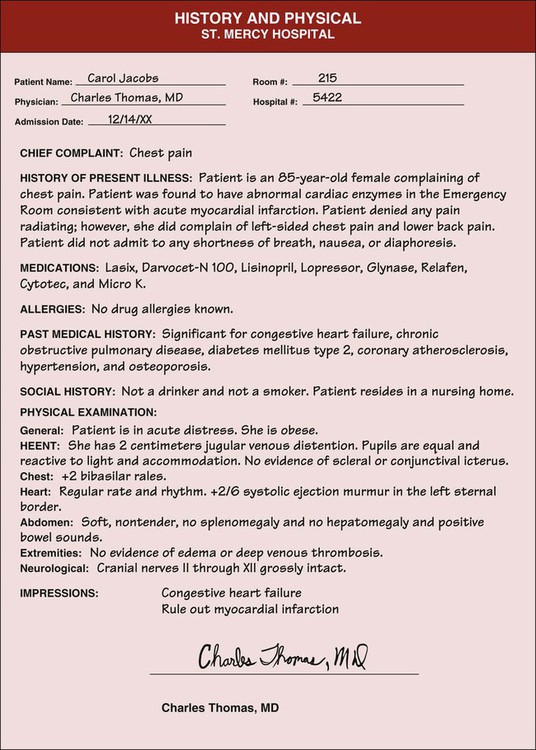
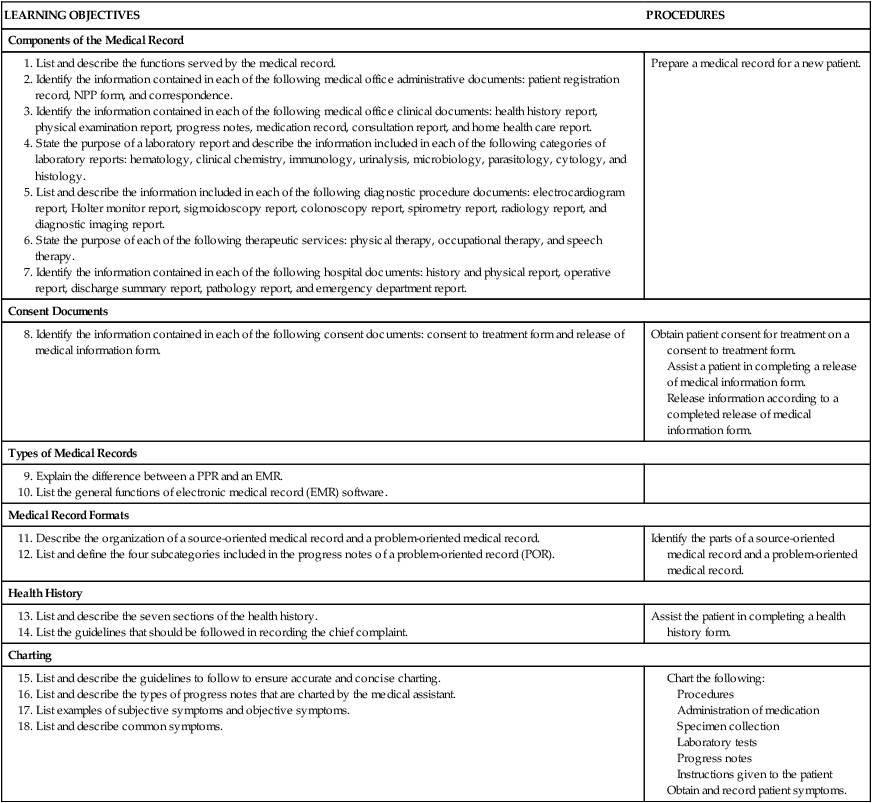
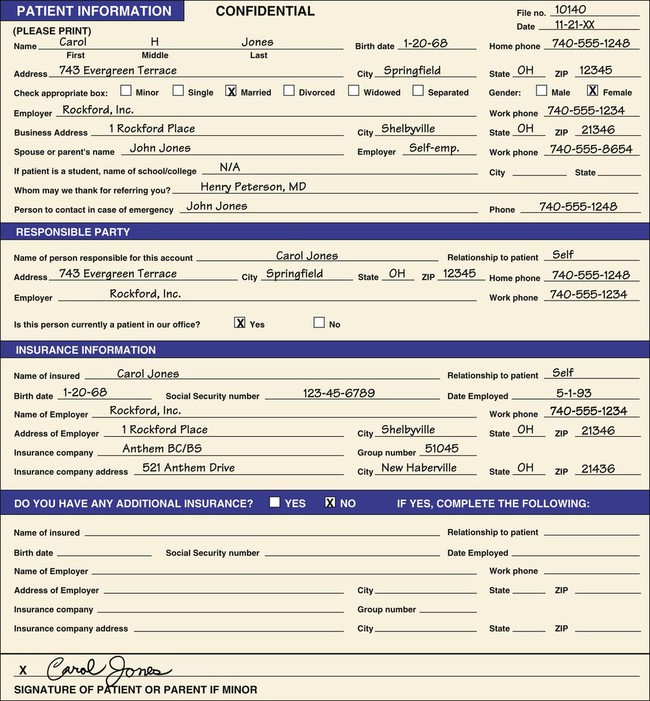
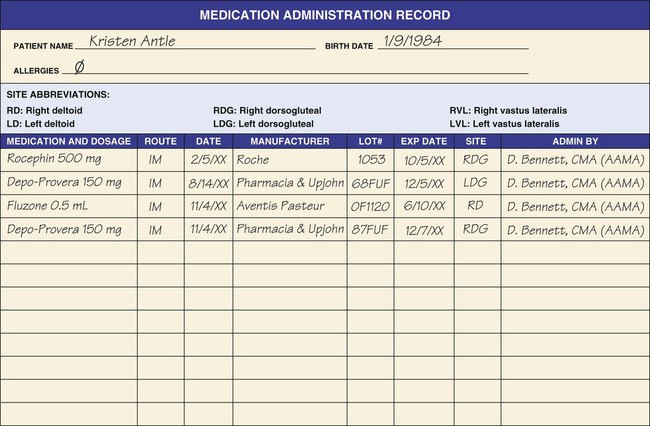
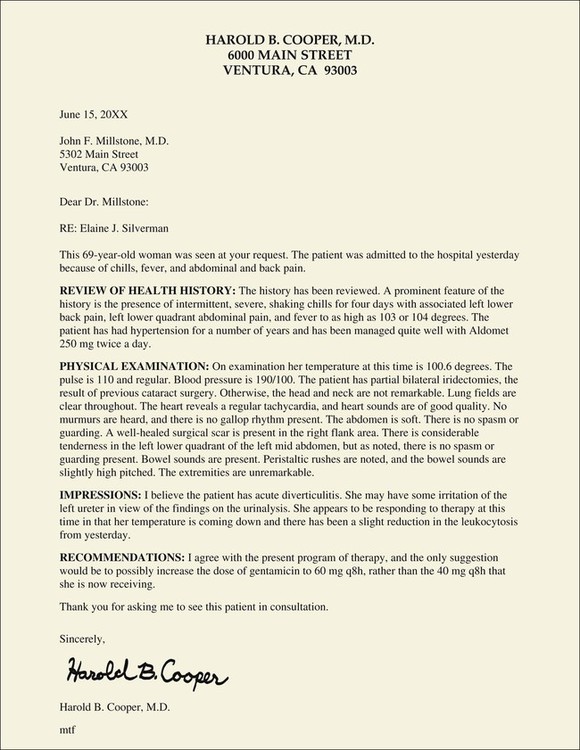
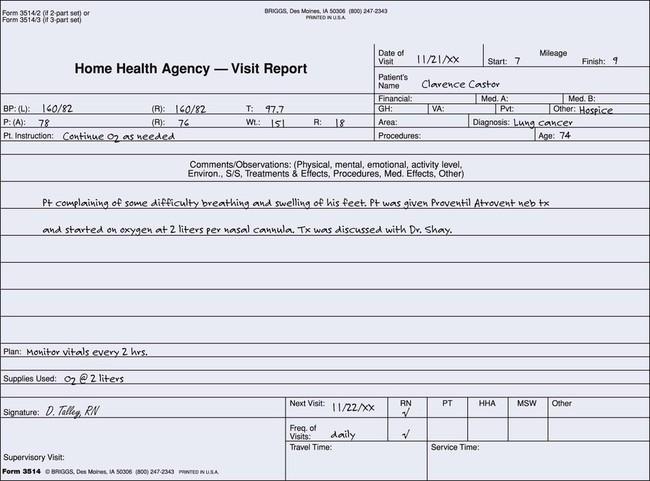
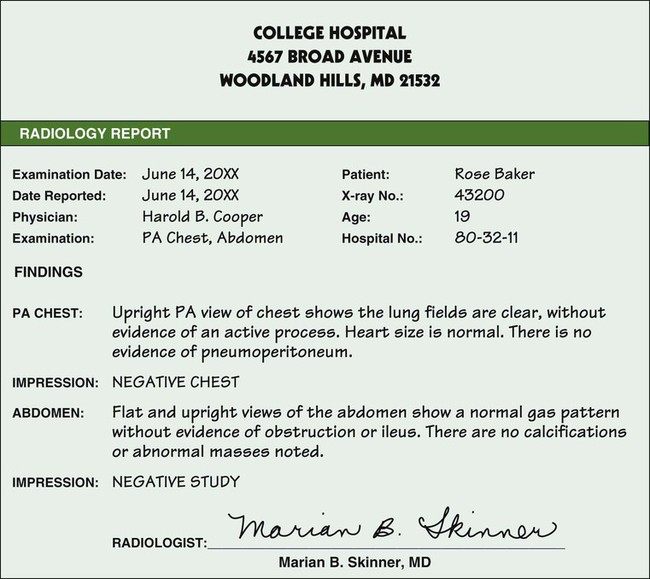
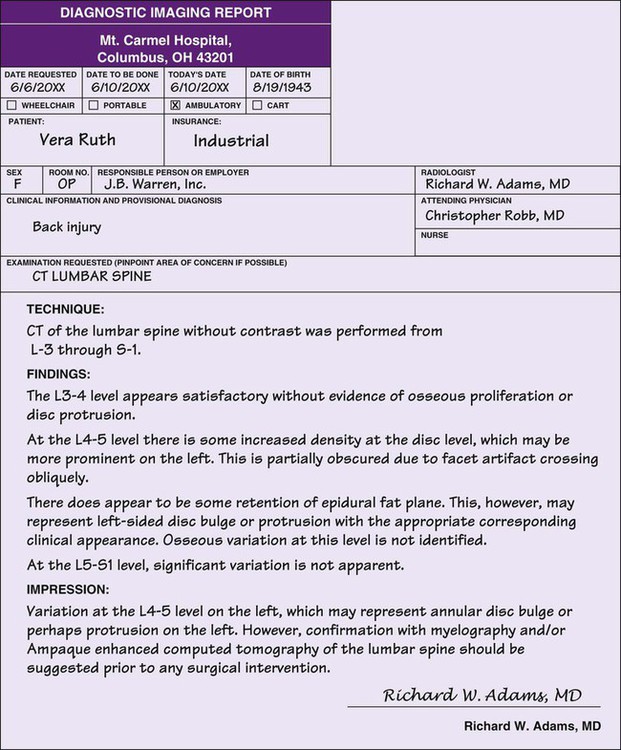
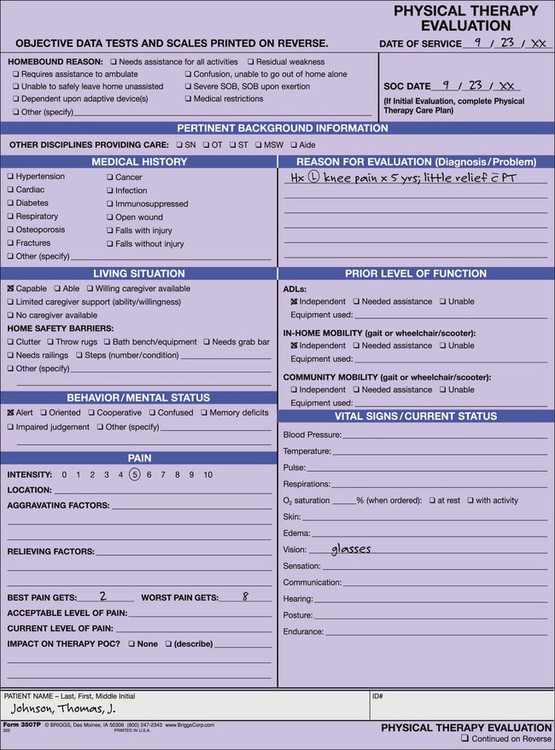
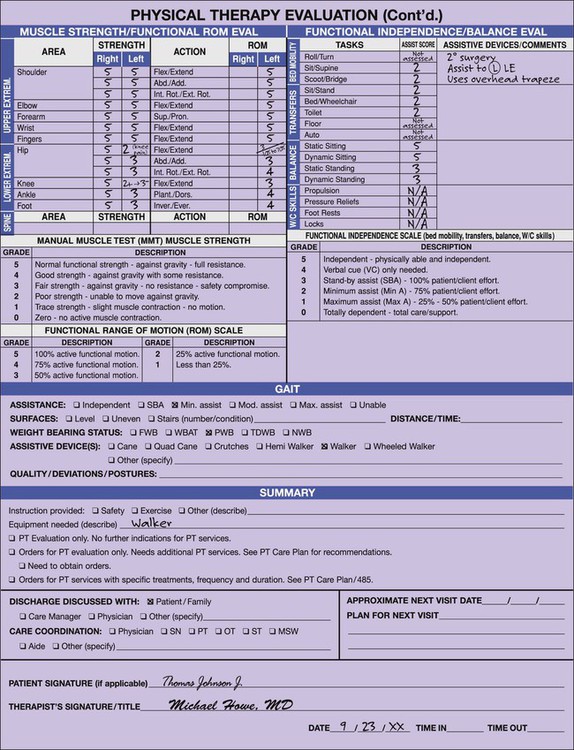
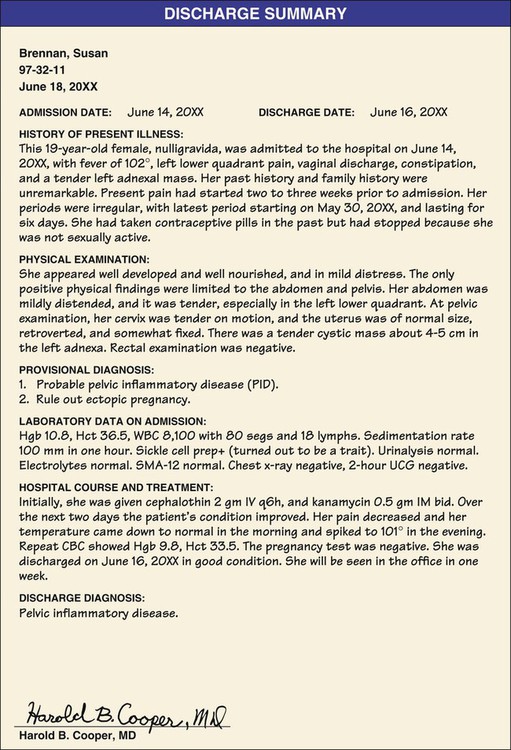
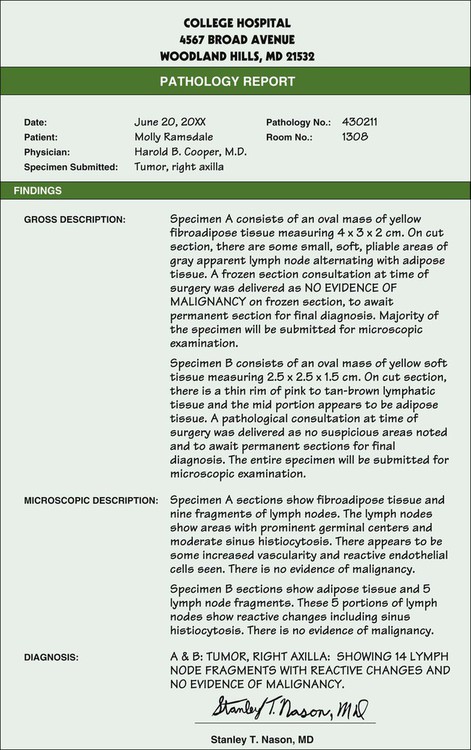
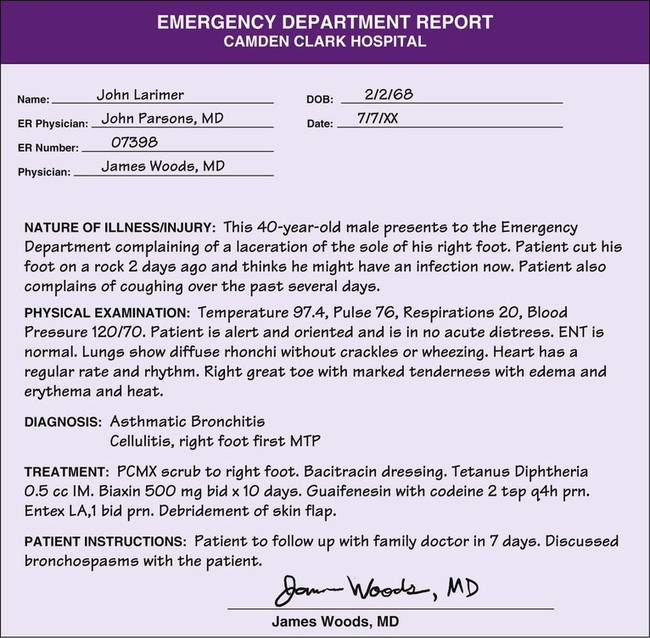
The patient registration record (Figure 36-1) consists of demographic and billing information. All new patients must complete a patient registration record form. After the patient completes the registration record, the medical assistant enters the information into a computer. This allows the demographic and billing information to be used for numerous computerized functions, such as scheduling appointments, posting patient transactions, and processing patient statements and insurance claims. With a paper-based patient record (PPR), the original patient registration record is then usually placed in the front of the patient’s medical record. With an electronic medical record (EMR), the original registration record is usually shredded. A physical examination is an assessment of each part of the patient’s body. The purpose of the physical examination is to provide objective data about the patient, which assists the physician in determining the patient’s state of health. (The physical examination is described in detail in Chapter 20.) A form for recording medications administered to the patient at the medical office (Figure 36-2) includes the following: A consultation report is a narrative report of a clinical opinion about a patient’s condition by a practitioner other than the primary physician, known as a consultant (Figure 36-3). The consultant is usually a specialist in a certain field of medicine (e.g., cardiology, endocrinology, urology). The consultant’s opinion of the patient’s condition is based on a review of the patient’s record and an examination of the patient. The consultation report must include the following: Home health care must be ordered by the patient’s physician and is provided by skilled professionals. Home health care professionals include nurses, home health aides, dietitians, physical therapists, occupational therapists, speech therapists, and social workers. Examples of specialized services available through home health care include cardiac home care, intravenous (IV) therapy, respiratory therapy, pain management, diabetes management, rehabilitation, and maternal-child care. Home health care providers must periodically provide a summary report (Figure 36-4) to the patient’s physician that includes the following: A laboratory report is a report of the analysis or examination of body specimens. Its purpose is to relay the results of laboratory tests to the physician to assist in diagnosing and treating disease. The specific categories of laboratory tests include hematology, clinical chemistry, immunology, urinalysis, microbiology, parasitology, cytology, and histology. A thorough discussion of laboratory documents is presented in Chapter 29. A radiology report is a narrative description of a diagnostic or therapeutic radiologic procedure (Figure 36-5). A radiologist examines the radiograph and provides a written report, which includes a detailed interpretation of the radiograph and his or her impressions. The patient’s physician receives a copy of the radiology report; the actual radiographic film or digital images are kept on file in the hospital’s radiology department but are available for review by the patient’s physician. A diagnostic imaging report is a narrative description of a diagnostic imaging procedure (Figure 36-6). The report includes a detailed interpretation of the diagnostic image, along with the practitioner’s impressions. Examples of common diagnostic imaging procedures include ultrasonography, computed tomography (CT) scan, and magnetic resonance imaging (MRI). The diagnostic computer image is kept on file at the hospital but is available for review by the patient’s physician. Physical therapy involves the use of therapeutic exercise, thermal modalities, cold, hydrotherapy, electrical stimulation, massage, and other physical agents to restore function and promote healing after an illness or injury. A physical therapist might help a football player with a knee injury to regain normal functioning of the knee or assist a patient recovering from a stroke to use his or her legs to walk again. Figure 36-7 shows an example of a physical therapy report. The history and physical report is a physician’s narrative report of the patient’s history and physical examination, along with the physician’s medical impressions (Figure 36-8). The purpose of the history is to document the patient’s current complaints and symptoms, whereas the purpose of the physical examination is to assess the patient’s current health status. Medical impressions, or simply impressions, are conclusions drawn from an interpretation of data. In this case, the physician interprets the data from the health history and physical examination and draws conclusions as to the patient’s state of health. Other terms for impressions include provisional diagnosis and tentative diagnosis. An operative report (Figure 36-9) must be completed for all patients who have had a surgical procedure. This report describes the surgical procedure and must be completed and signed by the surgeon who performed the operation. The operative report must include the following: • Patient identification information • Date and location of the surgery • Names of primary surgeon and assistants • Name of the surgical procedure • Full description of the findings at surgery (normal and abnormal) • Description of the technique and procedures used during surgery • Numbers of packs, drains, and sponges used • Description of any specimens removed • Condition of the patient at the completion of surgery The discharge summary report is a brief (usually one-page) summary of the significant events of a patient’s hospitalization (Figure 36-10). The report must be completed and signed by the attending physician. The discharge summary report includes a concise account of the patient’s illness, course of treatment, and response to treatment, as well as the condition of the patient at the time of discharge from the hospital. The purpose of this report is to document information needed by the patient’s physician to provide for the continuity of future care. It also is used to respond to authorized requests for information regarding the patient’s hospitalization. The discharge summary report must include the following: A pathology report consists of a macroscopic (gross) and a microscopic description of tissue removed from a patient during surgery or a diagnostic procedure. The macroscopic description includes information about the size, shape, and appearance of the specimen as it appears to the naked eye. The report also includes a diagnosis of the patient’s condition (Figure 36-11). A pathologist is required to examine the tissue specimen, complete the report, and sign it. The emergency department report is a record of the significant information obtained during an emergency department visit (Figure 36-12). The report is prepared and signed by the emergency department physician, and a copy is sent to the patient’s family physician for the purpose of providing follow-up care. The emergency department report includes the following: Completion of a consent to treatment form (Procedure 36-1) is required for all surgical operations and nonroutine therapeutic and diagnostic procedures (e.g., sigmoidoscopy) performed in the medical office. The form must be signed by the patient or his or her legally authorized representative and must provide written evidence that the patient agrees to the procedure or procedures listed on the form (Figure 36-13).
The Medical Record
Introduction to the Medical Record
Medical Office Administrative Documents
Patient Registration Record
Medical OFFICE Clinical Documents
Physical Examination Report
Medication Record
Medication Administration Record Form
Consultation Report
Home Health Care Report
Laboratory Documents
Diagnostic Procedure Documents
Radiology Report
Diagnostic Imaging Report
Therapeutic Service Documents
Physical Therapy
Hospital Documents
History and Physical Report
Operative Report
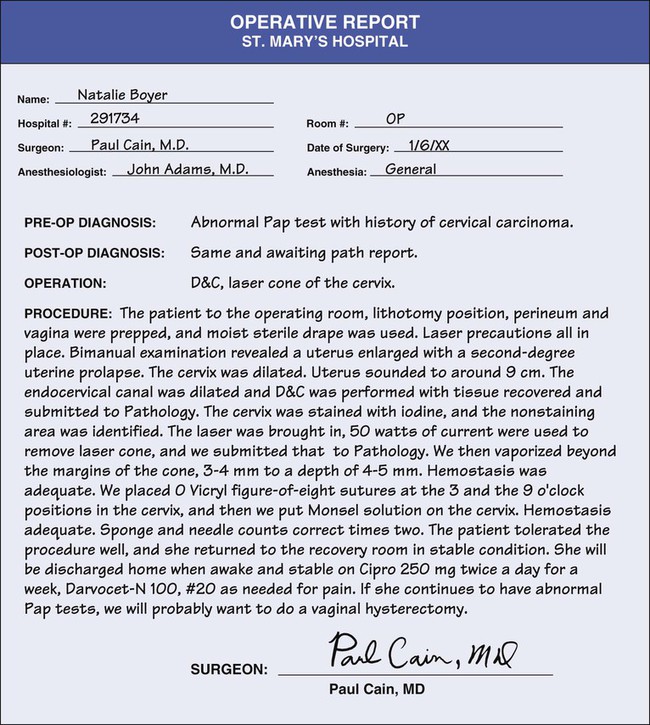
Discharge Summary Report
Pathology Report
Emergency Department Report
Consent Documents
Consent to Treatment Form

The Medical Record
Get Clinical Tree app for offline access