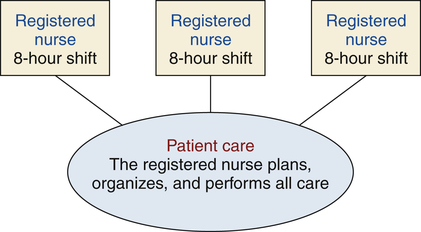
Barbara Cherry, DNSc, MBA, RN, NEA-BC After studying this chapter, the reader will be able to: 1. Outline key issues surrounding staffing for a health care organization. 2. Evaluate lines of responsibility and accountability associated with various types of nursing care delivery models. 3. Analyze the advantages and disadvantages of nursing care delivery models in relation to patient care in various settings. 4. Integrate essential components of the critical pathway model into patient care planning. 5. Differentiate among several nursing care delivery models by evaluating their defining characteristics. 6. Explain the purpose and components of nursing case management. 7. Summarize criteria to be considered in developing future models of nursing care delivery. Clinical management plans that specify the optimal timing and sequencing of major patient care activities and interventions by the interprofessional team for a particular diagnosis, procedure, or health condition and are designed to standardize care delivery (Coffey et al, 2005); clinical pathways may also be called critical paths, practice protocols, or care maps; clinical pathways support the implementation of clinical practice guidelines. Recommendations for appropriate treatment and care for specific clinical circumstances; guidelines are developed though a systematic process to integrate the best evidence for treating specific medical conditions and assist health care providers to make decisions about appropriate treatment (Institute of Medicine [IOM], 1990). Also called care delivery system or patient care delivery model; details the way work assignments, responsibility, and authority are structured to accomplish patient care; depicts which health care worker is going to perform what tasks, who is responsible, and who has the authority to make decisions. Indication of the amount and complexity of care required for any particular patient; high acuity indicates a need for more intense, complex nursing care as compared with lower acuity, which indicates a need for moderate, less complex nursing care. Patient classification system: Method used to group or categorize patients according to specific criteria and care requirements and thus help quantify the patient acuity, or amount and level of nursing care needed. Combination of categories of workers employed to provide patient care (e.g., RNs, LPNs, or licensed vocational nurses [LVNs], or unlicensed assistive personnel [UAP]). Ensuring that an adequate number and mix of health care team members (e.g., RNs, LPNs or LVNs, UAP, clerical support) are available to provide safe, quality patient care; usually a primary responsibility of the nurse manager. Unlicensed assistive personnel (UAP): An unlicensed individual who is trained to function in an assistive role to the RN by performing patient care activities as delegated by the nurse; may include nursing assistants, clinical assistants, orderlies, health aides, or other titles designated within the work setting. Additional resources are available online at: http://evolve.elsevier.com/Cherry/ Vignette Questions to Consider While Reading This Chapter 1. Why is the RN’s work assignment different in different units—obstetrics, critical care, medical-surgical, and the outpatient clinic? 2. Who decides how many nurses and other personnel are needed to staff a clinical site? 3. How do nurse managers on nursing units decide how assignments will be made? 4. Who has responsibility and authority for making patient care assignments? • How does staffing affect patient care, staff satisfaction, and the organization’s financial status? • What staff mix (e.g., combination of RNs, LVNs or LPNs, UAP, clerical support) is required to provide quality patient care? • Who is responsible for making work assignments? • What factors should be considered when making patient care and other work assignments? Is the work assigned by task or by patient? Staffing can be defined as the activities required to ensure that an adequate number and mix of health care team members (e.g., RNs, LVNs or LPNs, UAP, clerical support) are available to meet patient needs and provide safe, quality care. Important research is validating the contribution and value of RNs to improving patient outcomes, reducing complications and length of hospital stay, and preventing premature mortality (Blegen et al, 2011; Dall et al, 2009; Needleman et al, 2011). The Institute of Medicine’s report titled Keeping Patients Safe: Transforming the Work Environment of Nurses (2004) is an extensive analysis of nurses’ work environments and staffing issues; this report strongly affirms nurses’ essential roles in achieving quality patient care and safety. In order for nurses to have the greatest opportunity to achieve safe, quality care, staffing systems must address individual and aggregate patient care needs and the clinical competencies of nurses to provide care to specified patient populations; staffing systems must also reflect the value of RNs as vitally important to the organization and provide nurses time to exercise professional judgment, and acknowledge that patient needs can change from moment to moment (ANA, 2012). While appreciating the overall value of the RN in providing patient care, several specific considerations regarding staffing are reviewed related to (1) patient needs, (2) staff satisfaction, and (3) organizational needs. The primary considerations for staffing a specific nursing unit are the number of patients; the level of intensity of care required by those patients (commonly referred to as patient acuity); contextual issues, such as architecture, geography of the environment, and available technology; level of preparation and experience of the staff members providing the care; and the quality of the nurses’ work life (ANA, 2005). Knowing only the number of patients that require care is an ineffective way to plan staffing because of the wide range of care requirements needed by individual patients. To account for the diverse care needs and quantify the intensity of care required by a group of patients, nurse managers responsible for staffing use various patient classification systems. Because of this complexity and the differences in patient populations across different health care facilities, patient classification systems vary from organization to organization. However, the ANA (2005) has recommended that the following physical and psychosocial factors be considered when determining the intensity of care required for any group of patients: • Cultural and linguistic diversities • Severity and urgency of the admitting condition • Ability to meet health care requisites • Availability of social supports • Other specific needs identified by the patient and by the RN Nurses who are satisfied with their work generally provide higher-quality, more cost-effective care. Staffing systems should address the quality of work life for the nursing staff as equally important as the quality of patient outcomes (ANA, 2005). Attention to staff schedules is a major responsibility for the nurse manager, especially in light of the 24-hour/day, 365-day/year staffing needs in many health care facilities. Creative staffing options are available to meet the varied needs of staff members, including the following: • 10-hour shifts/4 days per week • 12-hour shifts/3 days per week • Combination of 8-hour and 12-hour shifts • Premium pay or part-time staff for weekend work Each of these options has various advantages and disadvantages. For example, long shifts over consecutive days may result in clinical errors when nurses become fatigued (Barker and Nussbaum, 2011; IOM, 2004). Self-scheduling is a popular staffing technique in which the responsibility for staffing the unit is delegated to the employees on the unit who work collectively to design the schedule based on preestablished staffing criteria and some guidance from the manager. No one scheduling system has proven to be best overall for staff satisfaction. However, staffing methods that gain staff input and enhance staff autonomy seem to be a major key to staff satisfaction (Wieck et al, 2009). Productivity, the ratio of the amount of outputs produced (i.e., home visits) to the specific amount of input (nursing hours worked), is the measure of staffing efficiency. Because staff salaries are by far the largest expense for any health care organization, productivity—or the efficient use of staff—has a direct effect on the organization’s bottom line. Fortunately, even though RNs represent the highest-paid staff in a facility, research has yet again demonstrated the value of RNs in improving patient outcomes and increasing hospital profitability (Anderson et al, 2011; Dall et al, 2009; McCue et al, 2003). However, it is important to remember that most health care organizations continue to function under tight financial constraints, making efficient management of staff essential to ensure the organization’s financial solvency. The nurse manager is accountable for appropriately managing staffing to stay within budgetary guidelines for the following: Perhaps most critical to an organization’s success in a competitive health care environment is customer (patient) satisfaction. The key to customer satisfaction is the patient’s personal interaction with the organization’s employees. According to Kenagy and associates (1999), “Interactions with patients and their families have remarkably strong effects on clinical outcomes, functional status and even physiologic measures of health” (p. 663). Appropriate staffing within budget constraints with well-trained, competent, professional staff members who are committed to providing safe, high-quality care is the number-one challenge for health care facilities. This section has provided the reader with a brief introduction to staffing issues, such as scheduling options, patient classification systems, productivity and staff mix, and the RN’s contribution to improved patient outcomes. These issues related to staffing in a health care organization are much more complex than may appear from this introduction. The reader, especially the person interested in entering nursing management, is encouraged to learn more about staffing and these related issues. Box 20-1 lists online learning resources related to staffing. The oldest method of organizing patient care is total patient care, sometimes referred to as case nursing. In total patient care, nurses are responsible for planning, organizing, and performing all care, including personal hygiene, medications, treatments, emotional support, and education required for their assigned group of patients during the assigned shift. A diagram of the total patient care model is shown in Figure 20-1.
Staffing and Nursing Care Delivery Models
Chapter Overview
Staffing
Staffing and Patient Needs
Patient Classification Systems
Staffing and Staff Satisfaction
Staffing and Organizational Needs
Financial Resources
Customer Satisfaction
Nursing Care Delivery Models
Total Patient Care
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Staffing and Nursing Care Delivery Models
Get Clinical Tree app for offline access