45 Care of the obese patient undergoing bariatric surgery
Bariatrics: Branch of medicine dealing with the causes, prevention, and treatment of obesity.
Biliopancreatic Diversion (BD): Surgical procedure that involves reducing the size of the stomach and allowing food to bypass part of the small intestine to change the normal process of digestion.
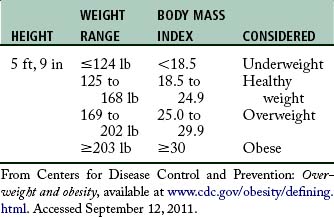
Body Mass Index (BMI): A measure of body fat derived from a formula using a person’s weight and height.
Laparoscopic Adjustable Gastric Banding (LAGB): One of the most common weight loss surgical procedures, it involves placing an adjustable silicone band around the upper portion of the stomach to restrict the size of the stomach. The band is tightened by adding saline through a port that is placed under the skin in the abdomen.
Malabsorptive Procedures: Weight loss surgeries combining the reduction of stomach size, with redirection of the digestive process causing poor absorption of nutrients and calories.
Metabolic Syndrome: A syndrome characterized by several common factors, including abdominal obesity and insulin resistance in which the body cannot use insulin efficiently.
Morbid Obesity: Generally involves a state of being 50% to 100% over normal weight, being more than 100 pounds (45.5 kg) over normal weight, having a BMI of 40 or higher, or being sufficiently overweight to severely interfere with health or normal function.
Obstructive Sleep Apnea (OSA): A sleep-disordered breathing; the risk increases with increased body weight.
Obesity: A condition involving an excess proportion of total body fat. A person is considered obese when his or her weight is 20% or more above normal weight.
Restrictive Procedures: Weight loss surgeries reducing the stomach size limiting the capacity of the stomach to hold food.
Roux-En-Y (RNY): Common gastric bypass surgery that divides the stomach into a small upper pouch leaving a much larger, lower remnant pouch and then rearranges the small intestine into a Y configuration to enable outflow of food from the small upper stomach pouch, via a Roux limb.
Sleeve Gastric Resection (SGR): A newer weight loss surgery that creates a thin, vertical sleeve of stomach using a stapling device, removing the rest of the stomach, thus limiting the amount of food eaten without causing any malabsorption.
Vertical Banded Gastroplasty (VBG): Weight loss surgery also known as stomach stapling, using both a band and staples create a small stomach pouch to restrict food volume.
Weight Loss Surgery (WLS): Procedures that either limit the amount of food a stomach can hold or restrict the amount of food digested.
Obesity is the most common nutritional disorder in the world today. Current estimates suggest that more than one third of the adult population in the United States is affected by excess weight. Approximately 33.3% of adult males, 35.3% of adult females, and 10% to 16.5% of teenagers and children are clinically obese.1 Weight loss surgery is one treatment option for patients who are overweight. Bariatric surgeries increased during 1993 to 2005 from 9189 to more than 140,000 per year.2 Caring for the patient with bariatric concerns presents a number of challenges for the perianesthesia nurse.
Defining obesity
The higher the BMI, the greater the weight associated with a given height (Table 45-1). Recent studies have demonstrated that the patient who is considered overweight and one who is considered moderately obese usually experience minimal risks in the perioperative period.3 Underweight patients, as well as patients with a BMI greater than 30, are found to have increased perioperative mortality rates. Although obesity is not equally distributed across gender or race, the incidence of obesity in a given community is relevant and clinically important. Patients in the obese and morbidly obese categories are seen in perianesthesia services for a wide variety of conditions for a wide variety of services, including surgery.
Physiologic considerations in obesity
Pulmonary
In the general population, undiagnosed obstructive sleep apnea (OSA) is common in obese patients despite awareness that increased abdominal girth is a significant risk factor. Reportedly more than 70% of patients undergoing weight loss surgery have been clinically diagnosed with sleep apnea.4 OSA can occur in patients with redundant pharyngeal tissue. Obstructive sleep apnea is characterized by excessive episodes of apnea (approximately 10 seconds), apneic episodes occurring more than five times per hour, and a 50% reduction in airflow or a reduction sufficient to lead to a 4% decrease in oxygen saturation during sleep as a result of a partial or complete upper airway obstruction. Clinically significant apnea episodes of more than five episodes in 1 hour or 30 per night result in hypoxia, hypercapnia, systemic and pulmonary hypertension, and cardiac arrhythmias. In obese patients with OSA, there is an increased risk of difficult intubations as well as postextubation complications.4
Cardiovascular
A positive correlation exists between an increase in body weight and increased arterial pressure. Hypertension is a known risk factor for the development of coronary artery disease. A weight gain of 28 lb (12.75 kg) can increase the systolic and diastolic blood pressure by 10 and 7 torr, respectively. Systemic hypertension is tenfold more likely in the obese patient. The increase in blood pressure is probably caused by the increased cardiac output.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree