2000; Sugrue et al. 2002), and more direct measurements of IAP are now available.
There are a number of different methods that can be utilised to measure IAP, but the most common approach currently in use is via an indwelling urinary catheter. This can be done using either a fluid manometer set (see Figures 8.3 and 8.4) or a transducer system (Harrahill 1998; Brush 2007b). A good overview of the range of methods and their potential advantages and limitations can be found in Malbrain (2004).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



