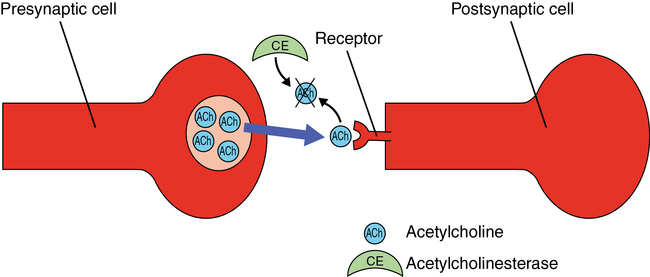
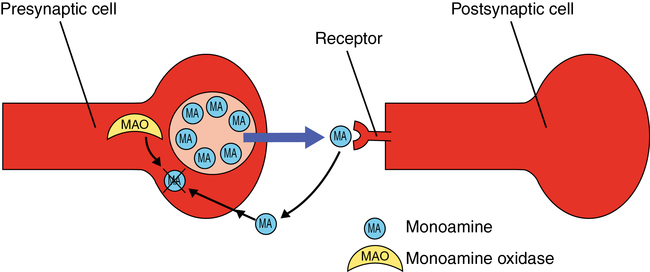
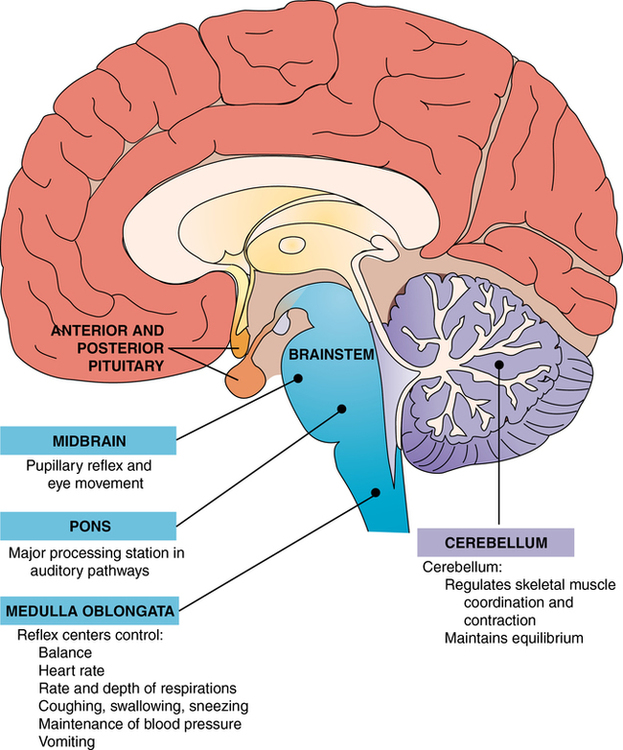
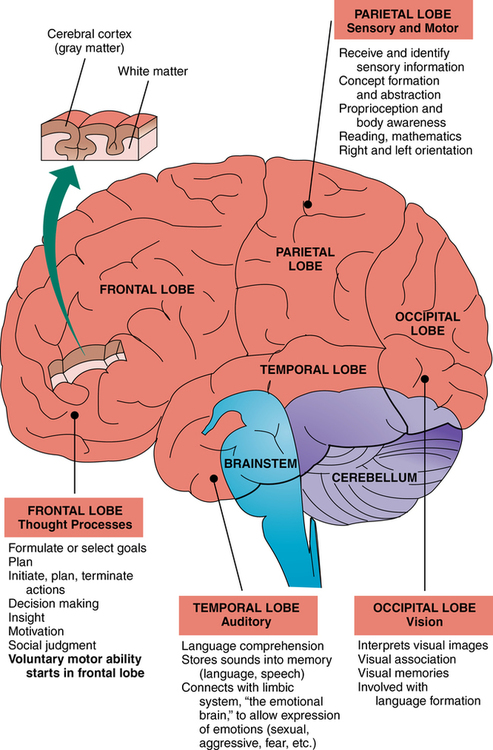
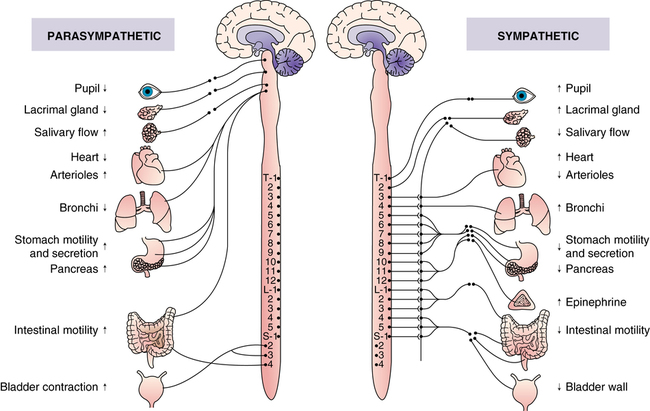
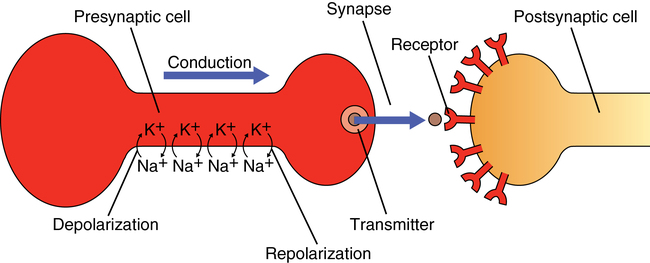
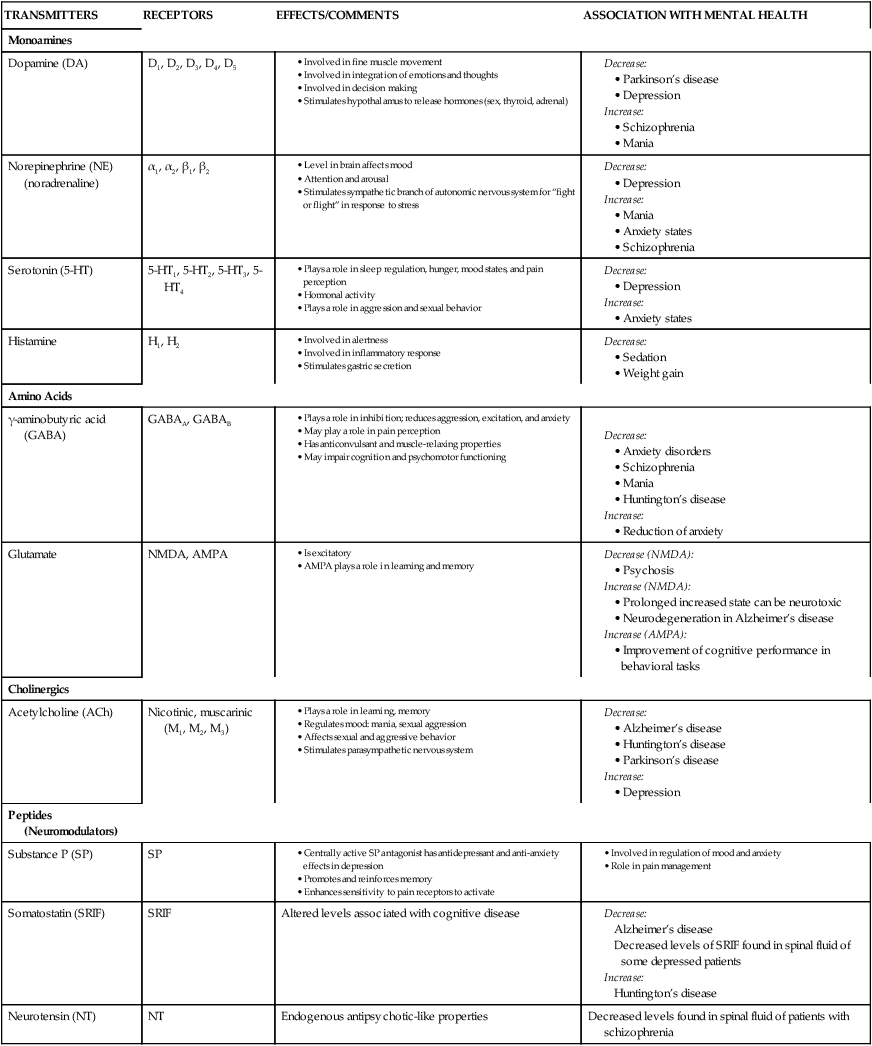
CHAPTER 3 Mary A. Gutierrez, Jerika T. Lam and Mary Ann Schaepper 1. Discuss major functions of the brain and how psychotropic drugs can alter these functions. 2. Identify how specific brain functions are altered in certain mental disorders (e.g., depression, anxiety, schizophrenia). 3. Describe how a neurotransmitter functions as a chemical messenger. 4. Describe how the use of imaging techniques can be helpful for understanding mental illness. 5. Develop a teaching plan that includes side effects from dopamine blockage (e.g., antipsychotic drugs) such as motor abnormalities. 6. Describe the result of blockage of the muscarinic receptors and the α1 receptors by the standard neuroleptic drugs. 7. Identify the main neurotransmitters that are affected by the following psychotropic drugs and their subgroups: Antianxiety and hypnotic drugs 8. Identify special dietary and drug restrictions in a teaching plan for a patient taking a monoamine oxidase inhibitor. 9. Identify specific cautions you might incorporate into your medication teaching plan with regard to the following: Genetic pharmacology (i.e., variations in effects and therapeutic actions of medications among different ethnic groups) Visit the Evolve website for a pretest on the content in this chapter: http://evolve.elsevier.com/Varcarolis Although the origin of a psychiatric illness may be related to a number of factors, such as genetics, neurodevelopmental factors, drugs, infection, and bad experiences, there is ultimately a physiological alteration in brain function that accounts for the disturbances in the patient’s behavior and mental experiences. These physiological alterations are the targets of the psychotropic (Greek for psyche, or mind, + trepein, to turn) drugs used to treat mental disease. From a holistic point of view, mental disorders have psychobiological components that support the efficacy of treating these disorders both pharmacologically and with appropriate psychotherapy, or “talk” therapy that provides social and psychological support and actually alters brain function (Karlsson, 2011). Regulating behavior and carrying out mental processes are important, but far from the only, responsibilities of the brain. Box 3-1 summarizes some of the major functions and activities of the brain. Because all of these brain functions are carried out by similar mechanisms (interactions of neurons) often in similar locations, it is not surprising that mental disturbances are often associated with alterations in other brain functions and that the drugs used to treat mental disturbances can also interfere with other activities of the brain. The autonomic nervous system and the endocrine system serve as the communication links between the brain and the cardiac muscle, smooth muscle, and glands of which the internal organs are composed (Figure 3-1). If the brain needs to stimulate the heart, it must activate the sympathetic nerves to the sinoatrial node and the ventricular myocardium. If the brain needs to bring about vasoconstriction, it must activate the sympathetic nerves to the smooth muscles of the arterioles. An essential feature of neurons is their ability to conduct an electrical impulse from one end of the cell to the other. This electrical impulse consists of a change in membrane permeability that first allows the inward flow of sodium ions and then the outward flow of potassium ions. The inward flow of sodium ions changes the polarity of the membrane from positive on the outside to positive on the inside. Movement of potassium ions out of the cell returns the positive charge to the outside of the cell. Because these electrical charges are self-propagating, a change at one end of the cell is conducted along the membrane until it reaches the other end (Figure 3-2). The functional significance of this propagation is that the electrical impulse serves as a means of communication between one part of the body and another. Once an electrical impulse reaches the end of a neuron, a neurotransmitter is released. A neurotransmitter is a chemical substance that functions as a neuromessenger. Neurotransmitters are released from the axon terminal at the presynaptic neuron on excitation. This neurotransmitter then diffuses across a space, or synapse, to an adjacent postsynaptic neuron, where it attaches to receptors on the neuron’s surface. It is this interaction from one neuron to another, by way of a neurotransmitter and receptor, that allows the activity of one neuron to influence the activity of other neurons. Depending on the chemical structure of the neurotransmitter and the specific type of receptor to which it attaches, the postsynaptic cell will be rendered either more or less likely to initiate an electrical impulse. It is the interaction between neurotransmitter and receptor that is a major target of the drugs used to treat psychiatric disease. Table 3-1 lists important neurotransmitters and the types of receptors to which they attach. Also listed are the mental disorders associated with an increase or decrease in these neurotransmitters. TABLE 3-1 AMPA, α-Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid; NMDA, N-methyl-d-aspartate. After attaching to a receptor and exerting its influence on the postsynaptic cell, the neurotransmitter separates from the receptor and is destroyed. The process of neurotransmitter destruction is described in Box 3-2. There are two basic mechanisms by which neurotransmitters are destroyed. Some neurotransmitters (e.g., acetylcholine) are destroyed by specific enzymes at the postsynaptic cell. The enzyme that destroys acetylcholine is called acetylcholinesterase (most enzymes start with the name of the neurotransmitter they destroy and end with the suffix –ase). Other neurotransmitters (e.g., norepinephrine) are taken back into the presynaptic cell from which they were originally released by a process called cellular reuptake and are either reused or destroyed by intracellular enzymes. In the case of the monoamine neurotransmitters (e.g., norepinephrine, dopamine, serotonin), the destructive enzyme is called monoamine oxidase (MAO). Located behind the brainstem, the cerebellum (Figure 3-3) is primarily involved in the regulation of skeletal muscle coordination and contraction and the maintenance of equilibrium. It plays a crucial role in coordinating contractions so that movement is accomplished in a smooth and directed manner. The cerebrum consists of surface, the cerebral cortex, and deep areas of integrating gray matter that include the basal ganglia, amygdala, and hippocampus. Tracts of white matter link these areas with each other and the rest of the nervous system. The cerebral cortex, which forms the outer layer of the brain, is responsible for conscious sensation and the initiation of movement. Certain areas of the cortex are responsible for specific sensations. For example, the sensation of touch resides in the parietal cortex, sounds are based in the temporal cortex, and vision is housed in the occipital cortex. Likewise, a specific area of the frontal cortex controls the initiation of skeletal muscle contraction. Of course, all areas of the cortex are interconnected so that an appropriate picture of the world can be formed and, if necessary, linked to a proper response (Figure 3-4). A variety of noninvasive imaging techniques are used to visualize brain structure, functions, and metabolic activity. Table 3-2 identifies some common brain imaging techniques and preliminary findings as they relate to psychiatry. There are two types of neuroimaging techniques: structural and functional. Structural imaging techniques (e.g., computed tomography [CT] and magnetic resonance imaging [MRI]) provide overall images of the brain and layers of the brain. Functional imaging techniques (e.g., positron emission tomography [PET] and single photon emission computed tomography [SPECT]) reveal physiological activity in the brain, as described in Table 3-2. TABLE 3-2 COMMON BRAIN IMAGING TECHNIQUES
Biological basis for understanding psychiatric disorders and treatments
Structure and function of the brain
Functions and activities of the brain
Regulation of the autonomic nervous system and hormones
Cellular composition of the brain
TRANSMITTERS
RECEPTORS
EFFECTS/COMMENTS
ASSOCIATION WITH MENTAL HEALTH
Monoamines
Dopamine (DA)
D1, D2, D3, D4, D5
Norepinephrine (NE) (noradrenaline)
α1, α2, β1, β2
Serotonin (5-HT)
5-HT1, 5-HT2, 5-HT3, 5-HT4
Histamine
H1, H2
Amino Acids
γ-aminobutyric acid (GABA)
GABAA, GABAB
Glutamate
NMDA, AMPA
Cholinergics
Acetylcholine (ACh)
Nicotinic, muscarinic (M1, M2, M3)
Peptides (Neuromodulators)
Substance P (SP)
SP
Somatostatin (SRIF)
SRIF
Altered levels associated with cognitive disease
Neurotensin (NT)
NT
Endogenous antipsychotic-like properties
Decreased levels found in spinal fluid of patients with schizophrenia
Organization of the brain
Brainstem
Cerebellum
Cerebrum
Visualizing the brain
TECHNIQUE
DESCRIPTION
USES
PSYCHIATRIC RELEVANCE AND PRELIMINARY FINDINGS
Electrical: Recording Electrical Signals from the Brain
Electroencephalograph (EEG)
A recording of electrical signals from the brain made by hooking up electrodes to the subject’s scalp.
Can show the state a person is in —asleep, awake, anesthetized —because the characteristic patterns of current differ for each of these states.
Provides support from a wide range of sources that brain abnormalities exist; may lead to further testing.
Structural: Show Gross Anatomical Details of Brain Structures
Computerized axial tomography (CT)
A series of x-ray images is taken of the brain and a computer analysis produces “slices” providing a precise 3D-like reconstruction of each segment.
Get Clinical Tree app for offline access

Biological basis for understanding psychiatric disorders and treatments
Get Clinical Tree app for offline access