Fecal Stoma Construction
A stoma is a surgically created opening in the gastrointestinal tract or within the urinary system. The word stoma comes from the Greek word for mouth. Writings about spontaneous stomas occur throughout history, and many of these stomas were originally the result of battle-related wounds or disease. Over the years, surgical techniques improved as did techniques for stoma construction. These advancements enhanced a surgeon’s ability to treat disease or repair and minimize the effects of trauma, thereby saving lives (Wu, 2012). Optimizing quality of life and maintaining good health are now primary goals for a person with an ostomy. Preoperative stoma site marking, ideal stoma construction, and the promotion of self-care through postoperative fitting of ostomy system and management contribute to enhanced quality of life for the individual with a stoma.
There are a variety of classifications of stomas, including by level of permanence (temporary or lifelong), by anatomic name, or by surgical construction (Table 7-1). Temporary stomas usually remain in place for 3 to 6 months but may become permanent for 20% to 50% of individuals (Forgoine & Cataldo, 2003; Pine & Stevenson, 2014; Wexner et al., 1993; Kairaluoma et al., 2002). An example would be a patient with an ostomy after bowel resection that chooses to keep the stoma rather than undergoing another operation to restore bowel continuity.
TABLE 7-1 Stoma Classifications
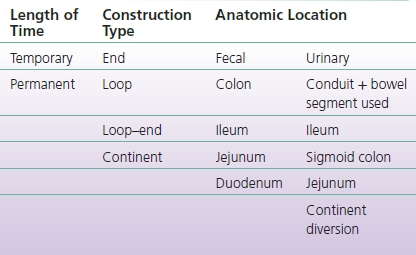
There are two broad anatomic categories of abdominal stomas: fecal and urinary. Stomas are further anatomically categorized by construction as end, loop, and loop–end. The concept of maturation is important when discussing stomal construction and will be addressed first.
Fecal Stoma Construction
Stoma Maturation
Initially, stomas were created flush to skin level. This technique resulted in severe tissue destruction as stomas were very difficult to manage due to leaking of the pouching system. The concept of a spouted (non–skin level) stoma was introduced in 1913; however, this exposed the serosal layer of the intestine to the air, resulting in inflammation called serositis. As a result of serositis, there is massive edema of the stoma with a risk for partial or complete obstruction, diarrhea, fluid and electrolyte imbalances, and dehydration (Kaidar-Person et al., 2005; Martin & Vogel, 2012; Wu, 2012). Eventually, these stomas would self-mature. Maturation refers to the eversion of the bowel segment to expose the mucosa. Stomas not matured at surgery undergo self-maturation, a process that occurs when the inflamed and gummy serosal surfaces adhere to each other, causing a gradual eventual eversion of the stoma (Doughty, 2004).
Eversion of the bowel is a gradual process taking approximately 4 to 6 weeks. The stoma will look the same at the end of this process as a matured stoma. An unmatured stoma is difficult for patients to deal with due to the large size and dramatic appearance. The concept of eversion or primary maturation introduced by Dr. Bryan Brooke in 1952 paved the way for increased survival for the majority of individuals requiring ostomy surgery; this technique is referred to as a Brooke stoma (Kaidar-Person et al., 2005; Martin & Vogel, 2012; Wu, 2012). In primary maturation, the intestinal segment is brought through the predesignated site and everted, similar to cuffing a sleeve. The matured stoma will expose the inner mucosal lining of the bowel with a beefy red, shiny, and moist surface. There are stretch receptors, so patients may sometimes feel a stretch as the bowel content exits the stoma, particularly if a large, formed stool passes through similar to bowel motions encountered with a sigmoid colostomy.
CLINICAL PEARL
There are no sensory nerve endings in the stoma.
Stoma Construction Types
There are three anatomic stoma construction types: end, loop, and loop–end (Table 7-2).
TABLE 7-2 Stoma Construction Types
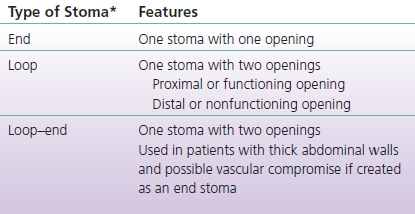
*Anatomic location dictates type, amount, and quality of effluent.
CLINICAL PEARL
End stoma construction results in one stoma with one opening.
End Stoma
To create the end stoma, the surgeon, after surgical management of the disease process or traumatic event, prepares and mobilizes the bowel segment needed for the stoma. The well-vascularized bowel segment is then brought through a predetermined abdominal aperture to create the stoma (Fig. 7-1). This aperture is two fingerbreadths in size in order to minimize the risk of herniation or prolapse (Forgione & Cataldo, 2003; Garofalo, 2012; Martin & Vogel, 2012; Pine & Stevenson, 2014; Saunders & Hemingway, 2008; Stocchi, 2012). The application of sterile dressings or drapes protects the incision from possible fecal contamination; maturation of the stoma follows. The edge of this intestinal segment is everted using four equidistant sutures placed through the entire bowel wall followed by suturing through the subcuticular (dermal) layer of the adjacent skin (Fig. 7-2). This is done to prevent seeding of the epidermis with mucosal cells, which can result in peristomal mucosal implants.
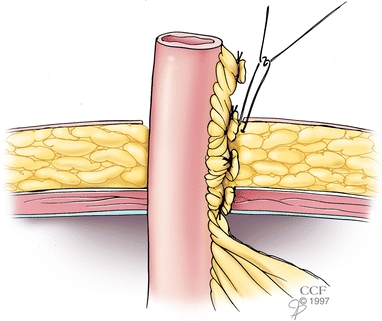
FIGURE 7-1. End ileostomy. The end of the ileum is brought through the preselected stoma site.
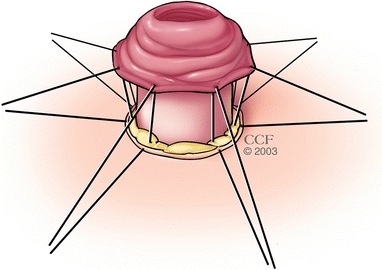
FIGURE 7-2. Stoma maturation. Absorbable sutures are placed through the full thickness of the bowel wall and secured to the subcuticular (dermal) layer of skin only. Full-thickness suturing of the skin (through the epidermis) can result in tracking of mucosal cells through the epidermis, resulting in mucosal implants.
It is important to bring a well-vascularized bowel segment through the abdominal wall without tension or twisting (Martin & Vogel, 2012; Saunders & Hemingway, 2008; Wu, 2003). Once full eversion is accomplished, additional sutures are added to complete the process, and the newly created stoma is ready for the appropriate pouching system (Garofalo, 2012). End ileostomies should protrude from the skin approximately 2 to 3 cm (Martin & Vogel, 2012; Stocchi, 2012). The formation of a spout should prohibit the effluent from going beneath the pouching system (Fig. 7-3). End colostomies should protrude, but flush construction may also occur (Forgione & Cataldo, 2003; Garofalo, 2012; Martin & Vogel, 2005; Saunders & Hemingway, 2008).
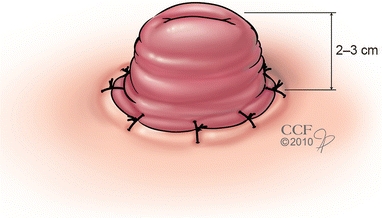
FIGURE 7-3. Matured end ileostomy. The stoma ideally protrudes 2 to 3 cm above skin level. This helps to protect the skin from stomal output and makes for easier pouching.
Loop Stoma
In general, loop stoma construction usually protects a distal anastomosis or diverts from a downstream obstruction. After completion of the surgery on the distal intestinal anastomosis, the surgeon brings a loop of intestine, usually located 12 to 15 cm from the ileocecal valve for an ileostomy (Martin & Vogel, 2012), through a predetermined site on the abdomen. It is important that the proximal and distal ends of the intestine are properly identified in order to maintain appropriate anatomic orientation. The distal limb is marked with a catgut (brown) suture, and the proximal limb is marked with a blue (Vicryl) suture “(brown for the earth [i.e., [sic], down or distal] and blue for the sky [i.e., [sic], upward or proximal])” (Martin & Vogel, 2012, p. 25). A plastic rod, tubing, or similar device is placed under the loop of intestine to provide support in order to prevent early retraction of the stoma (Fig. 7-4).
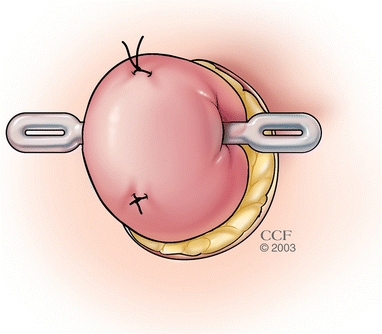
FIGURE 7-4. Loop ileostomy construction. Note the placement of sutures (each would be in a different color) that help maintain appropriate orientation of the proximal and distal portions of the intestine. The loop of the small bowel is brought out through the predetermined stoma site, and a rod is placed underneath the intestine and on top of the skin in order to provide support to the intestinal loop.
After closing the abdominal wounds, sterile dressings or towels protect the incision from contamination when opening the bowel. The intestine is then cut open about 5/8ths of its circumference. The intestine remains joined along its mesenteric or inside edge, and maturation of the two cut edges creates one stoma with two openings (Figs. 7-5 and 7-6). The proximal opening is the functional lumen through which effluent will pass. The distal lumen leads to the lower intestine; a small quantity of mucus will occasionally pass from the distal lumen or anus. The proximal lumen usually protrudes more from the abdomen than the distal lumen (Fig. 7-7).
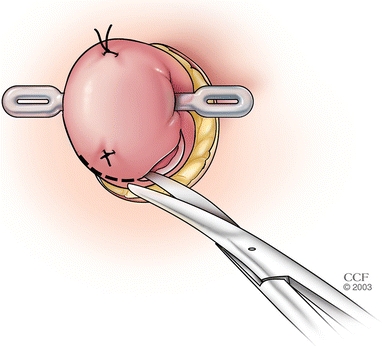
FIGURE 7-5. Loop ileostomy construction. The appropriate area of the intestine is opened from one side to the other, leaving intact intestine on the underside.
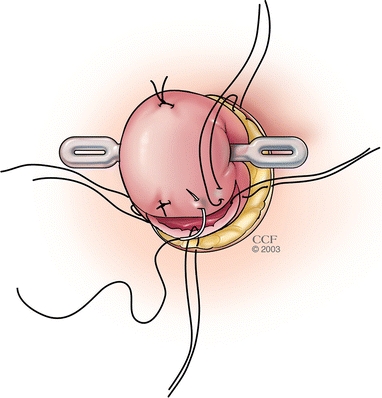
FIGURE 7-6. Loop ileostomy construction. Maturation of the stoma: Note the placement of the sutures through full thickness of the intestinal wall and the subcuticular (dermal) layer of the skin.
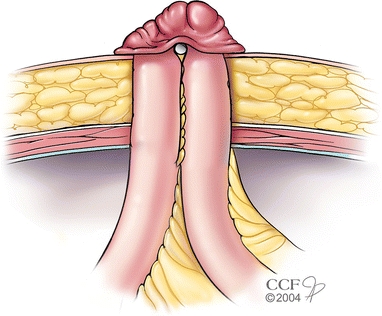
FIGURE 7-7. Matured loop ileostomy: The proximal (afferent) limb of the stoma is the protruding end, and the distal (efferent) limb is flush to skin level.
The rod under the stoma stays in place for 2 to 7 days depending on whether the case is laparoscopic or open, the amount of tension present on the rod, and surgeon preference (Garofalo, 2012; Martin & Vogel, 2012; Pine & Stevenson, 2014; Stocchi, 2012). For example, the rod remains in place for 2 days following a laparoscopic creation of the stoma and 3 days following conventional surgery. As with an end stoma, it is important to bring the intestine used to create the stoma through the abdominal opening with as little tension as possible, a good blood supply, and with normal orientation of the mesentery.
CLINICAL PEARL
The loop stoma is one stoma with two openings, proximal and distal. The loop stoma protects a distal anastomosis.
Loop–End Stoma
With loop–end construction, the intestine is transected from the lower bowel. After closing this end with a stapler, a loop of intestine approximately 10 cm proximal to this stapled end is brought to the abdominal surface through the premarked stoma site. Loop type construction is then used to create the stoma (Martin & Vogel, 2012; Stocchi, 2012; Wu, 2003). Externally, there is no difference in how a loop or loop–end stoma looks. With loop–end construction, the distal lumen leads to a blind pouch. The blind segment is usually not very long and will produce mucus as the bowel is viable. A loop–end ileal conduit uses this type of construction, which is discussed in more detail under ileal conduits. The rod under this type of urinary stoma is generally kept in place for 5 days versus the 2 to 3 days for a bowel stoma. Loop–end construction is used in bowel stomas when the person has a thick abdominal wall, shortened mesentery, or a combination, and there is concern about adequate blood supply to the distal end of the stoma (Figs. 7-8 and 7-9). Additionally, when there is a need for a permanent stoma and a loop stoma is already present, the distal limb can be transected and the stoma converted to loop–end construction (Martin & Vogel, 2012; Stocchi, 2012; Wu, 2003).
CLINICAL PEARL
Loop-end stoma is sometimes called Turnbull loop-end stoma.
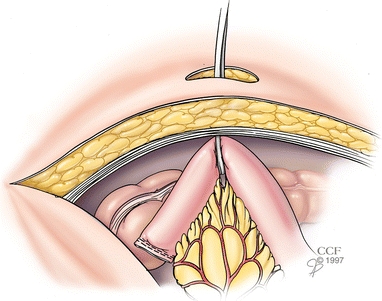
FIGURE 7-8. Loop–end ileostomy construction: Distal intestine is removed or left dormant. The proximal end of the intestine is stapled closed. The vascular arcade is protected with this technique.
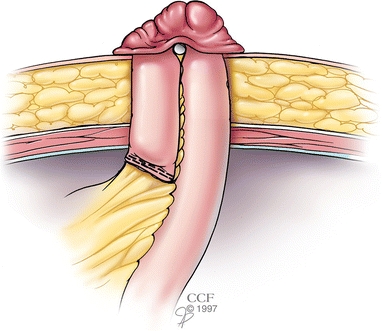
FIGURE 7-9. Loop–end ileostomy construction: A loop of intestine above this staple line is brought through the premarked site, and a loop of ileum is matured. This creates one stoma with a proximal, functioning lumen and a short distal segment.
Double-barrel ostomy construction is seen rarely; when it is, it usually occurs with colostomies. Two stomas are created in proximity to each other, resembling the end of a double-barrel shotgun, hence the name. The proximal stoma is functional, and the distal stoma serves as a mucous fistula (Saunders & Hemingway, 2008). Double-barrel construction prevents any effluent from flowing into the distal stoma (mucous fistula). Indications for this type of stoma construction include massive infection and situations of distal obstruction where the bowel above the obstruction needs venting. Leaving a blind loop in the abdomen increases the risk for perforated viscus; there needs to be a way for the mucus to exit the bowel. Pouching can be difficult with double-barrel ostomies depending on how far apart the stomas are.
CLINICAL PEARL
Duodenostomy and jejunostomy are rare and usually done following a catastrophic event.
Anatomic Classification
Duodenostomy
Duodenostomies, that is, stomas in the duodenum, are rarely done. This type of stoma sometimes indicates an abdominal catastrophe, such as an embolism to the superior mesenteric artery (SMA). Management of a duodenostomy is similar to that of the jejunostomy; peristomal skincare and management of dehydration, electrolyte disturbances, and high-volume output are major challenges. The location of these stomas is in the midline and near body creases, which is a direct result of limited bowel length secondary to the initial catastrophic event; this location creates significant pouching challenges. These patients tend to require much emotional support as minimal preoperative education is performed due to the emergent nature of surgery. Pouching considerations are the same as with jejunostomies.
Jejunostomy
The location of jejunostomies is usually in the left upper quadrant of the abdomen. Creation of this stoma type is generally a result of an abdominal catastrophe or the need to protect a distal anastomosis. Jejunostomies produce high volumes of liquid output (Bafford & Irani, 2013; Martin & Vogel, 2012; Rombeau, 2012); chunks of food can be seen in the output if the person is taking food orally. These stomas typically begin function on days 1 to 3 postoperatively. The initial output is a dark green viscous liquid. The output from a jejunostomy is neutral to slightly alkaline with a pH ranging from 7 to 9 and contains activated digestive enzymes.
When jejunal effluent contacts the skin, the activated enzymes digest the epidermis, rapidly exposing the dermis. Peristomal moisture-associated skin damage is moist, red, and painful with a burning, stinging sensation, particularly when effluent comes in contact with the denuded area. Issues of concern are protection of the peristomal skin from stoma output, containment of high-volume output, and management of fluid and electrolyte disturbances (Colwell et al., 2011; Gray et al., 2013; Krapfl & Zurcher, 2010). Individuals with jejunostomies run the risk of dehydration and may require total parenteral nutrition to maintain proper nutrition and fluid intake; use of medication to slow intestinal motility is common (Parekh & Seidner, 2012). Suggested for use with liquid output are pouching systems with extended wear barriers, which have components that withstand liquid output better than do standard wear barriers (Goldberg et al., 2010). High-volume output pouches are standard. The output has minimal odor.
Ileostomy
Ileostomies, usually located in the right lower quadrant, have output that ranges from a liquid to a mushy (applesauce or pudding) consistency depending upon the location in the ileum. The higher the ileostomy, that is, the closer the stoma is to the stomach, the more liquid the output and the greater the enzyme content. Ileostomies begin to function from 1 to 3 days postoperatively. The effluent is usually a dark green liquid with a viscous appearance. There is potential for significant peristomal moisture-associated skin damage if the effluent contacts the peristomal skin. The preference is for extended wear skin barriers (Goldberg et al., 2010; Registered Nurses’ Association of Ontario [RNAO], 2009). Drainable pouches are the norm; if an individual has high-volume output, the recommendation is to use high-volume output pouches.
Cecostomy
Cecostomies are rarely done, and when they are, it is as a tube cecostomy. The tube cecostomy acts to decompress the colon, treat cecal volvulus, or manage perforation of the cecum when resection is not an option (Garofalo, 2012; Saunders & Hemingway, 2008). A large-bore tube or catheter is inserted into the cecum, secured to the skin, and connected to gravity drainage. The output is liquid with particles, is malodorous, and frequently clogs the drainage tubing even with irrigation (Garofalo, 2012). Leakage around the catheter or tube is very common, and peritubular moisture-associated skin damage can occur.
Colostomy
Ascending colostomies are another rare type of stoma. They have output similar to cecostomies in that it is semiliquid with a strong odor secondary to the effects of colonic bacteria (Martin & Vogel, 2012). The effluent can cause considerable tissue destruction to the peristomal skin. Fluid and electrolyte imbalances are also a concern.
Transverse colostomies may be in the right upper quadrant, midabdomen, or left upper quadrant depending upon where in the transverse colon the stoma creation occurs. The stool is a liquid to a pasty consistency and usually malodorous. They are generally created for protection of an anastomosis or to relieve a distal obstruction and are often constructed as part of an emergent surgery (Garofalo, 2012). Stomal prolapse, particularly of the distal lumen in loop transverse colostomies, and hernia formation are common problems seen in transverse colostomies. Pouching can be problematic, should these problems occur.
The location of a descending or sigmoid colostomy is usually in the left lower quadrant. The stool is a pasty to a formed consistency; the stool is not as irritating to the skin as ileostomy effluent but can still cause peristomal moisture-associated skin damage (Fig. 7-10). Depending upon how often the stoma functions, an individual will use either a drainable pouch or closed-end pouch. A closed-end pouch is recommended if the stoma functions once to twice a day. Individuals with a descending or sigmoid colostomy may choose to irrigate the stoma to control its activity. Irrigation entails instilling water into the bowel at the same time every day in order to stimulate the bowel to function. This procedure is discussed in more detail in Chapter 12.

FIGURE 7-10. Matured end colostomy. Note the degree of stomal eversion and presence of sutures to secure mucocutaneous junction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Urinary Stoma Construction
Urinary Stoma Construction Conclusions
Conclusions