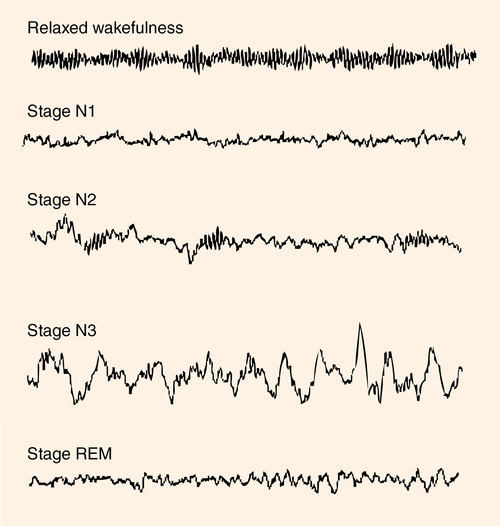
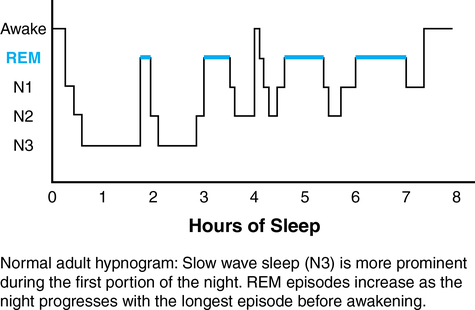
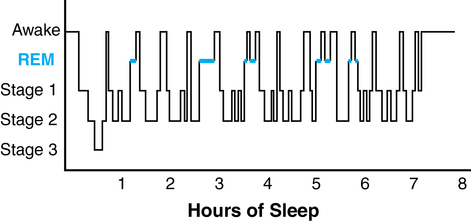
CHAPTER 19 1. Discuss the impact of inadequate sleep on overall physical and mental health. 2. Describe the social and economic impact of sleep disturbance and chronic sleep deprivation. 3. Recognize the risks to personal and community safety imposed by sleep disturbance and chronic sleep deprivation. 4. Describe normal sleep physiology and explain the variations in normal sleep. 5. Identify the major categories and medical diagnoses for sleep disorders. 6. Identify the predisposing, precipitating, and perpetuating factors for patients with insomnia. 7. Apply the nursing process in caring for individuals with sleep disorders. 8. Describe the use of two assessment tools in the evaluation of patients experiencing sleep disturbance. 9. Formulate three nursing diagnoses for patients experiencing a sleep disturbance. 10. Develop a teaching plan for a patient with insomnia disorder, incorporating principles of sleep restriction, stimulus control, and cognitive-behavioral therapy. 11. Develop a care plan for the patient experiencing sleep disturbance incorporating basic sleep hygiene principles. Visit the Evolve website for a pretest on the content in this chapter: http://evolve.elsevier.com/Varcarolis Sleep and sleep disorders are receiving increased attention in the medical, nursing, research, and social science literature. Obtaining sufficient quality sleep is now recognized as a key determinant of health and well-being (Grandner, 2012). Healthy People 2020 added sleep health to the list of current health topics, making sleep a national health priority. Sleep has become an expendable commodity. In a fast-paced society, sleep is often forfeited, and people subject themselves to schedules that disrupt normal sleep physiology. People frequently cut back on sleep to meet other social and vocational demands with compensated work time, time in academic activities, and travel time to and from work and school being the most potent determinant of total sleep time; the more time devoted to work-related activities, the less time spent sleeping (Knutson et al., 2010). The NSF (2012a) recommends that the average adult get 7 to 9 hours of sleep each night, yet annual surveys conducted by the NSF between 2002 and 2012 have consistently demonstrated that the average adult gets less than 7 hours of sleep most nights of the week (NSF, 2012b). While currently there seems to be some debate as to whether secular sleep trends have decreased over the last century (Bin et al., 2012), it does seem that the portion of short sleepers (i.e., individuals who sleep 6 hours or less per night) has increased over the last several decades among full-time workers, a period when the prevalence of chronic disease (such as diabetes, cardiovascular disease, and obesity) that may be linked to sleep has also significantly increased (Knutson et al., 2010). Many of the neurocognitive symptoms of chronic sleep deprivation can mimic psychiatric symptoms, highlighting the importance of a comprehensive sleep evaluation for patients with mental health disorders. In a recent multiethnic, representative sample of U.S. adults, insufficient sleep/rest was shown to be positively associated with poor self-rated health (Geiger et al., 2012). Adults who sleep less than 6 hours per night are more likely to report fair to poor general health, mood disturbance, increase in pain syndromes/perception, impaired cognitive function and memory disturbance, and reduction in measures of overall quality of life (Grandner et al., 2010). Short and long sleep duration (sleeping less than 6 hours per night or greater than 8 hours per night) is associated with up to a twofold increased risk of obesity, diabetes, hypertension, cardiovascular disease, stroke, depression, substance abuse, and all-cause mortality in multiple studies (NCSDR, 2011). Less than 6 hours of sleep per night is associated with impaired glucose tolerance, elevated cortisol levels, and alterations in sympathetic nervous system activity. Sleep deprivation may be linked to obesity since it is associated with dysregulation of leptin (a hormone that regulates satiety or feelings of fullness) and ghrelin (a hormone that regulates hunger). Less than 6 hours of sleep per night may also increase pro-inflammatory markers such as C-reactive protein, tumor necrosis factor, and interleukin (Luyster et al, 2012). All these problems are common pathways to the development of cardiovascular disease and diabetes. Mechanisms linking long sleep time with vascular and metabolic morbidities are unknown but may be related to cofounders such as depression, inactivity, low socioeconomic status, and overall poor general health (Luyster et al., 2012). Sleep loss diminishes safety and results in the loss of lives and property. Sleep deprivation can produce psychomotor impairments equivalent to those induced by alcohol consumption at or above the legal limit. Daytime wakefulness in excess of 17 to 19 hours can produce psychomotor deficits equivalent to blood alcohol concentrations (BACs) between 0.05% and 0.1% (the legal limit in most states is 0.08%) (Williamson & Feyer, 2007; Insurance Institute for Highway Safety, 2012). Acute or chronic sleep deprivation can result in episodes of microsleep lasting from a second up to 10 seconds when a tired person is trying to stay awake. Many of us have experienced this when sitting in a class or in a meeting; this can lead to lower capabilities and efficiency of task performance and increased risk for errors (Orzel-Gryglewska, 2010). Some of the most devastating environmental and human tragedies of our time can be linked to human error due to sleep loss and fatigue. The grounding of the Exxon Valdez, the nuclear meltdown at Three Mile Island, and the explosion of the Union Carbide chemical plant in India are prime examples. Sleepiness with driving has become a national epidemic. The 2011 NSF Sleep in America Poll indicates that an alarming 52% of respondents admit to driving while sleepy. An incredible statistic cites one third of Americans report falling asleep while driving once or twice a month (CDC, 2010). Although researchers have tried to quantify the financial burden associated with sleep disruption, there is relatively little comprehensive data available on the economic burden of sleep-wake disorders; however, considering the prevalence, impact on overall health and quality of life, and the indirect costs associated with property loss and damage, the economic burden is likely in the billions of dollars (Skaer & Sclar, 2010). For example, a recent study estimated that chronic insomnia results in nearly $63.2 billion dollars in direct and indirect expenses annually (Kessler et al., 2011). Formal training in sleep or sleep disorders within medical and nursing education is limited, and the number of trained clinicians and scientists continues to be insufficient (Institute of Medicine [IOM], 2006). Awareness among health care providers regarding the prevalence and burden of sleep disruption and the problem of inadequate sleep is underappreciated, and providers do not routinely screen for sleep disturbance or inquire about overall sleep quality (Sorscher, 2008). Consequently, sleep disturbances may not be recognized, diagnosed, managed, and treated. NREM sleep is divided into three stages (N1, N2, N3) according to criteria by the AASM (2005) and is characterized by progressive or deeper sleep. Stage 1 (N1) is a brief transition between wakefulness and sleep and comprises between 2% to 5% of total sleep time. The time it takes to fall to sleep is referred to as sleep latency. During stage 1 sleep, body temperature declines and muscles relax. Slow, rolling eye movements are common. People lose awareness of their environment but are generally easily aroused. Stage 2 (N2) sleep occupies 45% to 55% of total sleep time; heart rate and respiratory rate decline. Arousal from stage 2 sleep requires more stimuli than stage 1. REM sleep comprises 20% to 25% of total sleep time and is characterized by reduction and absence of skeletal muscle tone (muscle atonia), bursts of rapid eye movement, myoclonic twitches of the facial and limb muscles, reports of dreaming, and autonomic nervous system variability. The atonia in REM sleep is thought to be a protective mechanism to prevent the acting out of nightmares and dreams (Carskadon & Dement, 2011). Figure 19-1 shows the EEG patterns characteristic of these sleep stages. In the adult, sleep normally begins with NREM sleep. Continuous EEG recordings of sleep demonstrate an alternating cycle between NREM and REM sleep. There are typically four to six cycles of NREM and REM sleep occurring over 90- to 120-minute intervals across the sleep period. There is also a distinct organization to sleep, with NREM predominating during the first half of the sleep period and REM sleep predominating during the second half. The shortest REM period occurs 60-90 minutes after sleep onset and lasts only for several minutes. The longest REM period occurs at the end of the sleep period and can last up to an hour. This is the reason why many people remember dreaming upon awakening in the morning (Carskadon & Dement, 2011). The structural organization of NREM and REM sleep is known as sleep architecture and is often displayed graphically as a hypnogram. Figure 19-2 is a hypnogram depicting the normal progression of the stages of sleep in an adult. The visual depiction of sleep is helpful in identifying sleep continuity (i.e., the distribution of sleep and wakefulness across the sleep period), as well as changes in sleep that may occur as a result of aging, illness, or certain medications. Disruption of sleep stages as indicated by excessive amounts of stage 1 sleep, multiple brief arousals, and frequent shifts in sleep staging is known as sleep fragmentation. Figure 19-3 is a hypnogram of a patient with a complaint of insomnia, indicating multiple brief arousals. Sleep architecture changes over the lifespan. The percentage in each stage of sleep, as well as the overall sleep efficiency, or ratio of sleep duration to time spent in bed, varies according to age. For example, infants sleep 16 to 18 hours a day, enter sleep through REM (not NREM) sleep, and spend up to 50% of sleep time in REM sleep. The percentage of REM sleep decreases to 20% to 25% by age 3 and stays relatively constant throughout old age. The amount of slow wave sleep is maximal in young children and declines with age to almost none, particularly in men. This results in a tendency for middle-of-the-night awakenings and reduced sleep efficiency with age (Bliwise, 2011). Circadian drives are near-24-hour cycles of behavior and physiology generated and influenced by endogenous and exogenous factors and are wake-promoting. The exogenous factors are various clues from the environment known as zeitgebers (time-givers) that help set our internal clock to a 24-hour cycle. The strongest external cue for wakefulness is light whereas darkness is the cue for sleep. Other environmental cues include the timing of social events, such as meals, work, or exercise (Czeisler et al., 2011). A master biological clock is located in the suprachiasmatic nucleus (SCN) of the hypothalamus. This clock regulates not only sleep but also a host of other biological and physiological functions within the body. Information about the lighting conditions of the external environment is relayed to the SCN from the retina. The SCN also receives information from the thalamus and the midbrain. These two pathways transmit photic and nonphotic information to the circadian clock through an expansive network. In addition to regulating sleep/wake cycles, they also exert control over endocrine regulation, body temperature, metabolism, autonomic regulation, psychomotor and cognitive performance, attention, memory, and emotion (Czeisler et al., 2011). In addition to the circadian and homeostatic processes, several neurotransmitter systems are responsible for sleep and wakefulness. The neurotransmitters responsible for wakefulness are dopamine, norepinephrine, serotonin, acetylcholine, histamine, glutamate, and hypocretin; sleep-promoting neurotransmitters include adenosine, gamma–aminobutyric acid (GABA), and galanin (Carney et al., 2011). Any medication that crosses the blood-brain barrier may have effects on sleep and wakefulness through modulation of these neurotransmitters. Despite remarkable advances in the understanding of sleep disorders and the biological and physiological process of sleep, very little is known about the true function of sleep. Most of the information regarding the function of sleep comes to us from animal models of sleep deprivation and human models of partial sleep deprivation. Based on these models, several theories are proposed and include brain tissue restoration, body restoration (NREM sleep), energy conservation, memory reinforcement and consolidation (REM sleep), regulation of immune function, metabolism and regulation of certain hormones, and thermoregulation (Bonnet, 2011). Polysomnography is the most common sleep test and is used to diagnose and evaluate patients with sleep-related breathing disorders and nocturnal seizure disorders (Kushida et al., 2005). The MSLT is a daytime nap test used to objectively measure sleepiness in a sleep-conducive setting. Polysomnography and MSLT performed on the day following polysomnography evaluation are routinely indicated in patients suspected of having narcolepsy. MWT evaluates a patient’s ability to remain awake in a situation conducive to sleep and is used to document adequate alertness in individuals with careers for which sleepiness would pose a risk to public safety (Littner et al., 2005). Actigraphy involves using a wristwatch-type device that records body movement over a period of time and is helpful in evaluating sleep patterns and sleep duration. It is used in patients with circadian rhythm disorders and insomnia (Morgenthaler et al., 2007). In this chapter you will review the major categories of sleep disorders. Insomnia disorders are the most common sleep disorders and will be described along with the application of the nursing process. The American Psychiatric Association (2013) identifies the following disorders: • Narcolepsy/hypocretin deficiency • Breathing-related sleep disorders • Rapid eye movement sleep behavior disorder • Substance-induced sleep disorders Hypersomnolence disorders are associated with excessive daytime sleepiness and have a prevalence of more than 15% in the general population (Ohayon et al., 2012). Hypersomnolence disorders are chronic (3 months or more) and begin in young adulthood (Ali et al., 2009). The patient with hypersomnolence reports recurrent periods of sleep or unintended lapses into sleep, frequent napping, a prolonged main sleep period of greater than 9 hours, non-refreshing non-restorative sleep regardless of amount of time slept, and difficulty with full alertness during the wake period. Excessive sleepiness significantly impairs social and vocational functioning by impacting the person’s ability to participate in and enjoy relationships and function in the workplace. Cognitive impairment is common as is an increased risk for accident or injury associated with the sleepiness.
Sleep-wake disorders
Sleep
Consequence of sleep loss
Normal sleep cycle
Sleep patterns
Regulation of sleep
Functions of sleep
Sleep disorders
Clinical picture
Hypersomnolence disorders
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Sleep-wake disorders
Get Clinical Tree app for offline access