Kidney Location and Structure
 Structure and Function of the Lower Urinary Tract
Structure and Function of the Lower Urinary Tract
Adrenal Glands and Adjacent Organs
Urine Concentration and Volume
 Electrolyte Balance and Renin–Angiotensin–Aldosterone System
Electrolyte Balance and Renin–Angiotensin–Aldosterone System
Calcium, Phosphate, and Magnesium Regulation
Renin–Angiotensin–Aldosterone System
A fundamental understanding of the urinary system and the changes in urine filling, storage and elimination associated with urinary reconstruction is essential in providing care for a person with a urinary diversion. This complex system provides homeostasis to maintain a stabilized internal environment for optimal cell and tissue metabolism. This arduous task is accomplished through excretion of water and waste; fluid and electrolyte balance; regulation of acid–base balance, and endocrine function by secreting hormones: erythropoietin (EPO) to promote red blood cell production and renin–angiotensin–aldosterone to regulate blood volume and pressure; and activation of vitamin D to promote ossification of bones and teeth. The urinary system consists of the upper urinary tract, which is responsible for urine formation and transportation (pair of kidneys, renal pelves, and ureters), and lower urinary tract (urinary bladder, urethra, and support structures), which provides urine storage and elimination (Fig. 2-1). This chapter concentrates on the normal structure and function of the urinary system.
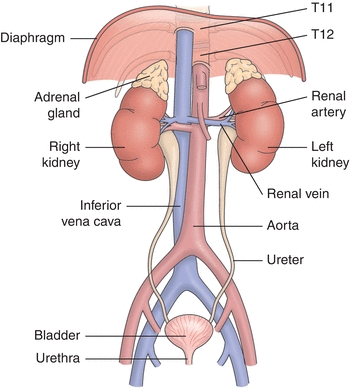
FIGURE 2-1. Kidneys, ureters, and bladder.
Kidney Location and Structure
The kidneys are a pair of reddish brown, bean-shaped organs situated near the twelfth thoracic (T-12) and third lumbar (L-3) vertebrae, lying on either side of the vertebral column. They are located against the deep muscles of the back in the retroperitoneal space. The right kidney is lower than the left to accommodate the liver. The lateral aspect of the kidney is convex, while the medial surface is quite concave. The hilum is located at the resulting medial depression that leads into a hollow chamber called the renal sinus, which contains blood vessels, nerves, lymphatic vessels, and the proximal ureter. The renal pelvis is a funnel-shaped sac, which is the superior end of the expanded ureter that is created by the convergence of two or three tubes called major calyces.
A bisected kidney discloses two distinct regions: an inner medulla and outer cortex, which is often referred as the parenchyma or “meat of the kidney” (Fig. 2-2). The inner medulla is made up of conical masses of tissue called renal pyramids. The base of the pyramids orientate toward the convex surface, whereas their apices form the renal papillae, which arise from the calyces approaching the hilum. The renal papilla is a valvular-like system that promotes outward (antegrade) flow from the nephron (functional unit of the kidney) into the renal pelvis to prevent reflux (retrograde flow) into the renal cortex. The renal cortex is granular in nature and forms a shell around the medulla. It dips into the medulla to fill the space between the pyramids forming renal columns and lobules. The cortex is protected by a dense adherent covering (renal capsule) and embedded in a mass of fat tissue. In addition, a double layer of renal fascia over the perinephric fat and other fibrous tissue helps protect and anchor the kidneys to the posterior abdominal wall. Therefore, the renal capsule, fat cushion, and perirenal and Gerota fascia, as well as the abdominal muscles, diaphragm, quadratus lumborum muscles, and ribs, offer protection and absorb shock if a blow occurs from the abdomen or flank region (Huether, 2011; Shier et al., 2013a).
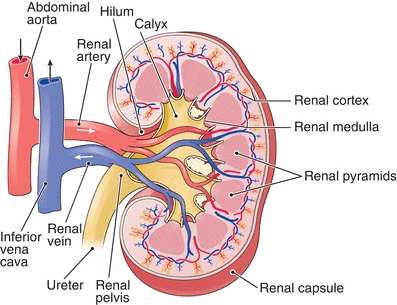
FIGURE 2-2. Structure of the kidney.
The functional unit of the kidney is the nephron (Fig. 2-3). Its primary function is to remove waste and toxic products from the plasma and control the composition of body fluids. There are about 1 million nephrons in each renal parenchyma, so one can envision how tiny and condensed each unit must be. The nephron is a tubelike structure subdivided into the renal corpuscle (glomerulus and Bowman capsule) and a renal tubule. The glomerulus begins as a complex filtering unit composed of a tangled collection of blood capillaries that is surrounded by a thin-walled, cuplike structure called a Bowman capsule. It continues with a proximal convoluted (highly coiled) tubule, loop of Henle, and ends with the distal convoluted tubule, which empties into a collecting duct where multiple distal convoluted tubules merge. The fluid (glomerular filtrate) then drains into the top of the renal pyramid, and then to the renal papillae (prevents retrograde flow) where it joins the minor calyx and major calyx and lastly empties into the renal pelvis.
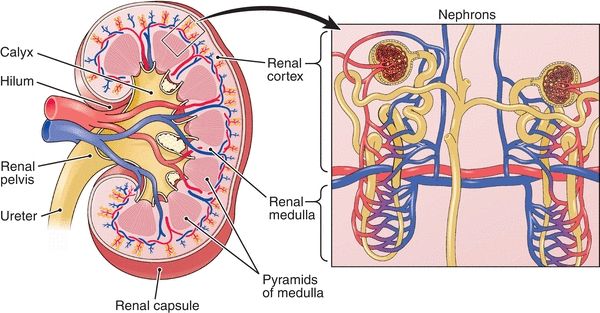
FIGURE 2-3. Kidney (left) with nephron (enlarged to show detail, right).
Blood supply to the nephron enters by an afferent arteriole, which gives rise to the glomerus’s tangled capillaries and exits the glomerus via the efferent arteriole. It continues through the peritubular and vasa recta capillary system near the nephron loop where it joins blood from other peritubular capillary systems and ultimately unites with the kidney’s venous system. The intricate adjacent capillary system of the nephron is crucial for renal filtration and urine formation.
There are two types of nephrons, cortical and juxtamedullary (Huether, 2011; Shier et al., 2013a). The kidney is a highly vascular organ. Although the kidneys account for only 1% of a person’s body weight, it receives over 15% to 30% (1,000 to 1,200 mL/min) of the total cardiac output when a person is at rest (Shier et al., 2013a). Blood is supplied to the kidney from usually a single (pairing can occur) renal artery, which directly branches off from the abdominal aorta. The position of the artery may vary in individuals; therefore, best surgical approach may need to be determined by the urologist prior to reconstruction. As the renal artery enters the hilum, it splits into the interlobar arteries, which pass through the renal pyramids and then branch to form a series of incomplete arches at the junction between the medulla and cortex called arcuate arteries. These arteries in turn branch into cortical radiate arteries, which finally give rise to the afferent arterioles that lead to the functional kidney units called nephrons. Venous return follows the same flow series as does the arterial return.
Elimination of Urine
Urine forms as the result of glomerular filtration of the blood plasma, tubular reabsorption, and minus tubular secretion. Once the glomerular filtrate passes through the collecting ducts, the urine remains unchanged. It exits the collecting ducts, drains into the minor and major renal calyces, and enters the renal pelvis, which is formed from the convergence of two to three major calyces. The renal pelvis is the funnel-shaped portion of the proximal ureter. The urine is transported from the kidney and ureters to a saclike muscle (bladder) in an antegrade fashion (efflux) while avoiding retrograde (reflux) movement of the urine through peristalsis. The bladder serves as a reservoir for urine and exits the body through a tubular structure called the urethra.
Ureters
The ureter is a long, tubular organ with an approximate length of 24 to 30 cm, with the left ureter slightly longer due to the inferior location of the right kidney (Huether, 2011; Schenkman, 2013; Shier et al., 2013a). The superior aspect of the ureter consists of the funnel-shaped renal pelvis, which holds approximately 15 to 20 mL of urine and tapers to 2 mm where it becomes officially the ureter, known as the ureteropelvic junction (UPJ). The UPJ is a common site for congenital or acquired obstruction, i.e., stones. The ureter continues in an inverted “S” shape in a downward and medial fashion until it terminates into the posterior base of the bladder (trigone) called the ureterovesical junction (UVJ).
A variety of sources supply arterial blood to the ureters, and these vary among people. Branches of the renal, gonadal, or adrenal arteries supply the upper ureters, while branches of the obturator artery, deferential artery in men, or uterine artery in women supply the lower (pelvic) ureter region. Venous return parallels the arterial supply as well as lymphatic drainage channels.
CLINICAL PEARL
The ureteropelvic junction (UPJ) obstruction is a common congenital condition.
Ureter Function
The main function of the ureter is to transport urine to the bladder in a fashion that promotes emptying without reflux. Several mechanisms promote antegrade urine flow: peristalsis through mechanical distention; neurologic, endocrine, and pharmacologic stimulation; as well as the UVJ structure. The renal pelvis holds about 15 to 20 mL of urine, and this distension initiates muscular peristaltic waves at a rate consistent with amount of urine present in the renal pelvis. For instance, if urine is formed quickly (i.e., diuretic therapy), then the peristaltic wave may occur every few seconds; in contrast, if glomerular filtration rate is slow (i.e., dehydration), the peristalsis may occur every few minutes (Shier et al., 2013a). In recent research, it appears that interstitial cells of Cajal (ICC) are more likely the modulators of smooth muscle activity involved in ureteral peristalsis (Hurtado et al., 2014; Lang et al., 2007).
Resting intraluminal pressure is elevated with each peristaltic contraction (r), which pushes the bolus of urine before it is at relatively low pressure. Because urine transport is at low pressure, any disorder that increases bladder pressure (i.e., low bladder wall compliance or bladder outlet obstruction) can elevate the risk of upper tract damage such as hydroureteronephrosis, recurrent urinary tract infections (UTIs), vesicoureteral reflux, and potentially irreversible renal damage. Gap junctions (electrochemical communication between ureteral muscle cells) allow the ureter to function as a single unit to propel urine forward through the entire ureter to the bladder in one single peristaltic contraction, even if innervation to the ureter is compromised or the ureter is transplanted (Gray, 2006; Gray & Moore, 2009). In addition to mechanical distention, neurologic, endocrine, and pharmacologic factors aid in ureteral peristaltic action. Sympathetic stimulation within the ureteral wall of the alpha adrenergic receptors cause increase strength and number of contractions, while beta adrenergic stimulation causes relaxation of the ureter. Parasympathetic stimulation of cholinergic receptors with medications such as epinephrine (catecholamine) creates strong peristaltic action.
CLINICAL PEARL
Since urine transport is at low pressure, any disorder that increases bladder pressure (i.e., low bladder wall compliance or bladder outlet obstruction) can elevate the risk of upper tract damage such as hydroureteronephrosis, recurrent UTIs, vesicoureteral reflux, and potentially irreversible renal damage.
The UVJ plays a pivotal role in promoting antegrade urine flow from the kidney into the bladder and preventing reflux (retrograde movement) from the bladder to the upper tracts. It consists of the distal ureter, the adjoining bladder wall, and the trigone of the bladder, which acts together as a unit to prevent retrograde urine movement by three methods (Gray, 2004; Gray & Moore, 2009). First, the terminal ureter tunnels the adjacent bladder wall and trigone at a gentle angle for about 1.5 cm. This layout promotes sealing of the ureter when the bladder or trigone contract. The outer layer (adventitia) of the intramural (tunneled) ureter contains three sheaths known as Waldeyer sheath, to provide limited mobility and solid attachment to the bladder. Second, the smooth muscle bundles arranged in a circular and longitudinal manner within the bladder offer additional support as well as promotion of UVJ closure during urination. Lastly, the trigone is a triangular-shaped smooth muscle at the base of the bladder with the apex extending into the bladder neck in women and the verumontanum (an elevation in the floor of the prostrate where seminal ducts enter) in men.
The trigone is divided into two distinct segments, superficial and deep (Gray & Moore, 2009). Urine is expelled into the bladder following a peristaltic contraction through a flaplike fold of the mucous membrane. This fold acts like a valve at the UVJ in that it allows urine to enter the bladder but prevents backing up of urine from the bladder to the ureter even during coughing, sneezing, and physical exertion (Shier et al., 2013a). As the bladder fills with urine, both the detrusor and trigone regions are relaxed due to sympathetic nerve stimulation to allow urine to pass through the UVJ. Beta adrenergic receptors in the bladder cause smooth muscle relaxation, while alpha adrenergic receptors in the bladder neck cause the smooth muscle to contract to prevent urine leakage while filling and storage.
In contrast, during micturition, the bladder contracts due to parasympathetic stimulation of the cholinergic receptors and indirectly inhibits sympathetic stimulation of the bladder neck (causes relaxation of bladder neck) to promote urine elimination. The contraction of the bladder and trigone raises the closing pressure of the intramural ureter (UVJ) to prevent reflux. Moreover, the trigone contracts an additional approximately 20 seconds after micturition to further lessen the risk of reflux (Gray & Moore, 2009).
CLINICAL PEARL
The UVJ prevents retrograde urine flow from the lower to upper urinary tract.
Structure and Function of the Lower Urinary Tract
The lower urinary tract consists of the bladder, urethra, and pelvic floor muscles. These structures work together as a unit to maintain continence through storage and elimination of urine at a desirable time.
Urinary Bladder
The urinary bladder is a hollow, muscular organ that has a fixed base and quite a dispensable body designed to fill with urine at low pressures, store approximately 300 to 600 mL in the healthy adult, and eliminate urine. The bladder lies within the pelvic cavity and is located posterior to the symphysis pubis and inferior to the parietal peritoneum. In females, the anterior uterine wall and vagina come in contact with the bladder, while in males, the posterior bladder neighbors the rectum (Shier et al., 2013a). The pressure of surrounding organs modifies the spherical shape of the bladder, but the size and shape of the bladder are dependent upon the amount of urine being stored. Often, anatomic drawings inaccurately depict an air bubble in the bladder; however, as the bladder empties, the walls collapse down upon the fixed base creating a tetrahedron (triangular pyramid)-like shape.
As the bladder fills, the superior surface expands upward into a dome; it pushes above the pubic crest if distended and near the umbilicus if greatly distended (Shier et al., 2013a). The trigone is the anterior floor of the bladder with an inlet at each of the angles, the UVJ orifices as described above and a funnel-shaped extension into the apex of the trigone is called the bladder neck or UVJ. There are four histological layers in the wall of the bladder: mucosa, lamina propria or submucosa, muscularis, and serous coat or adventitia (Gray & Moore, 2009; Shier et al., 2013). The mucosa coat is composed of several thicknesses of the transitional epithelial cells or uroepithelium that are similar to the lining of the renal pelvis and ureters as well as the upper portion of the urethra. The thickness of this layer becomes reduced (only one to two cells deep) as the bladder fills and distends and returns to five to seven cells deep with urine elimination.
The uroepithelium is impermeable to the contents of the urine and manufactures a very thick, mucoid-like substance called glycosaminoglycans (GAG layer) to protect the mucosa from irritants in the urine. The second layer, lamina propria, is loosely connected to the uroepithelium but firmly attached to the third layer, muscularis. It contains connective tissue, nerves, blood vessels, as well as interstitial cells that communicate considerably by gap junctions. The third layer consists of a complex meshwork of smooth muscle bundles (unlike the organized circular and longitudinal layers of the intestine) known as the detrusor muscle. The muscle layer contains collagen and elastin to provide structural integrity to the bladder.
Unfortunately, some lower urinary tract disorders such as seen in specific types of denervation and obstruction result in excessive collagen deposition. This consequence creates trabeculation (thickening or hypertrophy of bladder muscle) and ineffective contractility of the bladder leading to elevated urine residuals, elevated risk for UTIs, and compromised upper tract urine production and drainage (Casey, 2011; Gray & Moore, 2009). The muscularis also contains interstitial cells connected by gap junctions to provide communication and coordination of detrusor activity.
The fourth layer is the serosal coat or adventitia. It covers most of the bladder with fibroelastic connective tissue except the upper portion of the bladder where simple squamous epithelium covers the area along with a small amount of connective tissue. Perivesical fat covers beyond the serosa/adventitia. The bladder receives its arterial blood supply via the superior, inferior, and medial vesical arteries, in addition to branches of the obturator, inferior gluteal, or internal iliac arteries. Females also receive arterial blood to the bladder from uterine and vaginal arteries.
CLINICAL PEARL
The urinary bladder is also known as the detrusor muscle. The detrusor smooth muscle contains collagen and elastin.
Urethra
Urine is expelled from the bladder through a collapsible tube called the urethra. Like the upper urinary tract and bladder, the urethra is composed of the same four histological layers (urothelium, lamina propria, muscularis, and serosa or adventitia) but differs in that it is composed of both smooth and specialized striated muscle that aids in maintaining continence. The urethra has specialized striated muscle that contains both fast-twitch and short-twitch muscle fibers that aid in tone of the urethra during periods of sudden increase in abdominal pressure (i.e., cough) and prolong periods needed for continence between voids. In females, the urethra is about 4 cm in length (3.5 to 5.5 cm), which begins at the bladder neck and terminates at the urethral meatus between the vagina and clitoris.
To promote female continence further, the anterior vaginal wall is fused with the distal two thirds of the urethra and shares vascular components, muscular and endopelvic fascial support (Gray & Moore, 2009; Pradidarcheep et al., 2011; Sampselle & DeLancey, 1998). The female urethra is obviously short compared to the male urethra but acts as a continence mechanism almost the entire length. In contrast, the male urethra is approximately 23 cm in length and acts as a passageway to transport not only urine but cells and secretions from the reproductive organs. It can be divided into three sections: prostatic urethra approximately 3 cm, membranous urethra approximately 2.5 cm, and penile urethra approximately 15 cm (Shier et al., 2013a).
The male urethra is composed of uroepithelium, lamina propria, muscularis, and adventitia but devoid of the muscularis layer in the distal portion. The proximal urethra wall contains both smooth and striated muscle that contributes to the continence sphincter mechanism. Females receive their urethral arterial blood supply from the vaginal artery while males receive theirs from the pudendal artery. Venous return occurs from the venous pelvic plexus in females; in males, venous return occurs through the deep dorsal vein. Lymphatic drainage takes place through the superficial and deep inguinal nodes, hypogastric, obturator, as well as internal and external iliac nodes.
Pelvic Floor
The pelvic floor consists of several muscle groups and ligaments that help support the pelvic viscera and deliver sphincter-like action in the anal canal and vagina (Ashton-Miller & DeLancey, 2007; Perucchini & DeLancey, 2008; Sampselle & DeLancey, 1998).
CLINICAL PEARL
The lower urinary tract is also supported by the perineal membrane and anal sphincter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Elimination of Urine
Elimination of Urine Function of the Kidneys
Function of the Kidneys Fluid and Electrolyte Balance
Fluid and Electrolyte Balance Conclusions
Conclusions