Chapter 10
The Chest
In the beginning the malady [tuberculosis] is easier to cure but difficult to detect, but later it becomes easy to detect but difficult to cure.
Niccolò Machiavelli (1469–1527)
General Considerations
Oxygen enables the breath of life; without adequate lung function, lives cannot be sustained. Patients with pulmonary disease must work harder for adequate oxygenation. These patients complain of “air hunger” or “too little air.” Anyone who has traveled to areas of high altitude, where the oxygen concentration is reduced, has experienced shortness of breath.
The magnitude of pulmonary disease is enormous. Whereas the top two causes of death, heart disease and cancer, have seen a drop in their mortality rate, lung diseases such as chronic obstructive pulmonary disease (COPD) have seen the largest rise of any leading cause of death. COPD is now the third leading cause of death in the United States, surpassing stroke.
The symptoms of COPD include breathlessness, chronic coughing (with or without mucus), wheezing, tightness in chest, and frequent clearing of the throat. Here are the facts:
• A person with COPD dies every 4 minutes in the United States.
• In 2007, COPD cost the United States economy $42.6 billion in direct and indirect costs.
• It is estimated that more than 600 million people worldwide have COPD.
COPD is a preventable and treatable condition. Almost 90% of COPD is due to smoking, and smoking cessation at any age and stage of disease is beneficial.
Cancer of the lung and bronchus is the leading cause of death from cancer in the United States in both men (28% of all cancer deaths) and women (26% of all cancer deaths). In 2011, the American Cancer Society reported that there were 221,130 new cases of lung and bronchus cancer. Cancer of the lung and bronchus is the second most common cancer in men (14%) after prostate cancer and second most common in women (14%) after breast cancer. There were 156,940 deaths, of which 85,600 were deaths in men and 71,340 deaths in women.
The 1-year relative survival for lung cancer increased from 35% in 1975 to 1979 to 43% in 2003 to 2006, largely because of improvements in surgical techniques and combined therapies. However, the 5-year survival rate for all stages combined is only 16%. The 5-year survival rate is 53% for cases detected when the disease is still localized, but only 15% of lung cancers are diagnosed at this early stage. The 5-year survival for small cell lung cancer (6%) is lower than that for non–small cell (17%).
Pulmonary diseases arise when the lungs are unable to provide adequate oxygenation or to eliminate carbon dioxide. Any derangement of these functions indicates abnormal respiratory function.
During a 24-hour period, the lungs oxygenate more than 5700 L of blood with more than 11,400 L of air. The total surface area of the alveoli of the lungs comprises an area larger than a tennis court.
Structure and Physiology
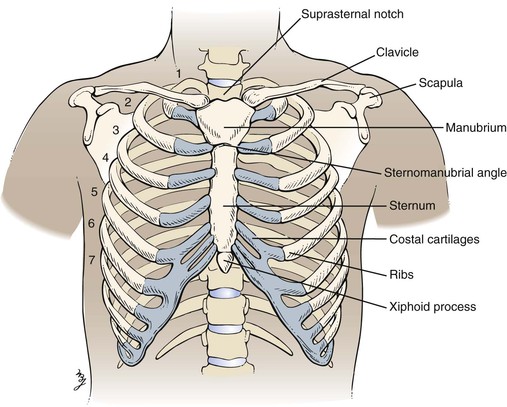
The chest forms the bony case that houses and protects the lungs, the heart, and the esophagus as it passes into the stomach. The chest skeleton consists of 12 thoracic vertebrae, 12 pairs of ribs, the clavicle, and the sternum. The bony structure is illustrated in Figure 10-1.
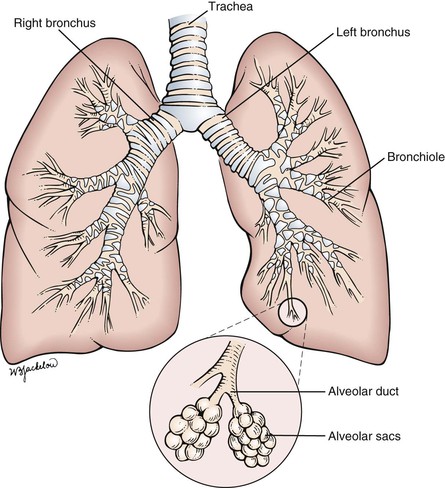
Inspired air is warmed, filtered, and humidified by the upper respiratory passages. After passing through the cricoid cartilage of the larynx, air travels through a system of flexible tubes, the trachea. At the level of the fourth or fifth thoracic vertebra, the trachea bifurcates into the left and right bronchi. The right bronchus is shorter, wider, and straighter than the left bronchus. The bronchi continue to subdivide into smaller bronchi and then into bronchioles within the lungs. Each respiratory bronchiole terminates in an alveolar duct, from which many alveolar sacs branch off. It is estimated that there are more than 500 million alveoli in the lungs. Each alveolar wall contains elastin fibers that allow the sac to expand with inspiration and to contract with expiration by elastic recoil. This system of air-conducting passages is illustrated in Figure 10-2.
The lungs are subdivided into lobes: the upper, middle, and lower on the right, and the upper and lower on the left. The lungs are enveloped in a thin sac, the pleura. The visceral pleura overlies the lung parenchyma, whereas the parietal pleura lines the chest wall. The two pleural surfaces glide over each other during inspiration and expiration. The space between the pleura is the pleural cavity.
To describe physical signs in the chest accurately, the examiner must understand the topographic landmarks of the chest wall. The landmarks of clinical importance are as follows:
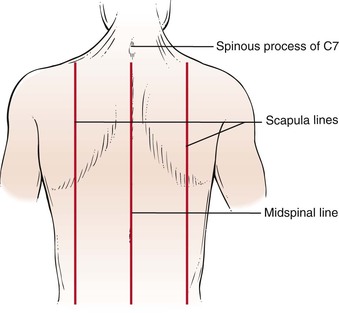
Figure 10-3 illustrates the anterior and lateral views of the thorax, and Figure 10-4 illustrates the posterior thorax.
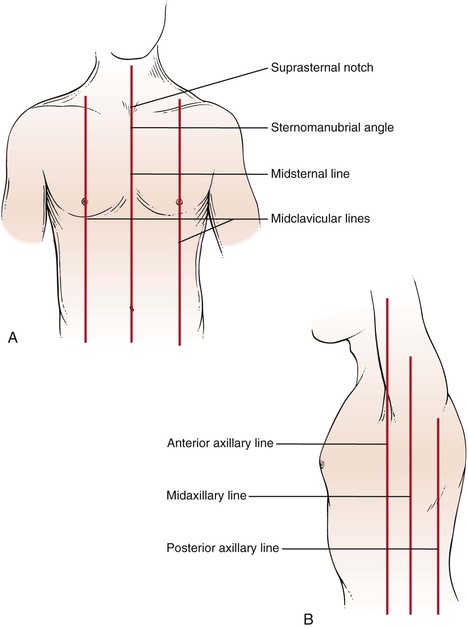
Figure 10–3 Thoracic cage landmarks. A, Topographic landmarks of the anterior thorax. B, Landmarks on the lateral view.
The suprasternal notch is located at the top of the sternum and can be felt as a depression at the base of the neck. The sternomanubrial angle is often referred to as the angle of Louis. This bony ridge lies approximately 5 cm below the suprasternal notch. When you move your fingers off the ridge laterally, the adjacent rib that you feel is the second rib. The interspace below the second rib is the second intercostal space. Using this as a reference point, you should be able to identify the ribs and interspaces anteriorly. Try it on yourself.
To identify areas, several imaginary lines can be visualized on the anterior and posterior chest in Figures 10-3 and 10-4. The midsternal line is drawn through the middle of the sternum. The midclavicular lines are drawn through the middle points of the clavicles and parallel to the midsternal line. The anterior axillary lines are vertical lines drawn along the anterior axillary folds parallel to the midsternal line. The midaxillary lines are drawn from each vertex of the axilla parallel to the midsternal line. The posterior axillary lines are parallel to the midsternal line and extend vertically along the posterior axillary folds. The scapular lines are parallel to the midspinal line and pass through the inferior angles of the scapulae. The midspinal line is a vertical line that passes through the posterior spinous processes of the vertebrae.
Rib counting from the posterior chest is slightly more complicated. The inferior wing of the scapula lies at the level of the seventh rib or interspace. Another useful landmark can be found by having the patient flex the neck; the most prominent cervical spinous process, the vertebra prominens, protrudes from the seventh cervical vertebra.
Only the first seven ribs articulate with the sternum. The eighth, ninth, and tenth ribs articulate with the cartilage above. The eleventh and twelfth ribs are floating ribs and have a free anterior portion.
The interlobar fissures, illustrated in Figure 10-5, are situated between the lobes of the lungs. Both the right and the left lungs have an oblique fissure, which begins on the anterior chest at the level of the sixth rib at the midclavicular line and extends laterally upward to the fifth rib in the midaxillary line, ending at the posterior chest at the spinous process of T3. The right lower lobe is below the right oblique fissure; the right upper and middle lobes are superior to the right oblique fissure. The left lower lobe is below the left oblique fissure; the left upper lobe is superior to the left oblique fissure. The horizontal fissure is present only on the right and divides the right upper lobe from the right middle lobe. It extends from the fourth rib at the sternal border to the fifth rib at the midaxillary line.
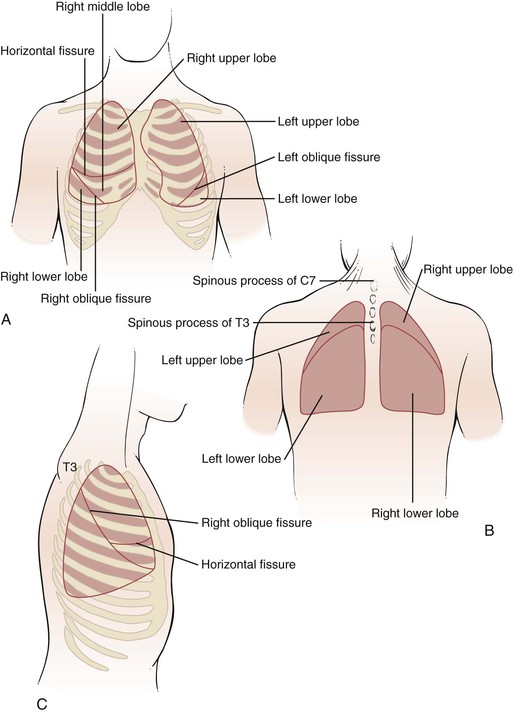
Figure 10–5 Surface topography and the underlying interlobar fissures. A, Anterior view. B, Posterior view. C, Lateral view.
The lungs extend superiorly approximately 3 to 4 cm above the medial end of the clavicles. The inferior margins of the lungs extend to the sixth rib at the midclavicular line, to the eighth rib at the midaxillary line, and between T9 and T12 posteriorly. This variation is related to respiration. The bifurcation of the trachea, the carina, is located behind the angle of Louis at approximately the level of T4 on the posterior chest. The right hemidiaphragm at the end of expiration is located at the level of the fifth rib anteriorly and T9 posteriorly. The presence of the liver on the right side makes the right hemidiaphragm slightly higher than the left.
During quiet breathing, muscle contraction occurs only during inspiration. Expiration is passive, resulting from the elastic recoil of the lungs and chest.
Review of Specific Symptoms
The main symptoms of pulmonary disease are the following:
• Cough
• Hemoptysis (coughing up blood)
• Dyspnea (shortness of breath)
• Wheezing
• Cyanosis (bluish discoloration of the skin)
• Snoring
Cough
The most common symptom of lung disease is the cough. Coughing is so common that it is frequently regarded as a trivial complaint. The cough reflex is a normal defense mechanism of the lungs that protects them from foreign bodies and excessive secretions. Infections of the upper respiratory tract are associated with coughing that usually improves in 2 to 3 weeks. A persistent cough necessitates further investigation.
Coughing is a coordinated, forced expiration, interrupted by repeated closure of the glottis. The expiratory muscles contract against the partially closed glottis, creating high pressure within the lungs. When the glottis suddenly opens, there is an explosive rush of air that clears the air passages. When a patient complains of coughing, ask these questions:
“Can you describe your cough?”
“How long have you had a cough?”
“Was there a sudden onset of coughing?”
“Do you smoke?” If so, “What do you smoke? How much, and for how long?”
“Does the cough occur for prolonged periods?”
“Does the cough occur after eating?”
“Is the coughing worse in any position?”
“Do you have any birds as pets? Do you feed pigeons?”
Coughing may be voluntary or involuntary, productive or nonproductive. In a productive cough, mucus or other materials are expelled. A dry cough does not produce any secretions.
Smoking is probably the most common cause of the chronic cough. Smoker‘s cough results from inhalation of irritants in tobacco and is most marked in the morning. Coughing is normally decreased during sleep. When the smoker awakens, productive coughing tends to clear the respiratory passages. In patients who stop smoking, the cough decreases and may disappear.
Coughing may also be psychogenic. This nonproductive cough occurs in individuals with emotional stress. When attention is drawn to it, the cough occurs more often. During sleep, or when the patient is distracted, the coughing stops. Psychogenic coughing is a diagnosis of exclusion: Only after all other causes have been eliminated can this diagnosis be made.
There are many terms used by patients and physicians to describe a cough. Table 10-1 provides a list of some of the more common descriptors and their possible causes.
Table 10–1
Descriptors of Coughing
| Description | Possible Causes |
| Dry, hacking | Viral infections, interstitial lung disease, tumor, allergies, anxiety |
| Chronic, productive | Bronchiectasis, chronic bronchitis, abscess, bacterial pneumonia, tuberculosis |
| Wheezing | Bronchospasm, asthma, allergies, congestive heart failure |
| Barking | Epiglottal disease (e.g., croup) |
| Stridor | Tracheal obstruction |
| Morning | Smoking |
| Nocturnal | Postnasal drip, congestive heart failure |
| Associated with eating or drinking | Neuromuscular disease of the upper esophagus |
| Inadequate | Debility, weakness |
Sputum Production
Sputum is the substance expelled by coughing. Approximately 75 to 100 mL of sputum is secreted daily by the bronchi. By ciliary action, it is brought up to the throat and then swallowed unconsciously with the saliva. An increase in the quantity of sputum production is the earliest manifestation of bronchitis. Sputum may contain cellular debris, mucus, blood, pus, or microorganisms.
Sputum should be described according to color, consistency, quantity, the number of times it is brought up during the day and night, and the presence or absence of blood. An adequate description may indicate a cause of the disease process. Uninfected sputum is odorless, transparent, and whitish-gray, resembling mucus; it is termed mucoid. Infected sputum contains pus and is termed purulent; the sputum may be yellow, greenish, or red. Table 10-2 lists the appearances of sputum and their possible causes.
Table 10–2
Appearances of Sputum
| Appearance | Possible Causes |
| Mucoid | Asthma, tumors, tuberculosis, emphysema, pneumonia |
| Mucopurulent | Asthma, tumors, tuberculosis, emphysema, pneumonia |
| Yellow-green, purulent | Bronchiectasis, chronic bronchitis |
| Rust-colored, purulent | Pneumococcal pneumonia |
| Red currant jelly | Klebsiella pneumoniae infection |
| Foul odor | Lung abscess |
| Pink, blood-tinged | Streptococcal or staphylococcal pneumonia |
| Gravel | Broncholithiasis |
| Pink, frothy | Pulmonary edema |
| Profuse, colorless (also known as bronchorrhea) | Alveolar cell carcinoma |
| Bloody | Pulmonary emboli, bronchiectasis, abscess, tuberculosis, tumor, cardiac causes, bleeding disorders |
Hemoptysis
Hemoptysis is the coughing up of blood. Few symptoms produce as much alarm in patients as does hemoptysis. Careful description of the hemoptysis is crucial because what is produced can include clots of blood, as well as blood-tinged sputum. The implications of each are very different. Coughing up clots of blood is a symptom of extreme importance because it often heralds a serious illness. Clots of blood are usually indicative of a cavitary lung lesion, a tumor of the lung, certain cardiac diseases, or pulmonary embolism. Blood-tinged sputum is usually associated with smoking or minor infections, but it can be seen with tumors and more serious diseases as well. When a patient complains of coughing up blood, the examiner should ask the following questions:
“Do you smoke?” If yes, “What do you smoke? How much, and for how long?”
“Did the coughing up of blood occur suddenly?”
“Have there been recurrent episodes of coughing up blood?”
“Is the sputum blood-tinged, or are there actual clots of blood?”
“How long have you noticed the blood?”
“What seems to bring on the coughing up of blood? Vomiting? Coughing? Nausea?”
“Have you ever had tuberculosis?”
“Is there a family history of coughing up blood?”
“Have you had recent surgery?”
“Do you take any ‘blood thinners’?”
“Are you aware of any bleeding tendency?”
“Have you had any recent travel on airplanes?”
“Have you felt any unusual sensation in your chest after coughing up blood?” If so, “Where?”
(For a woman with hemoptysis) “Do you use oral contraceptives?”
Any suppurative (associated with the production of pus) process of the airways or lungs can produce hemoptysis. Bronchitis is probably the most common cause of hemoptysis. Bronchiectasis and bronchogenic carcinoma are also major causes. Hemoptysis results from mucosal invasion, tumor necrosis, and pneumonia distal to bronchial obstruction by tumor. Pneumococcal pneumonia characteristically produces rust-colored sputum. Pink and frothy sputum can result from pulmonary edema.
On occasion, patients have a warm sensation in the chest at the location from which the hemoptysis originated. Therefore it is useful to ask patients with recent hemoptysis whether they experienced such a sensation. This information may lead to a more careful review of the physical examination and x-ray films of that area.
Patients who have undergone recent surgery or have traveled for long periods on airplanes are at risk for deep vein thrombophlebitis with pulmonary embolism. Women taking oral contraceptives are likewise at risk for pulmonary embolic disease. Hemoptysis occurs when pulmonary emboli result in infarction, with necrosis of the pulmonary parenchyma.
Recurrent episodes of hemoptysis may result from bronchiectasis, tuberculosis, or mitral stenosis. Atrial fibrillation is a common cause of “irregular heartbeats” and embolic phenomena.
Sometimes it is difficult to ascertain whether the patient coughed up or vomited blood. Most patients can provide a sufficiently clear history. Table 10-3 lists characteristics that help distinguish hemoptysis from hematemesis (vomiting of blood).
Table 10–3
Characteristics Distinguishing Hemoptysis from Hematemesis
| Features | Hemoptysis | Hematemesis |
| Prodrome | Coughing | Nausea and vomiting |
| Past history | Possible history of cardiopulmonary disease | Possible history of gastrointestinal disease |
| Appearance | Frothy | Not frothy |
| Color | Bright red | Dark red, brown, or “coffee grounds” |
| Manifestation | Mixed with pus | Mixed with food |
| Associated symptoms | Dyspnea | Nausea |
Dyspnea
The subjective sensation of “shortness of breath” is dyspnea. Dyspnea is an important manifestation of cardiopulmonary disease, although it is found in other states such as neurologic, metabolic, and psychologic conditions. It is important to differentiate dyspnea from the objective finding of tachypnea, or rapid breathing. A patient may be observed to be breathing rapidly while stating that he or she is not short of breath. The converse is also true: a patient may be breathing slowly but have dyspnea. Never assume that a patient with a rapid respiratory rate is dyspneic.
It is important for the examiner to inquire when dyspnea occurs and in which position. Paroxysmal nocturnal dyspnea is the sudden onset of shortness of breath occurring at night during sleep. Patients are suddenly seized with an intense strangling sensation. They frantically sit up and, classically, run to the window for “air.” As soon as they assume an upright position, the dyspnea usually improves. Orthopnea is difficulty breathing while lying flat. Patients require two or more pillows to breathe comfortably. Platypnea is a rare symptom of difficulty breathing while sitting up and is relieved by a recumbent position. Trepopnea is a condition in which patients are more comfortable breathing while lying on one side. (Some of the more common causes of positional dyspnea are listed in Table 10-4.) For any patient complaining of dyspnea, ask the following questions:
“How long have you had shortness of breath?”
“Did the shortness of breath occur suddenly?”
“Is the shortness of breath constant?”
“Does the shortness of breath occur with exertion? At rest? Lying flat? Sitting up?”
“What makes the shortness of breath worse? What relieves it?”
“How many level blocks can you walk without becoming short of breath?”
“How many level blocks could you walk 6 months ago?”
“Do you smoke?” If so, “How much? For how long?”
“Have you had any exposure to asbestos? Sandblasting? Pigeon breeding?”
“Have you had any exposure to individuals with tuberculosis?”
“Have you ever lived near the San Joaquin Valley? Midwestern or southeastern United States?”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree