16 The hepatobiliary and gastrointestinal system
Biliary: Pertaining to the gallbladder and bile ducts.
Cholelithiasis: The presence of a common bile duct stone. Also called chronic cholangitis.
Diarrhea: Rapid movement of fecal matter through the large intestine.
Enteric System: The gastrointestinal tract.
Gastritis: Inflammation of the gastric mucosa.
Nausea: Conscious recognition of subconscious excitation in an area of the medulla closely related to the vomiting center.
Pancreatitis: Inflammation of the pancreas.
Peptic Ulcer: An excoriated area of the mucosa caused by the digestive action of gastric acid; frequently located in the first few centimeters of the duodenum.
Vomiting: A method for the gastrointestinal tract to rid itself of its contents when almost any part of the upper gastrointestinal tract becomes over irritated, distended, or excitable. The physical act of vomiting results when the muscles of the diaphragm and abdomen contract so that the gastric contents can be expelled.
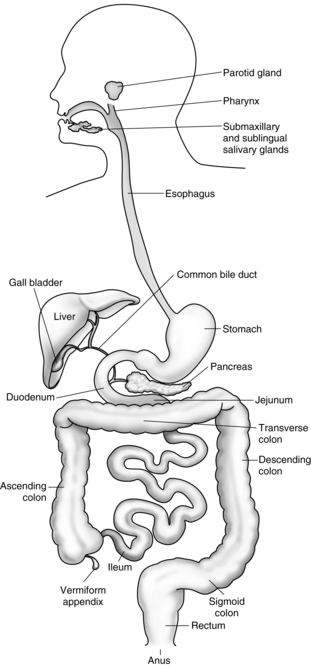
The esophagus
The esophagus is a pliable muscular tube that extends from the pharynx to the stomach (Fig. 16-1). It is located behind the trachea and in front of the thoracic aorta and traverses the diaphragm to enter the esophagogastric junction, sometimes called the cardia. Approximately 5 cm above the junction with the stomach is the lower esophageal sphincter (LES), a circular band of smooth muscle tissue, which functions to prevent the reflux of stomach contents into the esophagus. The normal resting pressure of the LES is approximately 30 torr. This pressure is maintained by stimulation provided by innervation from the vagus nerve. Ordinarily the sphincter remains constricted except during the act of swallowing. Anticholinergic drugs, such as atropine or glycopyrrolate, and pregnancy decrease the resting pressure of the lower esophagus. Drugs that increase the lower esophageal pressure include metoclopramide (Reglan) and antacids. The main function of the esophagus is to conduct ingested material to the stomach.1,2
Disorders of the esophagus
A hiatal hernia occurs when a portion of the upper stomach protrudes or herniates through the diaphragm. Ultimately this causes a stricture or narrowing to form where the diaphragm surrounds the stomach and causes a weakening of the LES. Symptoms of a hiatal hernia include chronic heartburn, pain, and vomiting. Patients with a hiatal hernia need constant observation for active and passive vomiting during the emergent phase of anesthesia. Monitoring patient with a hiatal hernia is especially important if the surgery was performed on an emergency basis when the patient had a full stomach.3
The stomach
The stomach can be anatomically divided into the following three sections: the fundus, the body, and the pyloric portion (Fig. 16-2). The fundus is the dome of the stomach, where peptic juice is secreted. The body is the middle portion of the stomach and is lined with parietal cells that secrete hydrochloric acid. The pH of the solution as secreted is approximately 0.8, which is extremely acidic. The total gastric secretion on a 24-hour basis is approximately 2 L. This volume normally has a pH of 1 to 3.5. Histamine has a major role in hydrochloric acid production by the parietal cells in the stomach, which is an effect mediated by histamine2 receptors, vagal stimulation, and the hormone gastrin. Activation on any one of these receptors potentiates the response of the other to stimulation. Blockade of the activated receptor produces a reduction in acid response because the potentiating effect of the stimulation is reduced. The third portion of the stomach is the pyloric portion, where a thick viscous mucus and the hormone gastrin are secreted. At the end of the antrum is the pylorus, an opening surrounded by a strong band of sphincter muscle that controls the amount of gastric contents that enter the duodenum.
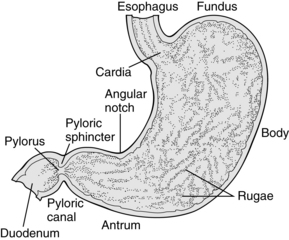
FIG. 16-2 Anatomy of the stomach.
(From Hall JE: Guyton and Hall textbook of medical physiology, ed 12, Philadelphia, 2010, Saunders.)
Nervous and hormonal stimulation have profound effects on gastric volume and pH. More specifically, stimulation of the parasympathetic nervous system causes increased gastric secretion, and stimulation of the sympathetic nervous system causes decreased gastric secretion. Consequently, pain and fear, which activate the sympathetic nervous system, decrease gastric emptying. In addition, the administration of opioids and active labor prolong gastric emptying. Food, depending on the type and amount, passes through the stomach at a variable rate. For example, foods rich in carbohydrates pass through the stomach in a few hours, whereas proteins exit more slowly. The emptying time for fats is the slowest. Fluids, however, pass through the stomach rather rapidly. In fact, 90% of 750 mL of ingested saline solution exits the stomach within 30 minutes. In addition, 150 mL of fluids taken 1 or 2 hours before induction of anesthesia stimulates peristalsis and facilitates gastric emptying. Consequently, the small sips of water taken with the preoperative oral medications may in fact contribute to lower intraoperative and postoperative gastric volumes. It must be emphasized that fasting, regardless of the duration, does not guarantee that the stomach is completely empty of fluids or food.4,5
Effect of pregnancy on gastric motility and secretions
During pregnancy, many alterations occur as a result of the enlarged uterus and altered hormonal state. Because of the enlarged uterus, the stomach and intestine are moved cephalad and the axis of the stomach is shifted to a more horizontal position. The gastric emptying time is increased in women who are at least 34 weeks pregnant. In regard to the gastric volume and pH, no difference between pregnant and nonpregnant states seems to exist. Consequently, pregnant patients who have had nothing by mouth (NPO) for elective surgery do not have any additional risk of aspiration pneumonitis than do nonpregnant patients. However, research findings suggest that pregnant patients who have heartburn may be at greater risk for regurgitation and subsequent development of aspiration pneumonitis. In addition, if intramuscular opioids are given during labor, gastric emptying time is substantially delayed. Epidural anesthesia with local anesthetics does not seem to affect gastric volume or pH; however, if opioids are introduced into the epidural space, a delay in gastric emptying occurs.6,7
Postoperative nausea and vomiting
A great deal of research on PONV over the past few years has yielded drugs that have certainly improved the outcomes of the patient in regard to PONV. The 5-HT3 antagonists, such as ondansetron, tropisetron, granisetron, and dolasetron, competitively antagonize the effect of 5-HT at the 5-HT3 receptor site. Other drug therapies are the antihistamines (promethazine and dimenhydrinate), anticholinergics (scopolamine), neuroleptics (droperidol and triflupromazine), and glucocorticoids, such as dexamethasone. The pathophysiology and pharmacology of PONV is discussed at length in Chapter 29.
With recent research and the advent of new pharmacologic agents, the ability to prevent and efficaciously treat PONV has greatly improved, even for those patients at highest risk for these complications. Under the auspices of the American Society of PeriAnesthesia Nurses, a multidisciplinary panel met to review current literature regarding the prevention and treatment of PONV and formulate a multimodal, multidisciplinary, evidenced-based set of guidelines to guide the practice of those taking care of surgical patients.8 Chief among these recommendations are that each patient should be assessed for the four evidenced-based risk factors for PONV (female gender, nonsmoker, a history of PONV or motion sickness, and administration of postoperative opioids); pharmacologic interventions should be based on the assessed risk for PONV; multimodal interventions, often consisting of more than one pharmacologic intervention targeting different drug receptors are superior to a single intervention; and rescue therapy should consist of administration of a different class of drug targeted at a different set of receptors than the ones given prophylactically.8
The incidence rate for this syndrome is higher in patients who had a full stomach at induction of anesthesia, who underwent intestinal or emergency surgery, or who have a suspected hiatal hernia. The best treatment is prevention. These patients should have a complete return of consciousness before the endotracheal tube is removed. If the endotracheal tube is to be removed in the PACU, the patient should be placed in a lateral position with the head down. Oxygen should be administered, and suction should be available for immediate use before the extubation is performed.9–12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree