Definitions of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS)
Adult respiratory distress syndrome was first described by Ashbaugh et al. in 1967 as a clinical syndrome different from other types of acute respiratory failure, with clinical characteristics of tachypnoea, hypoxaemia resistant to supplemental oxygen, diffuse alveolar infiltrates and decreased pulmonary compliance (Ashbaugh et al. 1967).
Since its initial description in 1967, the criteria for defining ALI/ARDS have changed several times. In 1988 Murray and colleagues proposed a definition which described whether the syndrome was in an acute or chronic phase, the physiological severity of pulmonary injury and the disorder associated with the development of the lung injury (Murray et al. 1988). In 1994, recognising that the study of ALI and ARDS was still hindered by the lack of a simple, uniform definition, the North American–European Consensus Conference (NAECC) published further revised definitions (Bernard et al. 1994) (see Table 1.2).
Table 1.2 American–European Consensus Conference Definitions of ALI/ARDS.
Source: From Bernard et al. (1994).
From the NAECC definition it can be deduced that Mr Kuan Yew has ARDS. He has developed acute respiratory failure requiring ventilation; he is hypoxaemic with a PaO2/FiO2 ratio of 21.6 kPa and has bilateral infiltrates on chest x-ray (see Figure 1.1).
Figure 1.1 Chest X-ray. (X-ray courtesy of Dr Duncan Wyncoll, Consultant Intensivist, Guy’s and St Thomas’ NHS Foundation Trust, London.)
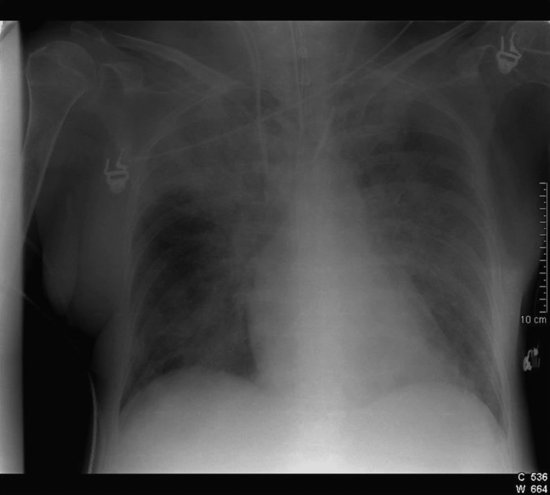
Mr Kuan Yew does not have a pulmonary artery catheter in situ to enable determination of the pulmonary artery occlusion pressure (PAOP); however, he has no history of cardiac disease and clinically shows no signs of left-atrial hypertension such as a raised central venous pressure (CVP), although the latter can be normal in left-atrial hypertension. Mr Kuan Yew is also demonstrating symptoms of severe sepsis (see Chapter 4 for further information on sepsis), a common co-existing condition.
Pathophysiology of ALI/ARDS
Pathology
In 1972 the National Institute of Health estimated the incidence of ARDS at 60 cases per 100 000 population per year (National Heart and Lung Institute, National Institute of Health (NHL, NIH) 1972). Several robust studies since then have demonstrated a wide range of incidence rates of ARDS from 1.5 to 8.3 cases per 100 000 per year (Villar and Slutsky 1989; Garber et al. 1996). Although it could therefore be considered a rare disease, the mortality of ARDS is high, estimated to be between 34% and 65% (Estenssoro et al. 2002; Herridge et al. 2003). The incidence of ALI, however, appears more common with many patients within high dependency settings having a PaO2/FiO2 of <40 kPa. It is therefore essential that critical care nurses have an understanding of the pathophysiology and management of ALI and ARDS. The major cause of death in patients with ALI/ARDS is multiple organ failure and irreversible respiratory failure, with 84% of deaths occurring more than three days after the onset of ALI/ARDS caused by multi-system organ failure (Ware and Matthay 2000).
Acute lung injury is a term used to describe the response of the lungs to a broad range of insults with ARDS representing the most severe end of the spectrum. Its pathophysiology is driven by an aggressive inflammatory reaction which results in widespread changes throughout the lung. A broad variety of precipitating causes are recognised and these can be differentiated into those which cause injury to the lung directly and those which cause injury indirectly (see Table 1.3). A number of endogenous anti-inflammatory mechanisms are also initiated to counteract the effects of the aggressive pro-inflammatory response; however, these responses may be excessive and contribute to a state of immunoparesis (Doyle et al. 1995).
Table 1.3 Risk factors for ARDS.
| Direct causes | Indirect causes |
|
|
Epidemiological literature indicates that the major risk factor for the development of ALI and ARDS is severe sepsis; 18–40% of patients with sepsis will develop ALI/ARDS, followed by pneumonia, aspiration of gastric contents, multiple blood transfusions, multiple trauma and pregnancy-related ALI/ARDS (Villar and Slutsky 1989; Ware and Matthay 2000).
From Mr Kuan Yew’s clinical history and initial presentation it appears that he may have developed an acute lung injury and subsequent ARDS from a direct cause such as lobar pneumonia. It is also important, however, to note that as Mr Kuan Yew is mechanically ventilated and is critically ill, he is at a significant risk of developing a nosocomial infection and secondary sepsis (Vincent et al. 1995), a major risk factor for the development of ARDS, and at present he is indeed demonstrating signs of severe sepsis.
ALI and ARDS cause diffuse alveolar damage affecting all parts of the alveolus, including the epithelium, the endothelium and the interstitial space. It is a progressive condition with the pathological changes typically described as passing through three overlapping phases – an inflammatory or exudative phase, a proliferative phase and a fibrotic phase (Ware and Matthay 2000).
Exudative phase
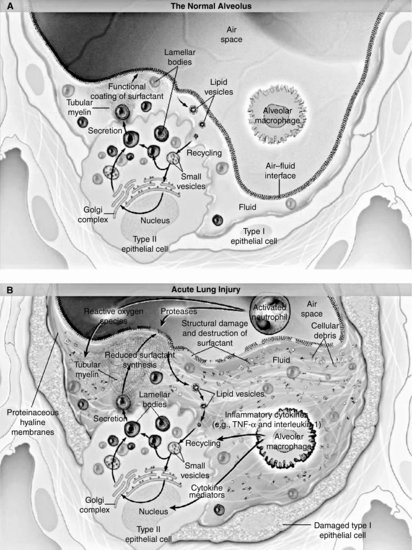
Lasting for up to seven days following the onset of symptoms, the exudative or acute phase of ALI/ARDS is characterised by the influx of protein-rich oedema fluid into the alveolar air spaces, as a result of increased permeability of the alveolar–capillary membrane and the formation of hyaline membranes. The hyaline membranes contain necrotic epithelial cells, plasma proteins which have been deposited in the alveolar space as part of the inflammatory exudate that leaks across the alveolar–capillary membrane, immunoglobulin and complement. The alveolar–capillary barrier has focal areas of damage and the alveolar wall is oedematous. Neutrophils are increasingly found within the capillaries, interstitium and eventually airspaces. As the process of damage progresses, there is extensive necrosis of type 1 alveolar epithelial cells and further hyaline membrane formation (Figures 1.2a and 1.2b).
Figure 1.2 (a) Histopathology slide of lung tissue. (b) Diagrammatic illustration of cellular changes in ARDS. (Baudouin 2004). Used with permission of Massachusetts Medical Society.
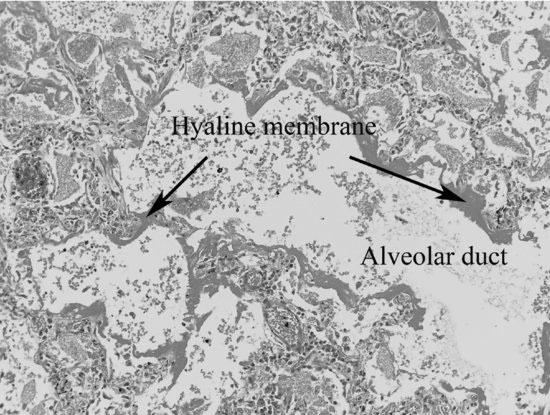
These pathological changes can be seen in Mr Kuan Yew’s clinical picture by the presence of pulmonary oedema and his deterioration in lung function. Flooding of the alveoli with protein-rich fluid and debris has caused a decrease in lung compliance, reflected in the high airway pressures. It has also caused a significant reduction in the diffusion of oxygen, leading to a reduced arterial oxygen saturation and PaO2. Fluid-filled and collapsed alveoli result in the development of a right to left intra-pulmonary shunt. The negative effects of this on Mr Kuan Yew’s gas exchange are further compounded by loss of the normal compensatory hypoxic pulmonary constriction.
Proliferative phase
The proliferative phase is characterised by organisation of the hyaline membranes by proliferating fibroblasts, cell debris and inflammatory cells (Ware and Matthay 2000). Necrosis of type 1 alveolar cells exposes areas of the epithelial basement membrane and the lumens of the alveoli fill with leucocytes, red blood cells and fibrin. Type 2 alveolar cells, which are responsible for the production of surfactant, are also damaged but some proliferate along the alveolar wall in an attempt to cover damaged areas of the epithelium and differentiate into type 1 cells. Pulmonary oedema is less prominent at this stage; however, alveolar collapse becomes more marked and the alveolar ducts become narrowed and distorted. This then leads to a further increase in the degree of intrapulmonary shunt, leading to a further deterioration in gas exchange, and hypoxaemia resistant to oxygen therapy.
At this stage the process can be reversed and the lung parenchyma may return to normal. However, in some cases the damage is severe and the hyaline membranes become incorporated into the walls of the revised alveoli (Ware and Matthay 2000).
Fibrotic phase
The fibrotic phase can begin as early as ten days following the insult and is characterised by progressive thickening of the vasculature walls and an increase in the amount of lung collagen (Ware and Matthay 2000). Fibrosis results in a further reduction in lung compliance, increasing the work of breathing, decreasing the tidal volume and resulting in the retention of CO2. As a result of the destruction of some alveoli and interstitial thickening, gas exchange is reduced and this contributes to further hypoxaemia and ventilator dependence.
Pathogenesis of ALI/ARDS
Inflammation
As a result of the initiation of an inflammatory response, there is increased leucocyte production and mobilisation to the inflamed site. Mediator cascades including the production of cytokines, chemokines, free radicals and complement and coagulation pathway components are also activated. There is also an anti-inflammatory response.
The neutrophil is the dominant leucocyte involved in the pro-inflammatory response. Neutrophils cause cell damage by the production of free radicals, pro-inflammatory mediators and proteases, and excessive quantities of these products, including cytokines, have been found in patients with ARDS (Chollet et al. 1996). The inflammatory response is in part driven by cytokines. Two of the major pro-inflammatory cytokines are tumour necrosis factor-α (TNF-α) and interleukin-1 (IL-1). The actions of these include (1) recruitment and localisation of macrophages to the lung parenchyma, (2) stimulation of other inflammatory cytokines such as IL-6 and IL-8 and (3) adherence of neutrophils to endothelium. Cytokines and other pro-inflammatory mediators such as endotoxin and thrombin have also been implicated in the increased vascular permeability that contributes to pulmonary oedema in ALI/ARDS (Ware and Matthay 2000).
This inflammatory response leads to surfactant dysfunction in ALI/ARDS (Baudouin 1997), with destruction and loss of type 2 cells resulting in decreased synthesis and recirculation of surfactants. Additionally, leakage of protein-rich fluid into the alveoli during the development of ALI/ARDS, as seen in Mr Kuan Yew’s clinical picture, contaminates the surfactant, resulting in a further reduction in its ability to function. The degree to which lack of surfactant contributes to the pathogenesis of ALI/ARDS, however, remains unclear.
Fibroproliferative response and resolution of ARDS
The fibroproliferative response is part of a normal repair process; however, if not closely regulated, it can have serious consequences such as lung fibrosis. Mediators such as TNF-α and products of the coagulation cascade such as thrombin, fibrin and factor Xa fuel the fibrotic response and stimulate local fibroblasts to migrate, replicate and produce excessive amounts of connective tissue.
In some patients pulmonary fibrosis does not completely resolve and can lead to problems with weaning from mechanical ventilation. There does not appear to be a uniform response to injury in that some patients develop ALI, some develop ARDS and some do not develop pulmonary symptoms at all. The reason for this may lie in genetics and recent evidence suggests that there is a genetic susceptibility both to sepsis and ARDS (Wax and Angus 2000).
Holistic assessment and detailed management of all issues related to total patient care are fundamental in caring for patients such as Mr Kuan Yew who have ARDS. In early ARDS, however, difficulties with oxygenation can be the major physiological challenge requiring careful assessment, titration of therapy and meticulous monitoring.
Tests and investigations
Continuous pulse oximetry
Continuous pulse oximetry has become a vital part of monitoring the critically ill patient as it is readily available, is non-invasive and can be used in many different settings. Pulse oximeters shine red and infrared light through a finger or ear lobe using a probe. The proportion of light absorbed allows the amount of oxygenated and deoxygenated haemoglobin to be estimated. The pulsatile component of absorption corresponds to arterial blood, and therefore, arterial oxygen saturation can be deduced. When arterial oxygen saturations are greater than 80%, current pulse oximeters can detect arterial oxygen saturations to within a few percentage points and their use would, therefore, be beneficial in the assessment of Mr Kuan Yew’s oxygenation. However, they are less accurate when arterial oxygen saturations are lower. It is also important to be aware that inaccurate values may be obtained in patients with shock, due to poor peripheral perfusion, by carboxyhaemoglobin, by low levels of haemoglobin and by the use of some dyes such as methylene blue which absorb wavelengths of light used by some pulse oximeters. After ruling out the possibility of any of these contraindications in Mr Kuan Yew’s case, pulse oximetry will be a useful tool to rapidly detect periods of arterial hypoxaemia.
Arterial blood gas analysis
Arterial blood gas analysis is considered the gold standard in the assessment and management of ARDS patients such as Mr Kuan Yew. To ensure accuracy, however, it is important that the health professional obtaining the sample is aware of several key points. The sample must be taken and processed as quickly as possible to eliminate aerobic contamination; the current FiO2 and temperature of the patient should be recorded at the time of sampling, the latter to allow temperature correction, and the sample rapidly analysed in a calibrated blood gas machine. If the arterial blood gas results are to reflect current ventilatory support, the sample should not be obtained until 15–20 minutes following any manipulation of ventilator settings. PaO2, PaCO2 and pH are measured during arterial blood gas analysis. Oxygen saturation may be measured by a co-oximeter built into a blood gas machine or estimated from the PaO2 based on the oxygen-dissociation curve corrected for temperature, PaCO2 and pH. This estimate is considered reasonably accurate for oxygen saturations greater than 80% but is significantly erroneous at lower saturations.
PaO2/FiO2 measurement
The sole use of PaO2 in assessing Mr Kuan Yew has limitations. As a result calculation of the ratio of PaO2 to FiO2 is now commonly used as an additional measurement (see Chapter 2 on weaning for how to calculate the PaO2/FiO2 ratio). The usefulness of the PaO2/FiO2 ratio is clearly demonstrated in Mr Kuan Yew’s arterial blood gas results. At first glance a PaO2 of 10.8 kPa could appear to be an acceptable level; however, when the FiO2 is taken into consideration, it is clear from the NAECC definition that he has ARDS as his PaO2/FiO2 ratio is 21.6 kPa.
Evidence-based management of a patient with ALI/ARDS
Airway and breathing
In patients like Mr Kuan Yew who have severe ARDS, the hallmark respiratory abnormality is hypoxaemia which gradually becomes more resistant to supplemental oxygen therapy as the condition progresses. Maintaining adequate arterial oxygenation is therefore a goal given a high priority and usually requires assisted/mechanical ventilation.
Assisted ventilation is generally carried out invasively via an endotracheal tube. However, a small subset of patients may be candidates for non-invasive ventilation (Hilbert et al. 2001). Non-invasive positive pressure ventilation (NIPPV) is finding increasing application in the management of acute respiratory failure in the high-dependency setting and it may be postulated that it would be successful in carefully chosen patients with ALI. It may aid in the recruitment of collapsed and fluid-filled alveoli, thereby reducing intrapulmonary shunt, and could also facilitate unloading of the respiratory muscles, reducing the work of breathing. It is important to highlight, however, that patients with ALI and ARDS are also frequently haemodynamically unstable, have severe hypoxaemia or have a rapidly progressive course of disease. Therefore, although NIPPV has been shown to be beneficial in some patients, there is little published experience or evidence of its benefits in patients with ARDS. It may therefore not be a good first choice for Mr Kuan Yew.
Approaches to mechanical ventilation
The pathophysiology of ARDS has been presented earlier in this chapter; however, it is important to highlight some important features which are relevant when discussing Mr Kuan Yew’s ventilatory management. Computerised tomographic scanning (CT) has demonstrated that consolidation of lung tissue in ARDS is not uniform but rather is concentrated in dependent lung regions, leaving non-dependent areas relatively aerated. This distribution of aerated lung, described as ‘baby lung’ (Gattinoni et al. 1987), has important implications for mechanical ventilation strategies.
Traditional methods of mechanically ventilating patients with ALI and ARDS gave priority to the maintenance of oxygenation, while minimising the use of high concentrations of oxygen, and providing sufficient ventilation to maintain arterial pH and PaCO2 within normal limits. These goals were achieved by the administration of increased levels of positive end expiratory pressure (PEEP) to enable a decrease in the FiO2, and the use of relatively large tidal volumes of 10–15 mL/kg. This approach, however, results in high inspiratory pressures in patients who already have decreased lung compliance. The application of tidal volumes of 10–15 mL/kg can also lead to over-inflation of the normal ‘baby lung’ which has been shown to cause local damage and further inflammation (Dreyfuss and Sauman 1998). Present understanding of ventilator-induced lung injury suggests that a traditional mechanical ventilation strategy such as this, using high tidal volumes and is likely to enhance Mr Kuan Yew’s lung injury. Lung injury is caused by excessive volumes rather than high airway pressure (Dreyfuss et al. 1988) and even healthy animals ventilated with high tidal volumes for several hours develop pulmonary oedema that is histologically identical to that seen in ARDS. Furthermore, in animal models with ALI, large lung volumes have been shown to cause increased oedema accumulation and cytokine production (Tremblay et al. 1997). Although evidence in humans is lacking, it is likely that ventilating with high tidal volumes results in similar effects.
Four randomised controlled trials of ‘lung-protective’ ventilation, directed at preventing over-distension of the lung in ARDS, have been published over the past ten years (Brochard et al. 1998; Stewart et al. 1998; Brower et al. 1999; Acute Respiratory Distress Syndrome Network (ARDSNet) 2000). Of these the ARDSNet (2000) study is the largest and the only one to date to demonstrate a mortality benefit of a lung-protective strategy in ARDS patients. Eight hundred and sixty one patients were randomised into two groups. One group received a tidal volume of 6 mL/kg if the plateau pressure (Pplat) did not exceed 30 cmH2O and 4–5 mL/kg if the Pplat exceeded 30 cmH2O and the other group received tidal volumes of 10–12 mL/kg if the Pplat did not exceed 50 cmH2O and tidal volumes as low as 4 mL/kg if the Pplat exceeded 50 cmH2O. A 9% mortality difference was observed in those patients who received the lower tidal volume ventilation strategy. Although the design of the ARDSNet trial has been heavily criticised, the ARDSNet lower tidal volume strategy has become accepted as the standard on which to base the ventilatory management of patients with acute lung injury (see Table 1.4 for protective lung ventilation protocol from the ARDSNet study) and this is how Mr Kuan Yew’s ventilation should be managed.
Table 1.4 Summary of ARDSNet (2000) low tidal volume strategy.
Source: Adapted from the NIH NHLBI ARDSNet low tidal volume ventilation strategy (ARDSNet 2000).
| Variable | Settings |
| Ventilator mode | Volume assist control |
| Set tidal volume (mL/kg) | Aim for 6 mL/kg (if baseline tidal volume >8 mL/kg, then set initial tidal volume at 8 mL/kg and reduce by 1 mL/kg every 2 h until 6 mL/kg) |
| Rate (breaths/min) | Set to approximate baseline rate of 6–35 breaths/min but not >35 breaths/min |
| Pressure (cmH2O) | Aim for Pplat <30 cmH2O or peak pressure <35 cmH2O |
| Inspiratory flow rate (L/min) | Above patient demand (>80 L/min) |
| Inspiratory:expiratory ratio | 1:1–1.3 |
| PaO2 (kPa) | 7.3–10.7 |
| SpO2 (%) | 88–95 |
| PEEP and FiO2 | Incremental FiO2/PEEP combinations have been suggested with PEEP range from 5 to 24 cmH2O (see Table 1.3) |
| pH | 7.30–7.45 |
Volume control versus pressure controlled ventilation
Traditionally, invasive mechanical ventilation has been provided by volume controlled modes, as in the case of Mr Kuan Yew, whereby a preset tidal volume is delivered at a preset rate and inspiratory flow. Volume control, has the benefit of maintaining a constant tidal volume and hence minute ventilation and PaCO2 under changing respiratory system conditions and easy detection of changes in lung mechanics. Over the past decade, however, in light of research demonstrating the non-homogenous distribution of consolidation in ARDS and the focus on limiting alveolar distension, there has been a trend towards the use of pressure controlled modes of ventilation.
With pressure control, a decelerating inspiratory flow is applied to a preset pressure limit, allowing the critical care team to select both inspiratory and expiratory pressures with the advantage of limiting pressure to a set level. The critical care nurse has to be particularly vigilant when caring for a patient on pressure control ventilation as changes in lung compliance are not as easily detected. Close observation of the tidal volume and PaCO2 is essential to detect changes in lung mechanics.
As a result of technological advances in mechanical ventilators, the distinction between volume- and pressure-controlled modes of ventilation has become slightly blurred. Parameters can now be adjusted within each of the different modes, such as pressure limitation within a volume-controlled mode of ventilation. The critical care teams are therefore faced with a number of different modes from which to choose. Several studies have attempted to compare the benefits of various modes; however, the majority of them have been too small to enable detection of an outcome benefit of either. In the ARDSNet (2000) study, a mortality benefit was detected between two groups of patients receiving volume-controlled ventilation which may suggest that it is more important to concentrate on the actual settings rather than the particular mode of ventilation.
Regardless of the mode of ventilation chosen, it is clear from the ARDSNet (2000) trial that we should aim for a tidal volume of 6 mL/kg, limiting the peak pressure to 35 cmH2O or plateau pressure <30 cmH2O if receiving volume-controlled ventilation (see Table 1.4).
Mr Kuan Yew is currently being ventilated on a volume-controlled mode which is acceptable when considering recent evidence. However, he is receiving greater than 6 mL/kg of tidal volume. In order to prevent further deterioration in Mr Kuan Yew’s lung function and ventilator-induced lung injury, it would therefore be advisable to gradually decrease his preset tidal volume to closer to that suggested by the ARDSNet trial. When considering the most appropriate tidal volume, it is important to highlight that the ARDSNet (2000) study used predicted body weight which is based on the patient’s sex and height rather than actual body weight.
Permissive hypercapnia
With traditional methods of mechanically ventilating patients with ALI/ARDS, attempts were made to maintain a normal PaCO2 and acid–base balance. Reducing Mr Kuan Yew’s tidal volume to 6 mL/kg, as advocated in the ARDSNet (2000) study, may result in an increase in his PaCO2 and a corresponding decrease in pH, leading to a respiratory acidosis. Over the past ten years, increasing evidence suggests that allowing the arterial PaCO2 to increase above 6 kPa, termed permissive hypercapnia, is safe when used in conjunction with a low-tidal volume, low-pressure ventilation strategy, as long as the pH remains >7.3. Although acidaemia has many physiological effects such as depression of myocardial contractility, systemic vasodilation, increased intracranial pressure and cellular metabolic dysfunction, these have not been demonstrated to be clinically significant. However, permissive hypercapnia is unlikely to be appropriate in patients who have a raised intracranial pressure. The question for the critical care nurse and critical team is therefore which puts the patient at more risk: a high PaCO2 or alveolar distension? Current evidence would suggest that it is the latter. It is important, however, that the critical care nurse remains vigilant in monitoring the PaCO2 and pH via arterial blood gas analysis, and responds to the results in a timely and appropriate manner.
Use of positive end expiratory pressure (PEEP)
PEEP has been shown to improve oxygenation in several ways, encouraging movement of fluid from the alveoli into the interstitial spaces, recruitment of small airways and collapsed alveoli and increasing functional residual capacity (FRC). Its application is now advocated during all modes of mechanical ventilation. Its use is particularly imperative for Mr Kuan Yew, not only as an adjunct to improve oxygenation, but also to prevent further ventilator-induced lung injury. It has been suggested that lung damage can be induced at low lung volumes as well as high lung volumes as a consequence of the production of shearing forces which can occur with the opening and closing of alveoli at low lung volumes during mechanical ventilation. The application of PEEP should reduce the volume of reopening–collapsing tissue and hence reduce the degree of damage (Gattinoni et al. 1995).
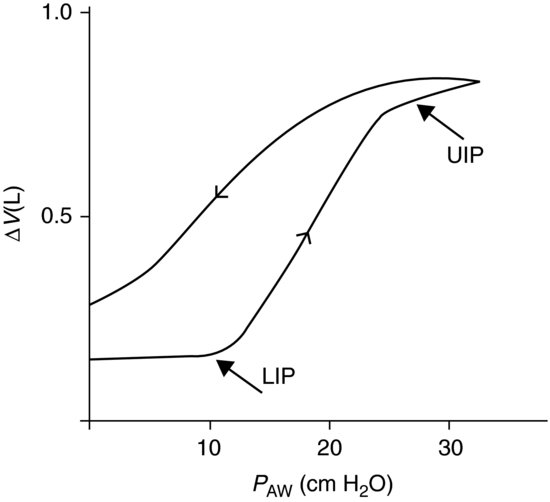
Mr Kuan Yew is currently receiving a PEEP of 5 cmH2O. Controversy exists over what level to set the PEEP in patients with ALI/ARDS and indeed in respiratory failure in general. One method which has been used is to assess the pressure–volume relationship of the lungs (see Figure 1.3).
Figure 1.3 Pressure–volume relationship. (Adapted from Russell J and Walley K (eds) (1999) Acute Respiratory Distress Syndrome: A Comprehensive Clinical Approach. Cambridge University Press, Cambridge.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


