The Nurse in the Faith Community
Objectives
After reading this chapter, the student should be able to do the following:
1. Describe the heritage of health and healing ministries in faith communities.
5. Examine the professional issues related to faith community nursing.
Key Terms
congregants, p. 983
congregational model, p. 972
faith communities, p. 970
faith community nurse, p. 970
faith community nursing, p. 970
faith community nurse coordinators, p. 976
healing, p. 972
health cabinet, p. 972
health ministries, p. 971
holistic care, p. 972
holistic health center, p. 973
institutional model, p. 972
parish nurse, p. 970
parish nursing, p. 970
partnership, p. 974
pastoral care staff, p. 979
polity, p. 982
wellness committee, p. 972
—See Glossary for definitions
 Jean C. Bokinskie, PhD, RN
Jean C. Bokinskie, PhD, RN
Dr. Jean C. Bokinskie is an assistant professor at the Department of Nursing at Concordia College in Moorhead, Minnesota, and serves as the director of the Concordia College Parish Nurse Center. She teaches both didactic and clinical courses in adult health nursing in the undergraduate nursing program. She has also served as a parish nurse in her home congregation of Hope Lutheran Church since 1996. Dr. Bokinskie has been involved in the educational preparation of faith community nurses since 2000. In her role as Program Director, she provides consultative services to many faith communities for the initiation, development, and support of faith community nursing and health ministry programs. Dr. Bokinskie is active in updating the international curriculum for parish/faith community nurse preparation and in the current revision of the Scope and Standards document. She is an author and conference presenter for nurses and related health and healing professionals on faith community nursing/health ministries, both regionally and nationally. Her research interest areas include work place environments, perceptions of empowerment, outcome measures of faith community nursing actions, and resilience of individuals who have experienced spinal cord injury.
Faith community nursing or parish nursing is the dynamic process of working with faith communities to promote wholeness of body, mind, and spirit (Patterson, Wehling, and Mason, 2008). This specialty nursing practice has long-established roots in the healing and health professions. Throughout historical accounts of nursing, caring for members of communities has been important. The earliest accounts of caring and serving others stem from communities of faith. Religious texts abound with reference to the importance of caring for others as a foundational component of the faith tradition. Wholeness and being a in relationship with one’s creator have sustained individuals and groups during times of illness, brokenness, and stress, and when cure was not possible (Hale and Koenig, 2003; Solari-Twadell and McDermott, 2006). In 1998 the American Nurses Association (ANA) accepted parish nursing as the most recognized term for the practice of nurses working with congregations or faith communities as published by the Health Ministries’ Association (HMA) and the ANA in the Scope and Standards of Parish Nursing Practice (HMA/ANA, 1998). In the 2005 revision of the ANA’s Scope and Standards of Practice, the term faith community nurse was adopted to be inclusive of the titles of parish nurse, congregational nurse, health ministry nurse, or health and wellness nurse (ANA/HMA, 2005). Currently the majority of faith community nurses serve in Judeo-Christian communities; however, the practice is expanding to other faith traditions as it attempts to respond to diverse faith perspectives and international needs (IPNRC, 2009a).
Faith community nurses work in close relationships with individuals, families, and faith communities to establish programs and services that significantly affect health, healing, and wholeness (Chase-Ziolek, 2005; Solari-Twadell and McDermott, 2006; Patterson, Wehling, and Mason, 2008). Faith community nurses balance knowledge and skill in their role in order to facilitate the faith community as it becomes a caring place—a place that is a source of health and healing for all members of the community. Nurses are drawn into faith community nursing because it encourages the expression of spirituality as a part of health and healing, whereas others become faith community nurses out of a sense of vocational calling (Mosack, Medvene, and Wescott, 2006).
Faith community nurses address health concerns of individuals, families, and groups of all ages. The members of faith communities, like other communities, experience birth, death, acute and chronic illness, stress, dependency concerns, challenges of life transitions, growth, and development; they also face decisions regarding healthy lifestyle choices. Serving as good stewards of resources, faith community nurses encourage partnering with other community health agencies, as well as lay and professional church leaders, to arrive at creative responses to health issues and to develop health promoting and spiritually healing activities. The nurse serves the faith community by focusing on the needs of the individual parishioner, the entire faith community, and the surrounding geographic area with attention to spiritual needs.
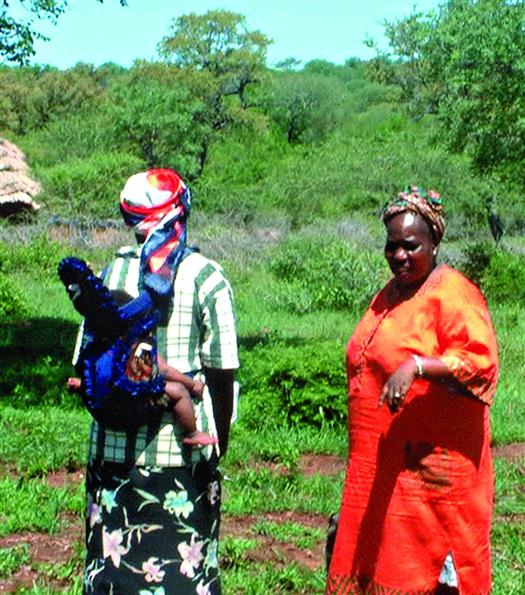
Faith community nursing continues to gain prominence as nurses reclaim their traditions of healing, acknowledge gaps in service delivery, and, along with the rise of nursing centers, affirm the independent functions of nursing (Nist, 2003; Solari-Twadell, 2006). The International Parish Nurse Resource Center (IPNRC) estimates that about 12,000 faith community nurses are practicing in all 50 states (IPNRC, 2009b). This estimation reflects a rather conservative estimate since it only includes the numbers reported by IPNRC-affiliated educating bodies and does not reflect the individuals who have completed non-affiliated IPNRC programs or who practice without additional education in the specialty area. Box 45-1 provides a demographic profile of a large sampling of parish nurses in the United States. In addition, the numbers of practicing faith community nurses continue to grow in other countries such as South Korea, Canada, New Zealand, Swaziland (Figure 45-1), Russia, and the United Kingdom (Daniels, 2009).
Definitions in Faith Community Nursing
Faith communities are groups of people that gather in churches, homeless shelters, congregations, parishes, synagogues, temples, or mosques and acknowledge common values, beliefs, and practices within a single faith or multi-faith tradition(s) (ANA/ HMA, 2005). It is a setting in which the members or guests are invited, but are not obligated, to participate in the rites and rituals of a faith tradition.
Parish nursing has been the most commonly used expression for the specialized practice of professional nursing in this context; however, the more inclusive term of faith community nursing, as adopted by the ANA and the HMA, better reflects the growing practice. The practice of faith community nursing is defined as the “practice of professional nursing that focuses on the intentional care of the spirit” in promoting “wholistic” health and prevention of illness (ANA/HMA, 2005, p 1). In addition, the practice is governed by each state’s nurse practice act and standards of practice.
Faith community nurses respond to health and wellness needs within the context of populations of faith communities and are partners with the faith community in fulfilling the mission of health ministry in the intentional care for the spiritual needs of the population. The faith community includes persons throughout the life span. This includes active and less-active members, as well as those confined to home or those living in institutional settings. Often, the faith community’s mission includes outreach to individuals and groups. These individuals or groups may be found in a geographic area near the traditional congregational setting, or in a common cultural community. These individuals or groups may not be designated members of the faith tradition. However, services may be extended to those beyond the congregational setting.
Health ministries are those activities and programs in faith communities organized around health and healing in order to promote wholeness in health across the life span (Chase-Ziolek, 2005). Health ministry services may be specifically planned or may be more informal. A professional or a layperson may provide them. These services include visiting the homebound, providing meals for families in crisis or when a family member returns home after hospitalization, participating in prayer circles, serving “healthy heart” meals, or holding regular grief support groups (Hale and Koenig, 2003). As a member of the health ministry team, the parish nurse emphasizes the nursing discipline’s intentionality to include the spiritual dimension while incorporating physical, emotional, and social aspects of nursing with individuals, families, and faith communities.
Faith community nurse models that have been widely implemented include congregation- and institution-based models. In the congregational model, the nurse is usually autonomous. The development of a faith community nurse/health ministry program arises from the individual community of faith. The nurse is accountable to the faith community and its governing body. The institutional model includes greater collaboration and partnership; the nurse may be in a contractual relationship with hospitals, medical centers, long-term care establishments, or educational institutions. In either model, nurses work closely with professional health care members, faith community pastoral staff, and lay volunteers. To promote healing, the nurse builds on strengths to encourage the connecting and integrating of inner spiritual knowing and healthy lifestyle choices to achieve optimal wellness in the many circumstances faced by individuals and families in life. Intentional and compassionate presence of a spiritually mature professional nurse in individual or group situations is vital. In this role, providing holistic care with congregation populations is important. Holistic care is concerned with the relationship between body, mind, and spirit in a constantly changing environment (Dossey, Keegan, and Guzzetta, 2005). The nurse and members of the congregation assess, plan, implement, and evaluate programs. The process of realizing holistic care is enhanced by an active wellness committee or health cabinet with members who are fully engaged in health ministry (Chase-Ziolek, 2005). These committees are most effective when members represent the broad spectrum of the life of the church. An active wellness committee provides leadership and influence throughout the faith community; ideas are not from one individual but generated out of a committee structure (McNamara, 2006). The faith community nurse uses all the knowledge and skills of this specialty to provide effective services. The outcome is a truly caring congregation that supports healthy, spiritually fulfilling lives. Resources for faith community nursing can be found on this book’s Evolve website.
Historical Perspectives
Faith Communities
In the roots of many faith traditions are concerns for justice, mercy, and the need for spiritual and physical healing. The appeal for caring, the healing of diseases, and acknowledging periods of illness and wellness is universal. Religion plays an important role in the lives of many individuals. In a 2005 poll, 64% of Americans described themselves as being religious and the same percentage indicated that they prayed daily (Adler, 2005). The relationship between spirituality, religion, and health is emerging as an important topic for nursing research. Schlundt and colleagues (2008) reported a positive association between religious involvement and perceptions of overall health, physical activity, healthy lifestyle behaviors, yet negative associations with eating patterns. An important aspect of living out one’s spirituality and religion is being a part of a community of faith from birth to death, throughout wellness and illness (Figure 45-2). Whether participating as individuals or as families, all benefit from association with a supportive faith community or congregation through enhanced happiness, peace, hope and purpose (Koenig, 2009).
The biblical account of Phoebe (Romans 16:1-2) exemplifies the tradition of health and healing within a congregation. In addition, many Old Testament accounts and healing stories in the New Testament provide additional faith foundations (Psalms 106, 107, 113; Mark; Luke; Acts). The charge of the early Christian church was to preach, teach, and heal. The church provided access to services such as shelter and food; the church tended to wounds and offered comfort and safety. So, too, nuns, deacons, and deaconesses from the Christian tradition are all examples of the healing professions serving in communities as they encounter more caring congregations.
The origins of wholeness and salvation are derived from similar concepts of sodzo (Greek) and shalom, or wholeness. These terms and harmony in health are common to most faith communities. Writings in Christian and Jewish sources address the individual and community relationships with God as the source for a wise use of resources of self, environment, and one’s community. Hygiene, health, and healing were a part of the Holiness Code of Leviticus. Throughout history, health existed at the center of the interaction between one’s creator and humankind. The integration of faith and health within the caring community results in beneficial outcomes. Persons who encounter physical and emotional illness and who are able to call upon their faith beliefs and religious traditions are able to increase coping skills and realize spiritual growth. In a study of African-American men, prayer, spirituality, and trust in a higher power were important health maintenance strategies (Ravenell, Johnson, and Whitaker, 2006). In a study exploring perceived burden of caregivers, religious involvement in general, and church attendance in particular, seemed to provide both spiritual and social psychological benefits to dementia caregivers (Sun et al, 2009).
Using strengths from earliest memories of faith traditions and previous learning experiences, as well as the ability to accept support from family and friends, helps individuals and groups to interpret brokenness, disasters, joys, births, deaths, illness, and recovery. Encouraging growth in faith beliefs and honoring traditions and rituals of the faith community bring individuals, families, and congregations in closer connection with their creator. The consolation of sacred liturgies, religious rituals, sacred space, and communal events aids the grieving and the healing process; they also affirm transcendent life (O’Brien, 2003; Dossey, Keegan, and Guzzetta, 2005).
Some of the major Christian faith communities in the late nineteenth and early twentieth centuries used missionaries to develop multipurpose activities in communities, which included health activities and education along with religious messages. Hospitals were built in the United States and abroad, and underserved populations were targeted. As political and economic forces have changed through the years, health ministry strategies of faith communities have altered their approaches. Some faith groups have identified with community development efforts to help empower people to meet their needs for food, education, clean environments, social support, and primary health care. Congregations have also recognized the need to increase awareness in several areas including one’s personal responsibility for healthy choices; the escalating cost of health care and the need for cost containment; the increasing numbers of the uninsured and underserved; the issues of domestic violence and substance abuse; and the ever-increasing dilemma of interpreting the complex changes within the health care delivery system.
The governing bodies of various faith communities have supported these efforts by endorsing statements related to health and wellness (ELCA, 2003; LCMS, 2003). The Presbyterian Church (USA) is cited as an example of a long-standing tradition of encouraging members to be good stewards or responsible managers of body, mind, the environment, and total resources. Studies in the late 1980s, the publication of essays titled “Health Care and Its Costs,” and the meetings of the Task Force on Health Costs and Policies resulted in a 1988 policy statement, Life Abundant: Values, Choices, and Health Care (OGA, 1988). Congregations were asked to responsibly model holistic and compassionate concern for health and the provision of care. Furthermore, the policy statement endorsed employing parish nurses or other health professionals as agents of the congregation’s mission to encourage the role of “communities of health and healing” (OGA, 1988, p 20). Similar efforts are present in the Episcopal Church USA, the United Church of Christ, the Catholic Church, and other national faith communities.
The revival of modern faith community nursing occurred in the 1940s when the Reverend Granger Westberg began to explore ways to address wholistic healing through the body-mind-spirit connection (1987). Believing that congregations should have a key role in wholistic health care, Westberg (1990) and his colleagues developed holistic health centers within faith community settings. He stated, “Care for all of the people of God is a part of the church’s mission, of its understanding of the Christian gospel” (Westberg, 1990, p 9). The holistic health centers of the 1970s were a pivotal development that connected hospitals and faith communities and highlighted the role of the nurse in health and wellness promotion (Westberg, 1990). As Westberg noted, “It was clear that the nurses in each of these centers were the glue that bound these three professions together in a common appreciation of the healing talents of each” (1999, p 35). The centers emphasized a comprehensive team approach to total health care and holistic health care. The teams included physicians, nurses, and clergy working with families to encourage personal responsibility for health (Westberg, 1990).
The formulation of parish nursing in the early 1980s built on the strengths of these holistic health centers and focused on the nurse–clergy team working with individuals and their families. Nurses used their abilities to listen to the spoken and unspoken concerns of individuals and made assessments and judgments that were based on their knowledge of the health sciences and humanities. By the mid-1980s, Lutheran General Hospital and Reverend Westberg embarked on a pilot project with six Chicago congregations that included four Protestant and two Roman Catholic communities (Solari-Twadell and McDermott, 2006). Loyola University and Swedish Covenant Hospital were among the forerunners in revitalizing the nurse’s role in the healing traditions; acknowledging the importance of body, mind, and spirit connections; incorporating education; and providing health promotion services within congregations.
Health Care Delivery
Early chapters in Parts 1 and 2 of this text familiarize the reader with the historical, economic, social, political, environmental, and ethical perspectives and influences on health care. The health care delivery system is challenged to work within parameters of tighter financial constraints while welcoming advanced technology and addressing new health concerns. Current health care reform reflects a shift in health care delivery to a more comprehensive wellness-focused program (ANA, 2010a). Faith community nurses are well positioned to provide holistic community-based care for vulnerable and underserved populations and to collaborate with care providers.
The following are examples of issues that are important to this chapter. After major hospitalizations, clients may return to their homes very sick with few, if any, care providers available. Caregivers are faced with the multiple tasks of managing finances, maintaining family responsibilities, and learning care-giving skills. Fragmented care and inadequate caregiver training and availability are problems for the disenfranchised, underserved, and uninsured, as well as for the economically well-situated and better-educated persons. Families are challenged to seek the best ways to meet the multiple demands of young children, teens, and aging parents whether in the metropolitan, micropolitan, or rural environment.
Consumer demand for involvement in health care decisions continues to increase, and society emphasizes individual responsibility for health. Simultaneously, consumers have increased interest in their own well-being and have expressed needs for health information to be available in a variety of formats (Loeb, O’Neill, and Gueldner, 2001; McGinnis and Zoske, 2008; Beacom and Newman, 2010). In addition to consumer interest and a heightened awareness of responsibility for one’s own health, health care providers and managed care systems have found it financially advantageous for their participants to be healthy and remain out of the system. Thus, with rising costs of care, scarce resources for populations, and the complex system demands on individuals and families to seek health care, the challenge for the consumer now is how to cope with these forces.
The traditional health care delivery model will not meet the burgeoning needs of the future. The skills of professional nurses, such as faith community nurses, will become more important with the provision of health care services in non-traditional settings (McGinnis and Zoske, 2008). However, it is important to differentiate the unique practice of faith community nursing from other community-based specialty practices. Faith community nursing shares many similarities with home health, hospice, and public health nursing; but it is also shaped and guided by the worshipping community’s traditions, rites, and rituals.
A primary focus of all nurses in the last few decades has been to coordinate care and to link health care providers, groups, and community resources as the client tries to understand diverse health plans. Negotiating with individuals, agencies, and community partnerships within the complex maze of the broader health care environment demands a knowledgeable and seasoned professional. Nurses are aware of the necessity of collaborative practices and the formation of partnerships to care for groups and individuals throughout the age span. These nurses recognize the need for diverse ways to address health promotion and disease prevention at all levels. They advocate for healthy lifestyle choices in exercise, nutrition, substance use, and stress management. They realize that information and guidance must be available via media, in schools, workplaces, faith communities, and residential neighborhoods. Faith community nurses need to partner with others as they serve populations through faith communities (Chase-Ziolek, 2005).
Holistic Health Care
Holistic health practices emphasize nurses’ and clients’ embrace of a commitment to optimal wellness. Such practices focus nurses and clients on seeking the meaning of wellness for the individual or situation, and on considering options from an array of therapies. Harmony between the physical, emotional, psychological, and spiritual self is sought. In addition to sharing backgrounds and functions similar to those of public health nursing, faith community nursing also parallels and benefits from commonalities and distinct practices of holistic nursing. Regardless of specialty or practice setting, nurses who practice in a holistic manner acknowledge wholeness as more than the sum of the individual parts (Dossey et al, 2005). The philosophy of holistic nursing practice (which is a subspecialty in nursing) embraces concepts of the presence, healing, and holism. The interconnectedness of body, mind, and spirit is basic to holistic nursing and is embedded in the practice of faith community nurses. Like faith community nursing, holistic nursing emphasizes wholeness of persons across the life span.
The current standards of holistic nursing practice were approved by the American Holistic Nurses Association (AHNA) in 2000 (updated 2007) and contain five core values. These standards provide guidelines for practice, education, and research. The standards are a guide for all professional nurses, as are the five assumptions that underlie faith community nursing as found in Faith Community Nursing: Scope and Standards of Practice (ANA/HMA, 2005). Faith community nurses will find them helpful in embracing more holistic practices and interventions. Faith community nurses have already used some of the interventions commonly found in holistic nursing, and additional exploration by faith community nurses enhances practice possibilities to promote wellness and healing for practitioner and client (Denton, 2005). Both faith community nurses and holistic nurses share the skill of creating a healing environment (Dossey et al, 2005). Listening coupled with intentional compassion is basic to effective interventions. Selected interventions that are often used in both specialties of nursing are prayer, meditation, counseling, guided imagery, health promotion guidance, journaling, therapeutic touch, healing presence, and massage. Information about accessing AHNA can be found on this book’s Evolve website.
Faith Community Nursing Practice
Characteristics of the Practice
As in the early history of the development of public health nursing in this country, faith community nurses found that health promotion services were needed in underserved urban and rural areas (Baldwin et al, 2001; Wallace et al, 2002). Nurses identified gaps in the delivery of service. They found that congregants residing in communities that offered access to adequate health services also requested and benefited from health counseling and health promotion services at all levels of prevention.
The faith community nurse services emphasized health promotion and disease prevention and provided the benefits of holistic care through the supportive, caring faith community. Nurses acknowledged the inner strength and spirituality of persons and groups to increase healing. The nurses developed effective skills in negotiation, collaboration, and leadership. They also honed astute non-verbal and verbal communication skills. They embraced the vital role of families for healthy outcomes, and parish nurses knew that community support augmented the interventions chosen by individuals and families. Working with the congregation as the population group, parish nurses attempt to include in the wellness programs those persons who are less vocal or visible in the community of faith. The spiritual dimension of health was and is optimized by complementing the nursing role with pastoral care.
Faith communities and nurses have formed new and unique partnerships in response to societal and institutional needs (Hickman, 2006). Coalitions of networks were important as faith communities developed into centers of support and caring. Faith community nurses also began to affiliate with coalitions of inner city churches, networks of rural churches, individual hospitals, chaplaincy programs, and health departments. If the vision or mission of the congregation extended beyond its immediate membership, those outside of the immediate faith community who would benefit from the services are also potential recipients. Nurses then included arrangements with nearby community centers, visiting nurse associations, homeless shelters, community health centers, or forms of neighborhood nursing associations. Some nurses work with one or more faith communities and with one or more religious traditions.
Nurses in any of these arrangements consider the environment and population characteristics of congregations and the community. The strengths and assets of the congregation are the building blocks for services, and because faith communities traditionally value the talents and gifts of their members, efforts flourish within and beyond the faith community. Faith community nurses address the identified needs for health promotion and disease prevention, and they understand the importance of the body-mind-spirit connection with a primary focus on spiritual care. Table 45-1 details the phases of faith community nurse program development.
TABLE 45-1
PHASES OF FAITH COMMUNITY NURSE PROGRAM DEVELOPMENT
| PHASE | CHARACTERISTIC |
| Recognizing | Nurses describe a calling and desire to have a holistic practice |
| Preparing | Personal development: seek information and affirmation |
| Professional development: educational preparation | |
| Coalition building: paving the way with the faith community | |
| Planning | Assess community needs, market ideas, elicit volunteers, set goals |
| Work with leaders, determine available resources, partnerships | |
| Implementing | Team building, support and manage volunteers, self-development |
| Evaluating | Record keeping, outcome summaries |
From Farrell SP, Rigney DB: From dream to reality: how a parish nurse program is born, J Christian Nurs 22:34-37, 2005.
To support the faith community nurse, the International Parish Nurse Resource Center (IPNRC) was established in 1986. The center’s mission is the promotion and development of quality faith community nurse programs through research, education, and consultation (Patterson, 2003). Establishment of the philosophy, mission, assumptions, and strategic purpose of the specialty was conceived with the guidance of the IPNRC. In addition, core curricula as standard preparation for faith community nurses and coordinators were developed and continue to be revised (Patterson, 2003; Solari-Twadell and McDermott, 2006). Throughout the years, the IPNRC has been vigilant in addressing emerging issues such as documentation accountability, preparation for parish nurses, and accreditation concerns (related to The Joint Commission [TJC]) for parish nurses connected with institutional hospital systems. The IPNRC sponsors the annual Westberg Symposium for faith community nursing, which is an international forum to present the latest research and practice patterns in faith community nursing. Information about accessing the center can be found on this book’s Evolve website.
The development of programs of study for the new specialty has evolved from the initial adoption of the HMA and ANA’s Scope and Standards of Practice of Parish Nursing Practice (HMA/ANA, 1998) and the revised Faith Community Nursing: Scope and Standards of Practice (ANA/HMA, 2005). The document will be further revised in 2011. Faith community nurses active in the interfaith Health Ministries’ Association (HMA) developed these documents. Professional and laypersons in both health and faith disciplines concerned about health ministries comprise the HMA, which also holds an annual symposium. Members of the faith community nurse section include professional nurse members committed to improving the practice and developing statements of agreement related to faith community nursing. Information about accessing the HMA can be found on this book’s Evolve website.
As advanced practice nurse and faith community nurse practices increase in numbers and varieties of arrangements, evaluation of practice trends within the health care delivery system and the needs of society is necessary. Nursing must be accountable and responsive to those being served, as well as to those who provide opportunities to serve.
The goal of faith community nursing is to develop and sustain health ministries within faith communities. Faith community nursing is community-based and population-focused professional nursing practice with communities of faith to promote whole-person health. Faith community nurses must be fully aware of the beliefs, faith practices, and level of spiritual maturity of congregants served, and they link these with health and healing. Nurses work with a health cabinet or wellness committee to evaluate assets and areas of need in order to plan services that will attain outcomes congruent with goals established by the congregation and faith communities served (Patterson, 2003).
Many faith community nurses function in a part-time capacity and serve as salaried or unpaid staff. If salaried, the average faith community nurse earns around $17.00/hour (McCabe and Somers, 2009; Bokinskie, 2010). Some nurses are responsible for services for several faith communities, whereas others engage in faith community nursing as part of a full-time commitment in other capacities. For example, a nurse might be employed part time as a public health nurse and part time as a faith community nurse in the same community. Alternatively, a nurse employed full time in an acute care setting may spend time serving in an unpaid capacity working in a faith community with a group of other nurses. Depending on the practice model, the nurse has a narrowly defined or a wider realm of responsibility. Faith community nurse practices may be integrated into a health care system or into practices that collaborate with related professional practice areas such as health departments or colleges of nursing. Health care systems employ faith community nurse coordinators, who facilitate different arrangements with several faith communities of varying backgrounds (Hickman, 2006; Zurell and Solari-Twadell, 2006). Both rural and urban settings find these arrangements effective for facilitating health ministry programs (Solari-Twadell and McDermott, 2006). Practices in which several faith community nurses are supervised by a coordinator have built-in opportunities for networking, partnering, and mentoring.
At the first IPNRC-sponsored colloquium held in the early 1990s, five characteristics identified as central to the philosophy of parish nursing (faith community nursing) were conceived by nursing educators and practitioners (Solari-Twadell, 2006):
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree