Chapter 13
The Breast1
The shape of the breast is like a gourd. They are round for holding blood to be changed into milk. … They have teats, that the new born child may suck therefrom.
Mondino De’ Luzzi (1275–1326)
General Considerations
In the United States, the National Cancer Institute estimates that one of every eight women (approximately 12.5%) will develop breast cancer during her lifetime. Among the malignant diseases in women, breast cancer is the most common to develop and is the second most common cancer cause of death, after cancer of the lung and bronchus. In 2011, it accounted for 230,480 new cancer cases in American women (30% of all new cancer cases), and 15% of all cancer deaths. There were 39,970 deaths from breast cancer: 39,520 in women, 450 in men. Breast carcinoma in situ, a very early form of the disease, was diagnosed in another 57,650 women.
The incidence of cancer of the breast is higher in the United States than in European or Asian countries. It has been well established that women in underdeveloped nations have lower rates of breast cancer than do women from more affluent societies. Among racial and ethnic groups, white and African-American women have the highest incidence rates of breast cancer (113.2 and 99.3 per 100,000 population, respectively). Asian and Pacific Islander women and Latino women have a lower risk (72.6 and 69.4 per 100,000 population, respectively). The incidence rate for female breast cancer began to decline in 2000. The dramatic decline of almost 7% from 2002 to 2003 has been attributed to reductions in the use of hormone replacement therapy following the publication of results from the Woman’s Health Initiative in 2002 indicating that combined estrogen and progesterone therapy was associated with an increased risk of breast cancer and coronary artery disease. Since 2003, breast cancer incidence rates have been stable.
Once breast cancer has occurred in a family, the risk that other women in the same family will have breast cancer is significantly higher. First-degree relatives, such as sisters or daughters, have more than twice the risk for development of breast cancer if the original patient developed cancer in one breast after menopause. Women with a family history of premenopausal breast cancer in one breast have three times the risk. If the original patient had postmenopausal cancer in both breasts, the first-degree relatives have more than four times the risk. First-degree relatives of patients with cancer in both breasts before menopause have nearly nine times the risk.
Most breast cancers are detected as painless masses, noticed by either the patient or the examiner during a routine physical examination. The earlier the diagnosis is made, the better the prognosis is. Screening for breast cancer is best accomplished by a thorough clinical breast examination, breast self-examination (BSE), and mammography. Mammography is the most sensitive method for the detection of breast cancer and has been demonstrated to reduce the breast cancer mortality rate.
Structure and Physiology
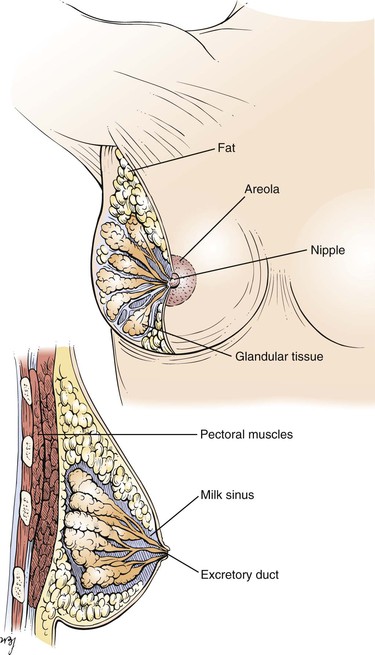
The mammary glands are the distinguishing feature of all mammals. Human breasts are conical in form and are often unequal in size. The breast extends from the level of the second or third rib to the level of the sixth or seventh rib, from the sternal edge to the anterior axillary line. The “tail” of the breast extends into the axilla and tends to be thicker than the other breast areas. This upper outer quadrant contains the greatest bulk of mammary tissue and is frequently the site of neoplasia. Figure 13-1 illustrates the normal breast.
Both the nipple and areola contain smooth muscle that serves to contract the areola and compress the nipple. Contraction of the smooth muscle makes the nipple erect and firm, thereby facilitating the emptying of the milk sinuses.
The skin of the nipple is deeply pigmented and hairless. The dermal papillae contain many sebaceous glands, which are grouped near the openings of the milk sinuses. The skin of the areola is also deeply pigmented but, unlike the skin of the nipple, contains occasional hair follicles. Its sebaceous glands are commonly seen as small nodules on the areolar surface and are termed Montgomery‘s tubercles.
Cooper‘s ligaments are projections of the breast tissue that fuse with the outer layers of the superficial fascia and serve as suspensory structures.
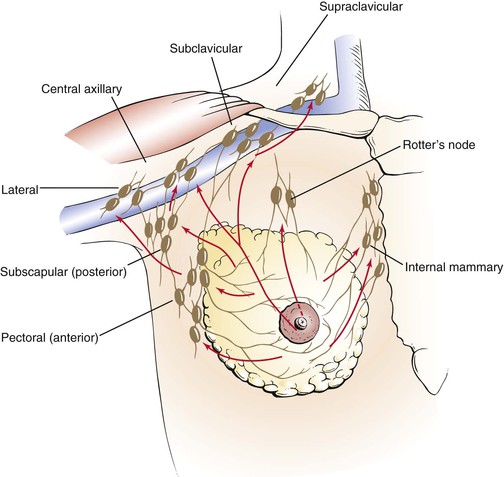
The blood supply to the breast is carried by the internal mammary artery. The breast has an extensive network of venous and lymphatic drainage. Most of the lymphatic drainage empties into the nodes in the axilla. Other nodes lie beneath the lateral margin of the pectoralis major muscle, along the medial side of the axilla, and in the subclavicular region. The main lymph node chains and lymphatic drainage of the breast are illustrated in Figure 13-2.
Several physiologic changes occur in the breast. These changes are a result of the following factors:
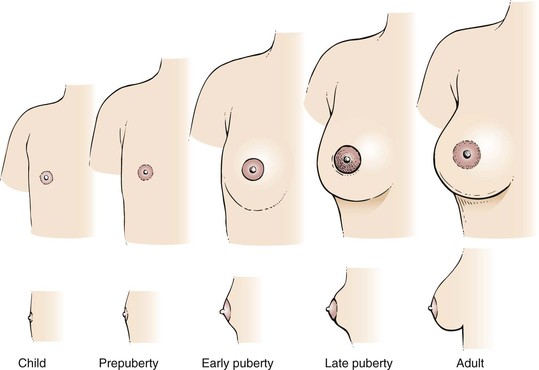
At birth, the breasts contain a branching system of ducts emptying into a developed nipple. There is elevation of only the nipple at this stage. Shortly after birth, there is a slight secretion of milky material. After 5 to 7 days, this secretory activity stops. Before puberty, there is elevation of the breast and nipple, called the breast bud stage. The areola has increased in size. At the onset of puberty, the areola enlarges further and darkens. A distinct mass of glandular tissue begins to develop beneath the areola. By the onset of menstruation, the breasts are well developed, and there is forward projection of the areola and nipple at the apex of the breast. When the breast has reached maturity 1 to 2 years later, only the nipple projects forward; the areola has receded to the general contour of the breast. The stages of breast development from birth to adulthood are illustrated in Figure 13-3. Figure 21-47 further illustrates and describes the breast developmental stages.
The nodularity, density, and fullness of the adult breast depend on several factors. Most important is the presence of excess adipose tissue. Because the mammary gland consists mainly of adipose tissue, women who are overweight have larger breasts. Pregnancy and nursing also alter the character of the breasts. Often, women who have nursed have softer, less nodular breasts. However, because the glandular tissue is approximately equal in all women, the size of the breast is unrelated to nursing. With menopause, the breasts decrease in size and become less dense. There is an associated decrease in elastic tissue as women age.
The major physiologic change related to the menstrual cycle is engorgement, occurring 3 to 5 days before menstruation. This is an increase in the size, density, and nodularity of the breasts. There is also an increased sensitivity of the breasts at this time. Because the nodularity of the breasts increases, the examiner should not attempt to diagnose a breast mass at this time. The patient should be reevaluated during the midperiod of the next cycle.
With pregnancy, the breasts become fuller and firmer. The areolae darken, and the nipples become erect as they enlarge. As the woman approaches the third trimester, a thin, yellowish secretion, called colostrum, may be noted. After the birth of the child, if the mother begins nursing within 24 hours, the secretion of colostrum stops, and the secretion of milk begins. During nursing, the breasts become markedly engorged. After the woman has stopped nursing, lactation continues for a short time.
The neuroendocrine control of the breasts can be outlined as follows. Suckling produces nerve impulses that travel to the hypothalamus. The hypothalamus stimulates the anterior pituitary to secrete prolactin, which acts on the glandular tissue of the breast to produce milk. The hypothalamus also stimulates the posterior pituitary to produce oxytocin, which stimulates the muscle cells surrounding the glandular tissue to contract and force the milk into the ductular system.
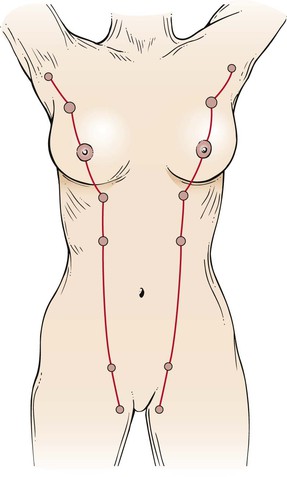
Many abnormalities of the breast are related to its embryologic characteristics. An epithelial ridge, called the milk line, forms along each side of the body from the axilla to the inguinal region. Along this milk line are multiple rudiments for future breast development. In humans, only one rudimentary pair in the pectoral region persists and eventually develops into normal breasts. Accessory breasts or nipples are present in as many as 2% of white women. Accessory breasts may exist as glandular tissue, nipple, or only the areola. The axilla is the most common site for these anomalous structures, followed by a site just below the normal breast. In more than 50% of all patients with accessory breast tissue, the anomalies are bilateral. In general, accessory breast tissue is of little clinical significance. It usually has no physiologic function and is rarely associated with disease. Figure 13-4 illustrates the milk line. Figure 13-5 shows an accessory nipple.
Review of Specific Symptoms
The most important symptoms of breast disease are the following:
Mass or Swelling
During self-examination, a patient may discover a breast mass. Ask the following questions:
“When did you first notice the lump?”
“Have you noticed that the mass changes in size during your menstrual periods?”
“Have you ever noticed a mass in your breast before?”
“Have you noticed any skin changes on the breast?”
“Have you had any recent injury to the breast?”
“Is there any nipple discharge? Nipple retraction?”
“Do you have breast implants?” If yes, “What are they made of?”
If the lump enlarges during the premenstrual and menstrual stages of the cycle, it is likely that the woman is detecting only physiologic nodularity. The association of nipple discharge, nipple inversion, or skin changes overlying the mass is strongly suggestive of neoplasm. Figure 13-6 shows a large breast mass found on self-examination.
Pain
Breast pain or tenderness is a common symptom. Most often, these symptoms are attributable to the normal physiologic cycle. Ask the following questions of any patient with breast pain:
“When did you first experience the pain?”
“Are there any changes in the pain with your menstrual cycle?”
“Do you have pain in both breasts?”
“Have you had any injury to the breast?”
“Is the pain associated with a mass in the breast? Nipple discharge? Nipple retraction?”
Rapidly enlarging cysts may be painful. Cystic disease of the breasts is usually painless. Although breast pain is a relatively uncommon manifestation of breast cancer, its presence does not exclude the diagnosis. Never delay evaluation of a painful breast mass.
Nipple Discharge
Nipple discharge is not a common symptom, but it should always raise the suspicion of breast disease, especially if the discharge occurs spontaneously. Any patient who describes a nipple discharge should be asked the following questions:
“What is the color of the discharge?”
“Do you have a discharge from both breasts?”
“When did you first notice the discharge?”
“Is the discharge related to your menstrual cycle?”
“When was your last menstrual cycle?”
“Is the discharge associated with nipple retraction? A breast mass? Breast tenderness?”
“Are you taking any medications?”
If the woman has recently delivered a child, ask
The most common types of discharge are serous and bloody. A serous discharge is thin and watery and may appear as a yellowish stain on the patient’s garments. This commonly results from an intraductal papilloma in one of the large subareolar ducts. Women taking oral contraceptives may complain of bilateral serous discharge. A serous discharge can also occur in women with breast carcinoma.
A bloody discharge is associated with an intraductal papilloma, which is common among pregnant and menstruating women. It may, however, be associated with a malignant intraductal papillary carcinoma. The presence of any nipple discharge is more important than its character because both types of discharge are associated with benign or malignant disease.
A milky discharge is usually milk. The secretion of milk while not nursing is known as galactorrhea. It is common for women to continue to secrete milk for a few months after they stop nursing. In rare instances, the secretion may continue for a year. Abnormal lactation may also result from a pituitary tumor that interferes with the normal hypothalamic-pituitary feedback loop or from the use of certain tranquilizing medications. Mechanical stimulation or suckling may produce physiologic stimulation.
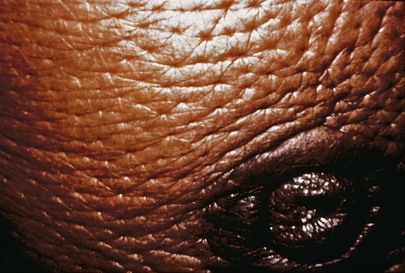
Change in Skin over Breast
A change in the color or texture of the skin of the breast or areola is an important symptom of breast carcinoma. The presence of dimpling, puckering, or scaliness warrants further investigation. The presence of unusually prominent pores, indicative of edema of the skin, is an important sign of malignancy. This clinical sign is called peau d’orange because of its orange-peel appearance. During the early stages of breast carcinoma, the lymphatic vessels of the breast are dilated and contain occasional emboli of carcinoma cells. Limited peau d’orange over the lower half of the areola is present. As the disease progresses, more lymphatic vessels become filled with carcinoma cells that block them, creating more generalized edema. The classic appearance of peau d’orange is pictured in Figure 13-7.
General Suggestions
The interviewer should pay special attention to the family history of any woman presenting with symptoms of breast disease. As indicated earlier, breast cancer may be a familial disorder. The occurrence of breast disease in a close relative and the age at which it developed are relevant to the patient’s disease. Ask the patient the following questions:
“Have you had a mammogram?” If yes, “When and what was the result?”
“Have you had breast cancer without the removal of your breast?”
“Do you have breast implants?”
“Have you had any breast biopsies or breast surgery?”
“Have you ever had radiation treatments to your breasts?”
“Do you use birth control pills?”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree