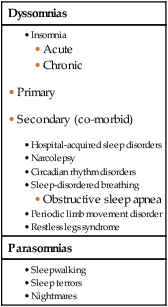
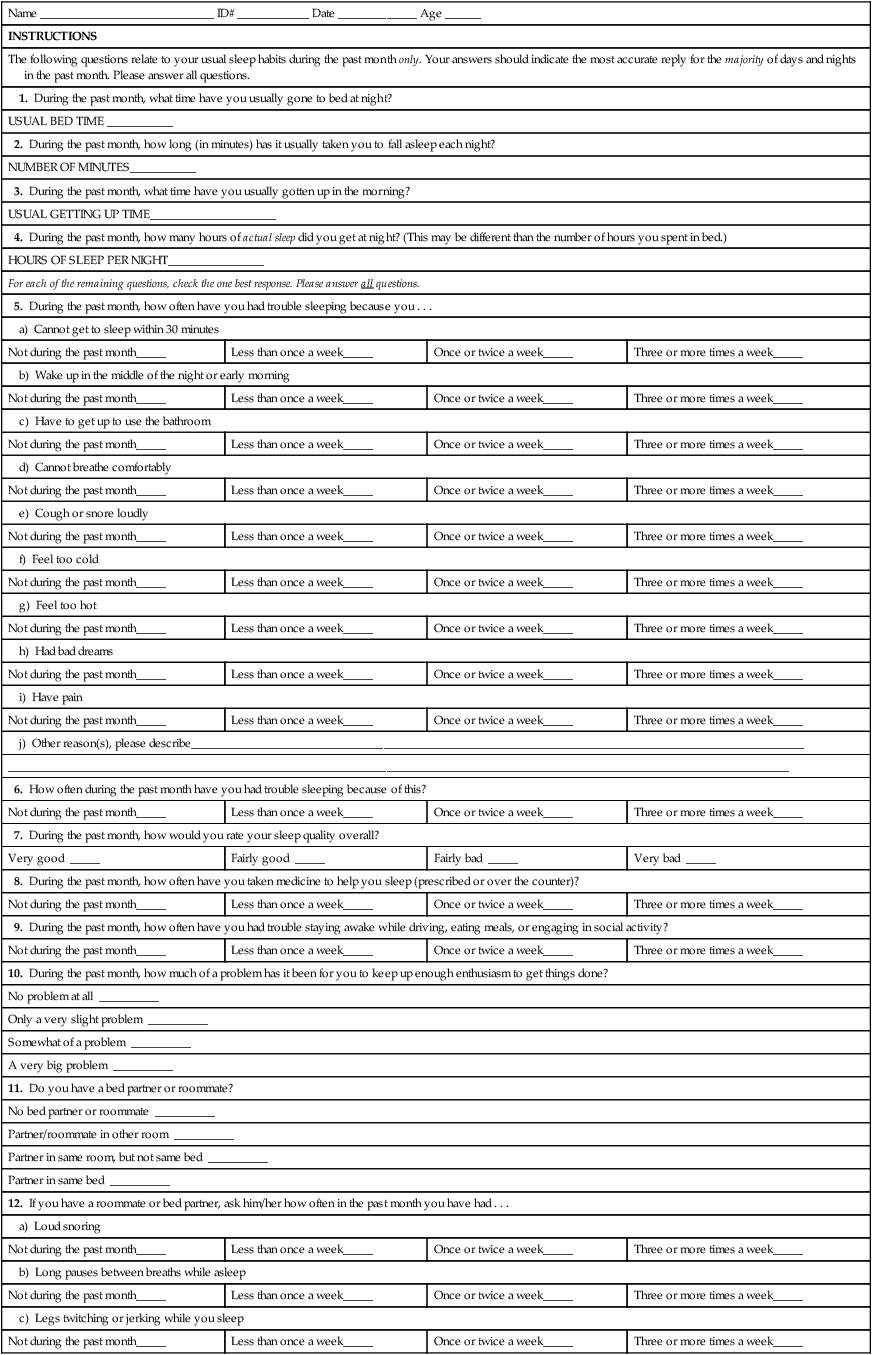
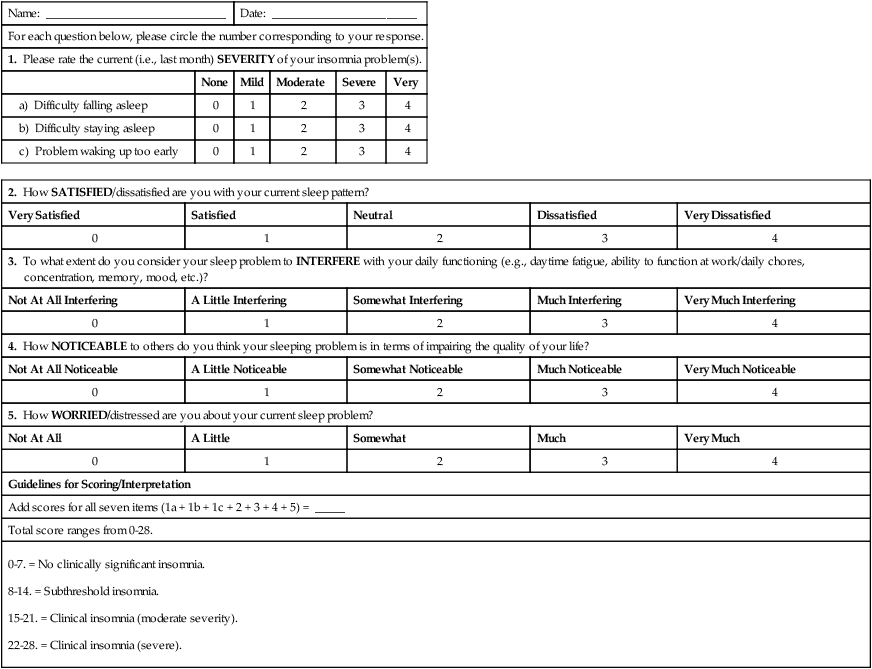
Chapter 8 Carol A. Landis and Margaret McLean Heitkemper 3. Explain the relationship of various diseases/disorders and sleep disorders. 4. Describe the etiology, clinical manifestations, and collaborative and nursing management of insomnia. 5. Describe the etiology, clinical manifestations, and collaborative and nursing management of narcolepsy. 6. Describe the etiology, clinical manifestations, collaborative care, and nursing management of obstructive sleep apnea. 7. Describe parasomnias, including sleepwalking, sleep terrors, and nightmares. 8. Select appropriate strategies for managing sleep problems associated with shift work sleep disorder. Sleep disturbance is a term used to indicate conditions of poor sleep quality. Sleep disorders are abnormalities unique to sleep. They can be classified as dyssomnias or parasomnias (Table 8-1). Dyssomnia is a term used to describe problems associated with initiating or maintaining sleep. Parasomnias are discussed later in this chapter on p. 110. TABLE 8-1 Source: Based on American Academy of Sleep Medicine: International classification of sleep disorders, 2nd ed: Diagnostic and coding manual, Westchester, Ill., The Academy, 2005. Retrieved from www.esst.org/adds/ICSD.pdf. More than 70 million people in the United States have a sleep disorder, and many are unaware that they have a problem1,2 (Fig. 8-1). On average most Americans report sleeping eTABLE 8-1 PITTSBURGH SLEEP QUALITY INDEX From Buysse DJ, Reynolds CF, Monk TH, et al: The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research, Psychiatry Res 28:193, 1989. eTABLE 8-2 © Morin CM (1993). eTABLE 8-3 © Copyright, M.W. Johns, 1990-1997. www.epworthsleepinessscale.com. eTABLE 8-4 From Kryger MH, Roth T, Dement WC: Principles and practice of sleep medicine, ed 5, Philadelphia, 2011, Saunders. Insufficient sleep is a serious problem with health consequences. In the 2011 National Sleep Foundation survey, 87% of Americans reported at least one sleep problem such as difficulty falling asleep, fragmented sleep, or snoring a few nights per week.3 Daytime sleepiness can be so severe that it interferes with work and social functioning (Fig. 8-2). People with chronic illnesses are at the greatest risk for sleep disturbances. Many sleep disorders go untreated because health care providers do not ask and patients do not talk about sleep problems. Untreated sleep disorders pose considerable health and economic consequences. Driving while drowsy is related to 100,000 accidents and 1500 traffic fatalities per year.4 Each year, sleep disorders, sleep loss, and excessive daytime sleepiness cost the United States billions of dollars from the cost of health care, work-related accidents, and lost productivity.1 Wake behavior is maintained by an integrated network of arousal systems from the brainstem and basal forebrain. A cluster of neuronal structures in the middle of the brainstem, called the reticular activating system (RAS), is associated with generalized cortical activation and behavioral arousal. Various neurotransmitters (glutamate, acetylcholine, norepinephrine, dopamine, histamine, serotonin) promote wake behavior.5 Orexin (also called hypocretin), a neuropeptide, is found in the lateral hypothalamus. Orexin activates arousal systems and simultaneously inhibits sleep active neurons. Decreased levels of orexin or its receptors lead to difficulties staying awake and the syndrome called narcolepsy. (Narcolepsy is discussed later in this chapter on pp. 106-107.) An area in the hypothalamus just above the optic chiasm contains many sleep-promoting neurons. These neurons act to inhibit the RAS and promote sleep.5 Sleep is stimulated by a variety of sleep-promoting neurotransmitters and peptides, including γ-aminobutyric acid (GABA), galanin, melatonin, adenosine, somatostatin, growth hormone–releasing hormone, delta-sleep–inducing peptide, prostaglandins, and proinflammatory cytokines (interleukin-1, tumor necrosis factor, interleukin-6). Proinflammatory cytokines are important in mediating sleepiness and lethargy associated with infection. Peptides, such as cholecystokinin, released by the gastrointestinal tract after food ingestion may mediate the sleepiness (postprandial sleepiness). Melatonin is an endogenous hormone produced by the pineal gland in the brain from the amino acid tryptophan. Melatonin secretion is tightly linked to the environmental light-dark cycle. Under normal day-night conditions, melatonin is released in the evening as it gets dark. Light exposure at night can suppress melatonin secretion.6 Many biologic rhythms of behavior and physiology fluctuate within a 24-hour period. Because the circadian (circa dian, about a day) rhythms are controlled by internal clock mechanisms, they persist when people are placed in environments free of external time cues. The suprachiasmatic nucleus (SCN) in the hypothalamus is the master clock of the body. The 24-hour cycle of sleep and wake is synchronized to the environmental light and dark periods through specific light detectors in the retina. Pathways from the retina reach the SCN, and pathways from the SCN innervate brain regions controlling wake and sleep behavior.5 Sleep architecture refers to the pattern of nighttime sleep recorded from physiologic measures of brain waves, eye movements, and muscle tone called polysomnography (PSG). Sleep consists of two basic states: rapid eye movement (REM) sleep and non–rapid eye movement (NREM) sleep (see eFig. 8-1 on the website for this chapter). During sleep, the body cycles between NREM and REM sleep. Once asleep, a person goes through four to six NREM and REM sleep cycles.7 In healthy adults the largest percentage of total sleep time, approximately 75% to 80%, is spent in NREM sleep. NREM sleep is subdivided into three stages:8 Stage 1 occurs in the beginning of sleep, with slow eye movements, and is a transition phase from wakefulness to sleep. During this period the person can be easily awakened. Stage 2 encompasses most of the night’s sleep. The heart rate slows down, and the body temperature drops. This stage is associated with specific electroencephalographic (EEG) wave forms that help to maintain sleep. Stage 3 is deep sleep or slow-wave sleep (SWS). This stage is associated with large EEG wave forms, called delta waves, which are used as a measure of sleep intensity. SWS sleep declines as people age such that most adults over 60 years of age have little NREM stage 3 sleep. Insufficient sleep and sleep disorders are associated with changes in body function (Fig. 8-3) and health problems (Table 8-2). Impaired cognitive function and impaired performance on simple behavioral tasks occur within 24 hours of sleep loss. The effects of sleep loss are cumulative. Individuals who report less than 6 hours of sleep a night have a higher body mass index (BMI) and are more likely to be obese. The risk for developing glucose intolerance and diabetes is increased in individuals with a history of insufficient sleep.9,10 Chronic loss of sleep places older adults at risk for depression, impaired daytime functioning, social isolation, and overall reduction in quality of life. In patients with chronic illnesses, especially cardiovascular disease and stroke, insomnia and sleep-disordered breathing are associated with increased morbidity and mortality.11,12 TABLE 8-2 RELATIONSHIP OF SLEEP DISTURBANCES TO DISEASES AND DISORDERS • Linked with heart disease (hypertension, stroke, coronary artery disease, dysrhythmias). • Results in impaired glucose control similar to that which occurs in type 2 diabetes.
Sleep and Sleep Disorders
Sleep
Dyssomnias
Parasomnias
 hours on workdays and
hours on workdays and  hours on non-workdays. Seventy percent of adults report habitually sleeping less than 7 hours a night.
hours on non-workdays. Seventy percent of adults report habitually sleeping less than 7 hours a night.
Name _____________________________ ID# ____________ Date _____________ Age ______
INSTRUCTIONS
The following questions relate to your usual sleep habits during the past month only. Your answers should indicate the most accurate reply for the majority of days and nights in the past month. Please answer all questions.
1. During the past month, what time have you usually gone to bed at night?
USUAL BED TIME ___________
2. During the past month, how long (in minutes) has it usually taken you to fall asleep each night?
NUMBER OF MINUTES___________
3. During the past month, what time have you usually gotten up in the morning?
USUAL GETTING UP TIME_____________________
4. During the past month, how many hours of actual sleep did you get at night? (This may be different than the number of hours you spent in bed.)
HOURS OF SLEEP PER NIGHT________________
For each of the remaining questions, check the one best response. Please answer all questions.
5. During the past month, how often have you had trouble sleeping because you . . .
a) Cannot get to sleep within 30 minutes
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
b) Wake up in the middle of the night or early morning
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
c) Have to get up to use the bathroom
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
d) Cannot breathe comfortably
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
e) Cough or snore loudly
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
f) Feel too cold
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
g) Feel too hot
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
h) Had bad dreams
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
i) Have pain
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
j) Other reason(s), please describe______________________________________________________________________________________________________
__________________________________________________________________________________________________________________________________
6. How often during the past month have you had trouble sleeping because of this?
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
7. During the past month, how would you rate your sleep quality overall?
Very good _____
Fairly good _____
Fairly bad _____
Very bad _____
8. During the past month, how often have you taken medicine to help you sleep (prescribed or over the counter)?
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
9. During the past month, how often have you had trouble staying awake while driving, eating meals, or engaging in social activity?
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
10. During the past month, how much of a problem has it been for you to keep up enough enthusiasm to get things done?
No problem at all __________
Only a very slight problem __________
Somewhat of a problem __________
A very big problem __________
11. Do you have a bed partner or roommate?
No bed partner or roommate __________
Partner/roommate in other room __________
Partner in same room, but not same bed __________
Partner in same bed __________
12. If you have a roommate or bed partner, ask him/her how often in the past month you have had . . .
a) Loud snoring
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
b) Long pauses between breaths while asleep
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
c) Legs twitching or jerking while you sleep
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
d) Episodes of disorientation or confusion during sleep
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
e) Other restlessness while you sleep; please describe ___________________________________________________________________________________
Not during the past month_____
Less than once a week_____
Once or twice a week_____
Three or more times a week_____
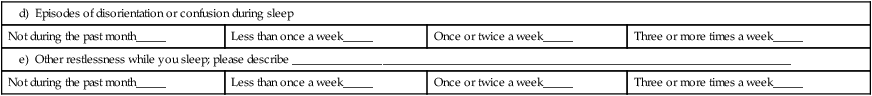
Name: ______________________________
Date: ________________________
For each question below, please circle the number corresponding to your response.
1. Please rate the current (i.e., last month) SEVERITY of your insomnia problem(s).
None
Mild
Moderate
Severe
Very
a) Difficulty falling asleep
0
1
2
3
4
b) Difficulty staying asleep
0
1
2
3
4
c) Problem waking up too early
0
1
2
3
4
2. How SATISFIED/dissatisfied are you with your current sleep pattern?
Very Satisfied
Satisfied
Neutral
Dissatisfied
Very Dissatisfied
0
1
2
3
4
3. To what extent do you consider your sleep problem to INTERFERE with your daily functioning (e.g., daytime fatigue, ability to function at work/daily chores, concentration, memory, mood, etc.)?
Not At All Interfering
A Little Interfering
Somewhat Interfering
Much Interfering
Very Much Interfering
0
1
2
3
4
4. How NOTICEABLE to others do you think your sleeping problem is in terms of impairing the quality of your life?
Not At All Noticeable
A Little Noticeable
Somewhat Noticeable
Much Noticeable
Very Much Noticeable
0
1
2
3
4
5. How WORRIED/distressed are you about your current sleep problem?
Not At All
A Little
Somewhat
Much
Very Much
0
1
2
3
4
Guidelines for Scoring/Interpretation
Add scores for all seven items (1a + 1b + 1c + 2 + 3 + 4 + 5) = _____
Total score ranges from 0-28.
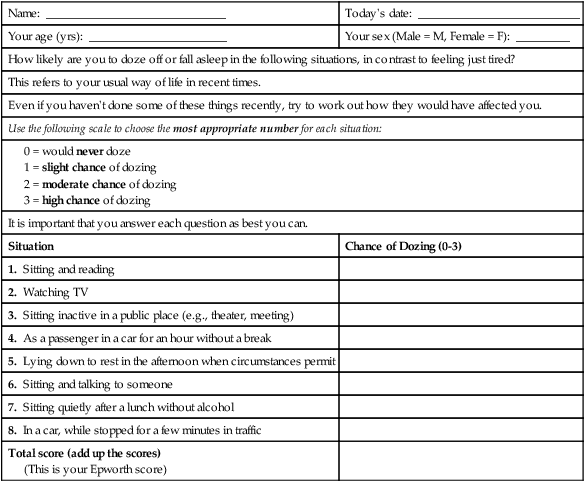
Name: ______________________________
Today’s date: ___________________________
Your age (yrs): _______________________
Your sex (Male = M, Female = F): _________
How likely are you to doze off or fall asleep in the following situations, in contrast to feeling just tired?
This refers to your usual way of life in recent times.
Even if you haven’t done some of these things recently, try to work out how they would have affected you.
Use the following scale to choose the most appropriate number for each situation:
It is important that you answer each question as best you can.
Situation
Chance of Dozing (0-3)
1. Sitting and reading
2. Watching TV
3. Sitting inactive in a public place (e.g., theater, meeting)
4. As a passenger in a car for an hour without a break
5. Lying down to rest in the afternoon when circumstances permit
6. Sitting and talking to someone
7. Sitting quietly after a lunch without alcohol
8. In a car, while stopped for a few minutes in traffic
Total score (add up the scores)
(This is your Epworth score)
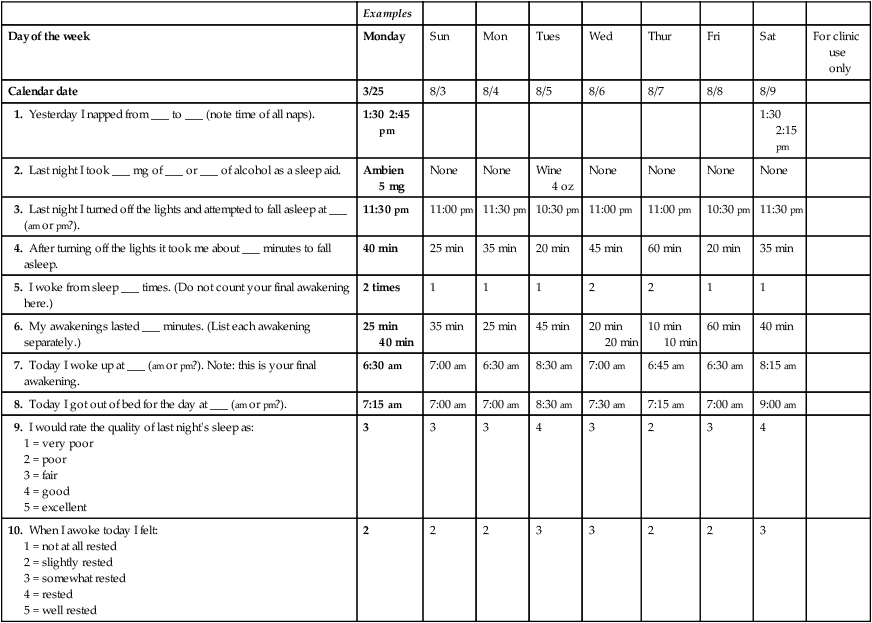
Examples
Day of the week
Monday
Sun
Mon
Tues
Wed
Thur
Fri
Sat
For clinic use only
Calendar date
3/25
8/3
8/4
8/5
8/6
8/7
8/8
8/9
1. Yesterday I napped from ___ to ___ (note time of all naps).
1:30 2:45 pm
1:30 2:15 pm
2. Last night I took ___ mg of ___ or ___ of alcohol as a sleep aid.
Ambien 5 mg
None
None
Wine 4 oz
None
None
None
None
3. Last night I turned off the lights and attempted to fall asleep at ___ (am or pm?).
11:30 pm
11:00 pm
11:30 pm
10:30 pm
11:00 pm
11:00 pm
10:30 pm
11:30 pm
4. After turning off the lights it took me about ___ minutes to fall asleep.
40 min
25 min
35 min
20 min
45 min
60 min
20 min
35 min
5. I woke from sleep ___ times. (Do not count your final awakening here.)
2 times
1
1
1
2
2
1
1
6. My awakenings lasted ___ minutes. (List each awakening separately.)
25 min
40 min
35 min
25 min
45 min
20 min
20 min
10 min
10 min
60 min
40 min
7. Today I woke up at ___ (am or pm?). Note: this is your final awakening.
6:30 am
7:00 am
6:30 am
8:30 am
7:00 am
6:45 am
6:30 am
8:15 am
8. Today I got out of bed for the day at ___ (am or pm?).
7:15 am
7:00 am
7:00 am
8:30 am
7:30 am
7:15 am
7:00 am
9:00 am
9. I would rate the quality of last night’s sleep as:
1 = very poor
2 = poor
3 = fair
4 = good
5 = excellent
3
3
3
4
3
2
3
4
10. When I awoke today I felt:
1 = not at all rested
2 = slightly rested
3 = somewhat rested
4 = rested
5 = well rested
2
2
2
3
3
2
2
3

Physiologic Sleep Mechanisms
Sleep-Wake Cycle
Wake Behavior.
Sleep Behavior.
Circadian Rhythms.
Sleep Architecture
NREM Sleep.
Insufficient Sleep and Sleep Disorders
Disease or Disorder
Sleep Disturbance
Respiratory
Asthma
Chronic obstructive pulmonary disease (COPD)
Obstructive sleep apnea
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

Sleep and Sleep Disorders
Get Clinical Tree app for offline access
