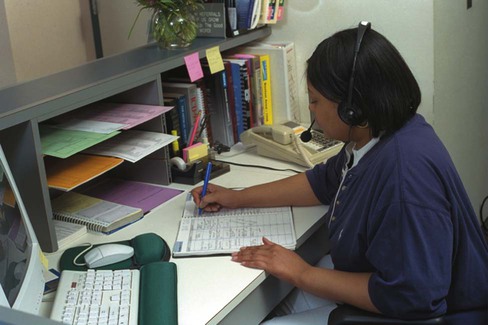
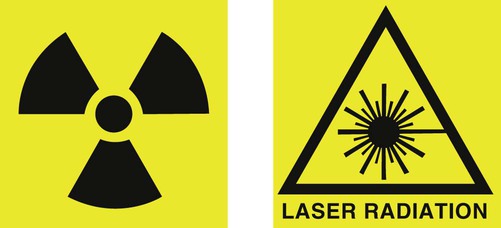
Depending on the size of the administrative area, supplies and equipment for correspondence and billing may be stored in this area, including stationery, envelopes, billing forms, and coding reference books. In addition to the telephone (discussed in detail in Chapter 39), the reception area usually contains a personal computer, which is usually linked to the office’s computer network. Materials for creating new patient folders should also be at hand if a paper medical record system is used. The administrative area needs to have enough room to perform the required activities without the patient files and other papers becoming mixed up, and it must also allow the medical assistant to maintain patient confidentiality (Figure 48-1). • Copayments are expected at the time of service (or some other language regarding the expectation of payment) • The following credit cards are accepted (followed by names of credit cards) • A charge will be added for returned checks to cover any bank fees • Patients will be charged for cancelled appointments unless at least 24-hour notice is given Waste containers and recycling containers should be checked daily and emptied as needed. Biohazard sharps containers should be checked daily and replaced when they are three-quarters full. The plastic liners of biohazard waste containers should be changed as needed. Contracted cleaning services will usually not empty biohazard waste containers because they contain regulated medical waste. The medical assistant must handle biohazard waste containers carefully to prevent an exposure incident. The OSHA Bloodborne Pathogen Standard outlines specific actions to take when handling regulated medical waste. These are outlined in Chapter 17. Storage cabinets, drawers, and bookcases are cleaned less frequently, often on a day when the physician or some of the physicians in the practice are absent so that the room is not in use. After cleaning, the medical assistant should check labels on all items before putting them back on shelves. This is a good time to check for the expiration date on supplies and make a list of any items that need to be ordered or restocked from the general supply area to the cabinet. Outdated supplies must be disposed of properly (Figure 48-2). 1. Manage the environment to reduce hazards. 2. Train employees in general safety and to use correct methods and processes to prevent accident or injury. 3. Maintain equipment and perform regular safety inspections. 4. Create open lines of communication so that mistakes and accidents can be reported without fear of severe consequences. 5. Analyze all incidents including “near misses” to be sure that effective systems are in place. Constant awareness of potential hazards and a culture that expects each employee to respond to potentially unsafe conditions is one of the most effective tools for preventing accident or injury. • Keep work areas, corridors, and hallways clear of obstacles. • Exits should be accessible, clearly marked, and well lit. Be aware of state and/or local requirements for emergency lighting for exit signs. • Keep floors dry, and clean up spills as soon as possible. • Store waste in appropriate receptacles. Remove waste promptly and dispose of medical waste appropriately (see Chapter 17). • Do not create high piles of materials that are likely to fall. Do not climb up on chairs or other unstable objects to retrieve objects stored on high shelves. • Do not allow electrical cords to be present in areas where people walk. The office should have a safety plan, and all employees in the medical office should receive training so that they can carry out their duties correctly. The prevention of the spread of infection is always important. This is discussed in detail in Chapter 17. Equipment should always be checked for frayed electrical cords and used correctly to prevent injury. Hazardous chemicals should be handled and discarded safely as discussed in Chapter 18. Laboratory safety should be maintained according to guidelines in Chapter 29. There should be a plan to respond to spills of blood, body fluids, or chemicals. Areas that are restricted for safety reasons (such as the medical laboratory) should be clearly marked. Employees should report any unsafe condition to their supervisors. Protective equipment is provided by the employer and should always be used by each employee. Chapter 49 will discuss emergency and disaster response in detail. The office should post signs to instruct patients and employees as needed. As defined by OSHA, danger signs indicate that there is immediate danger and special precautions should be taken. These signs must be red on the upper panel with black lettering and a white background. They are more common in construction areas than the medical office. Caution signs warn against potential hazards. They should be predominantly yellow with either yellow lettering on a black background or black lettering on a yellow background. Caution signs should be used if potentially hazardous procedures are performed in the medical office such as x-ray examinations or laser treatments (Figure 48-3). Signs should designate areas where access is restricted. Safety instruction signs (if necessary for employees; e.g., at an eyewash station) should have an upper panel that is green with white lettering. Labels or color-coding should also be used for all biohazard boxes, biohazard waste, and flammable gases. Smoking should not be permitted in a physician’s office, and signs advising patients and visitors that the office is a smoke-free environment should be clearly posted in the waiting area. Exits should be clearly marked, and an emergency evacuation map should be posted near the door to the waiting room. Exit signs should be white with red lettering not less than 6 inches high and Because constant attention is required to maintain a safe environment, it is important to create a procedure to check regularly for potential hazards. A safety checklist is a useful tool for regular safety inspections. It should include the categories to be assessed and have a space to write down any action that needs to be taken. Each part of the office should be checked for adequate lighting, clear walkways, proper storage of supplies, and removal of rubbish and biohazard waste. It is especially important to be sure that heavy boxes have not been stored in a high area where they could fall, that electrical cords are in good repair and do not cause a tripping hazard, and that spills have been attended to promptly. Storage of compressed gases, medications, and chemicals should be assessed according to office policies (Procedure 48-1).
The Medical Assistant as Office Manager
LEARNING OBJECTIVES
PROCEDURES
1. Describe routine maintenance activities in the medical office.
2. Identify methods to maintain a safe environment and prevent injury to patients and employees.
Create an environmental checklist and perform a safety inspection.
3. Describe an efficient system of maintaining equipment inventory lists and operator manuals.
4. Maintain administrative and clinical equipment.
Perform routine maintenance of equipment.
5. Describe the process of obtaining new equipment.
6. Explain procedures for taking inventory.
Take a supply or equipment inventory.
7. Describe an effective method for ordering, receiving, and storing supplies.
8. Explain how to manage office payroll.
9. Describe ways to enhance teamwork in the medical office.
10. Describe the medical assistant’s role in orienting and training new employees.
11. Manage the physician’s professional schedule.
12. Differentiate between medical office policies and procedures.
13. Create and/or revise medical office policies and procedures as needed to promote smooth office functioning.
14. Locate community resources to assist patients and medical office staff.
Locate community resources.
15. Describe how incident reports should be used to protect the medical office.
Complete an incident report.
16. List types of liability protection for physicians, the medical office, and medical assistants.
17. Describe the various components of risk management in the medical office.
Introduction to Medical Office Management
Maintaining the Office
Administrative Area
Waiting Room
Routine Maintenance
General Cleaning
Cleaning Cabinets and Drawers

Patient and Employee Safety
Safe Work Practices
Signs and Instructions
 inch wide. Lighted exit signs should be tested by shutting off the lights in the room; bulbs should be replaced if necessary.
inch wide. Lighted exit signs should be tested by shutting off the lights in the room; bulbs should be replaced if necessary.
Monitoring Environmental Safety

The Medical Assistant as Office Manager
Get Clinical Tree app for offline access






