Temporary Fecal Diversions
Prevention and Management of Constipation
Prevention and Management of Diarrhea
A fecal and/or urinary diversion presents many concerns for the individual who is adapting and trying to return to their previous life style. The Wound Ostomy Continence (WOC) nurse needs to address many issues related to the type of ostomy the person has as well as whether the diversion is temporary or permanent. This chapter discusses areas related to both fecal and urinary diversions to enable the WOC nurse to provide information to help the person to return to his or her former lifestyle. There are many options and interventions to help to manage his or her concerns, and these are addressed in this chapter.
Temporary Fecal Diversions
Not all fecal diversions are permanent, and this will depend on the patients’ diagnosis and prognosis. Types of temporary fecal stomas are end/Hartmann’s pouch and loop ileostomy or colostomy. Temporary stomas are created to divert the stool from the distal bowel, allowing the bowel to heal. The surgeon can reverse the stoma within 3 to 6 months with minimal loss of intestinal function (McGrath & Porrett, 2005). There are many conditions that can require a temporary diversion (Box 12-1).
Box 12-1 Conditions Requiring Temporary Fecal Stoma
Emergency condition for distal bowel obstruction or distal trauma
To rest distal segment of the bowel that may have a disease process, fistula, or Crohn’s disease
To protect an anastomosis
In the Hartmann’s procedure, a resection of the diseased bowel is performed, the rectal stump is closed, and an end colostomy is created. This procedure is usually performed for emergency conditions, that is, perforated diverticular disease. The patient will be taught that he or she may experience passing stool or mucus from the anus. This may be a temporary or permanent stoma depending on the indication for the surgery and the patient’s condition.
With the loop stoma, a loop of the bowel is brought through the abdominal wall (Figure 7-4 in Chapter 7). An opening is made in the bowel to allow stool to be expelled. A temporary rod or bridge is placed below the loop to prevent retraction of the stoma. Loop ileostomies are more common than are loop colostomies. Reversal surgery for loop ileostomy are easier as a small incision is made around the loop, and the two ends are brought through the incision and reconnected (Cera, 2008).
Although not commonly created, a mucous fistula can be created during emergency surgery at the same time as the ileostomy or colostomy. The proximal end of the remaining colon or rectum is brought out onto the abdomen as a mucous fistula, called a mucous fistula because some mucus will pass from this opening. The purpose of the mucous fistula is to reduce the risk of stump dehiscence, which can occur with active rectal disease and preoperative steroid use (Windsor & Conn, 2008). The patient will be taught to cover the mucous fistula with a stoma cap (Fig. 12-1) or a mini drainable pouch or in some cases a gauze pad changed, based on the amount of mucous drainage.

FIGURE 12-1. Stoma cap.
Colostomy
Irrigation
The person with a sigmoid colostomy has the option of managing his or her colostomy with irrigation, and this should be offered as a management method to a person with a left-sided colostomy (Fig. 12-2). Managing a colostomy by irrigation is for many people a simple, cost-effective procedure. Carlsson et al. (2010) studied the positive and negative aspects of colostomy irrigation (CI) and found that negative aspects reported were time required for CI, less flexibility to plan CI, and more flatulence. Positive aspects reported were feeling secure, having an empty pouch, sense of freedom, and fewer pouch changes.
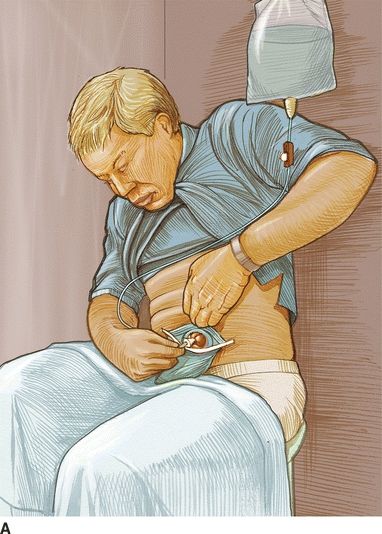
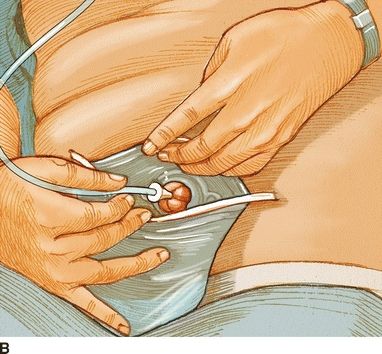
FIGURE 12-2. Colostomy irrigation. From Nursing 2006, 36(4), 22.
CI can be performed daily or every other day with the goal of being “stool free,” that is, no stool passing from the stoma between irrigation. Once the colostomy is regulated, the person no longer has to wear a pouching system and can wear a stoma cap. These are available as a one- or two-piece system; some people prefer the two-piece system to use with the irrigation sleeve. Stoma caps are available also as cut-to-fit skin barrier with filter to manage gas and absorb mucous discharge.
Patient Selection
Irrigation is not always suitable for all patients with a colostomy. The WOC nurse should evaluate the person’s understanding of the irrigation procedure as well as the person’s motivation, manual dexterity and eyesight, and the current function of his or her colostomy. Good candidates for a successful outcome with irrigation have one or two semi-formed or formed stools in 24 hours. Irrigation is recommended only for descending or sigmoid colostomy as this section of the colon has less peristalsis and can hold stool for several days; there is less frequent output, and the stool is formed unlike the right-sided colostomies.
The WOC nurse should explain to the patient that CI is an option to manage the ostomy. It is not always recommended early postoperatively. If a patient will undergo chemotherapy or has a healing perineal incision, the irrigation procedure can be delayed. The patient should be assured that he or she can always stop the irrigation procedure at any time and resume using a pouching system. See Box 12-2 for contraindications to CI. Complications associated with irrigation include nonreturn of fluid, vasovagal response, and abdominal cramps.
Box 12-2 Contraindications to Colostomy Irrigation
Current chemotherapy/radiotherapy
Stoma stenosis
Large parastomal hernia or stoma prolapse
Crohn’s disease
Poor prognosis
Diarrhea
During the learning stage of CI, the person will need encouragement and support while he or she becomes proficient in the procedure. Box 12-3 explains the CI procedure.
CLINICAL PEARL
Colostomy irrigations should be discontinued if a person develops a peristomal hernia.
Box 12-3 Colostomy Irrigation Procedure
1. Gather the following equipment*:
- Irrigation kit: 2-L bag, tubing with flow regulator, soft cone
- Water-soluble lubricant
- Irrigation drain sleeve
- Ostomy belt
- Warm water
- Coat hanger or wall hook to hang the irrigation bag from
2. Attach irrigation cone to tubing and fill the bag with 1,000 mL of warm tap water.
3. Hang the irrigation bag from hook at shoulder level when seating on toilet.
4. Open the regulator clamp on the tubing and let the water run through the tube to remove the air. Reclamp the tube.
5. Remove colostomy pouch; if two piece, leave the barrier in place. Place the irrigation sleeve over the stoma or attach to the barrier or secure with an ostomy belt.
6. Lubricate the cone with water-soluble lubricant and gently insert the cone into the stoma until it fits snugly.
7. While holding the cone in place with one hand, open the clamp on the tubing and let 500 to 1,000 mL of water flow slowly into the colon over 5 to 10 minutes. Regulate the flow of water using the clamp. Note start with 500 mL of water.
8. Once the amount of water is instilled, clamp the tube and hold the cone in place for about a minute, and then remove the cone from the stoma.
9. Close the top of the irrigation sleeve, and wait for results to flow into the toilet. Most is expelled in the first 5 to 10 minutes; the rest may take up to 30 to 45 minutes.
10. Once returns are complete, remove the sleeve, clean the skin, and apply the pouching system or stoma cap/mini pouch.
11. Wash the equipment with mild soap and warm water, hang to dry, and store in a clean container.
Adapted from Prinz, A. (2013). Irrigation for the Colostomate-Life without the pouch! Colostomy New Patient Guide. UOAA The Phoenix Magazine; Hayes, D. (2013). Colostomy irrigation: Retraining continence and regaling confidence. Journal of Stomal Therapy Australia, 33(2), 18–20.*Supplies can be obtained from ostomy companies that have irrigation sets.
Odor and Flatus Management
Odor is a common fear for the person with a diversion; pouching systems are odor proof, but this does not always assure the person there is no odor. Teach the person that odor should only occur when emptying and changing the pouching system, and taking time to clean the inside and outside of the pouch tail prevents odor. If using a pouch clip for open-ended pouch, teach to wash and dry the clip after emptying the pouch to eliminate any risk of odor.
Deodorants/eliminators are available in the form of droplets and liquid that can be added to the inside of the clean pouch to help eliminate the odor of stool. The liquid deodorant/eliminator is placed into the newly applied pouch, and as the stool drains into the pouch, the deodorant/eliminator mixes with the stool to decrease odor. When the pouch is emptied, the deodorant/eliminator is replaced. A lubricating deodorant can be used to both deodorize the stool and lubricate the inside of the pouch for easy emptying.
There are orally ingested products available to help deodorize the stool internally before it reaches the pouch. Bismuth subgallate (Devrom) is one option for both odor and flatus, usually recommended to take 200 mg before meals and at bedtime. The patient should be taught that this medication will turn the stool dark. Chlorophyllin 100 mg is another product that is taken orally three times a day. This will turn the stool or urine green and initially can cause loose stools, but this is a temporary side effect. Both of these products can be obtained without a prescription, but the patient should discuss this with his or her health care provider and WOC nurse before trying the product; some feel that the green color can mask blood in the stool, which is an important symptom requiring further investigation.
Other recommendations to help control odor from stool include parsley, buttermilk, cranberry juice, and yogurt. Foods to avoid that can produce odor and gas are listed in Box 12-4.
Box 12-4 Foods That May Cause Gas and Odor
Asparagus
Beans
Beer
Cabbage family
Carbonated drinks
Eggs (hard boiled)
Fish
Melon
Milk products
Onions
Spiced foods
In the large colon, flatus is formed from bacterial activity related to undigested carbohydrates including cellulose in the colon. About 500 mL of flatus may be expelled daily and can increase based on high-carbohydrate foods eaten (Richards, 2005). Proteins and fats cause little gas. In the small intestine, flatus can occur from swallowing air, chewing gum, eating fast, and using loose-fitting dentures. For flatus management, pouches are available with built-in charcoal filter, vents, and self-sealing filters that can be attached to the outside of the pouch. Integrated pouch filters are usually placed at the top of the pouch and, in many cases, may only last 24 to 36 hours when the filter becomes plugged or wet from stool. Vents, an external device, are designed without a filter and have a plug that needs to be manually opened to release built-up gas in the pouch. These are an alternative to relieving gas and will last as long as the pouch is in place.
Room sprays can be used to eliminate odor rather than mask it and are best used prior to emptying the pouch rather than afterward.
Prevention and Management of Constipation
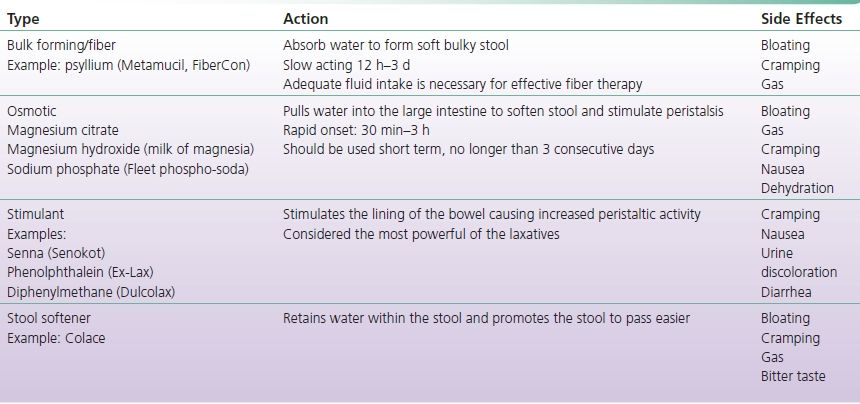
Constipation can occur in the patient with a sigmoid colostomy; a person with an ileostomy rarely will become constipated as there is little storage capacity in the small bowel. Fiber is recommended for the person with a colostomy to increase bulk to the stool and make it easier to pass. The person being managed with opioid pain medication may also suffer from constipation. Mild constipation can be managed by adjusting the diet in the following ways: increase fluids, high-fiber foods, and exercise. It is recommended that fiber be increased in small increments as it may cause bloating, fullness, and gas. Stool softeners should also be recommended when taking pain medications. There are four types of laxative to consider: bulk forming, stimulant, osmotic, and stool softeners (Table 12-1).
TABLE 12-1 Types of Laxatives
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Colostomy
Colostomy Ileostomy
Ileostomy Ileal Conduit
Ileal Conduit Conclusions
Conclusions